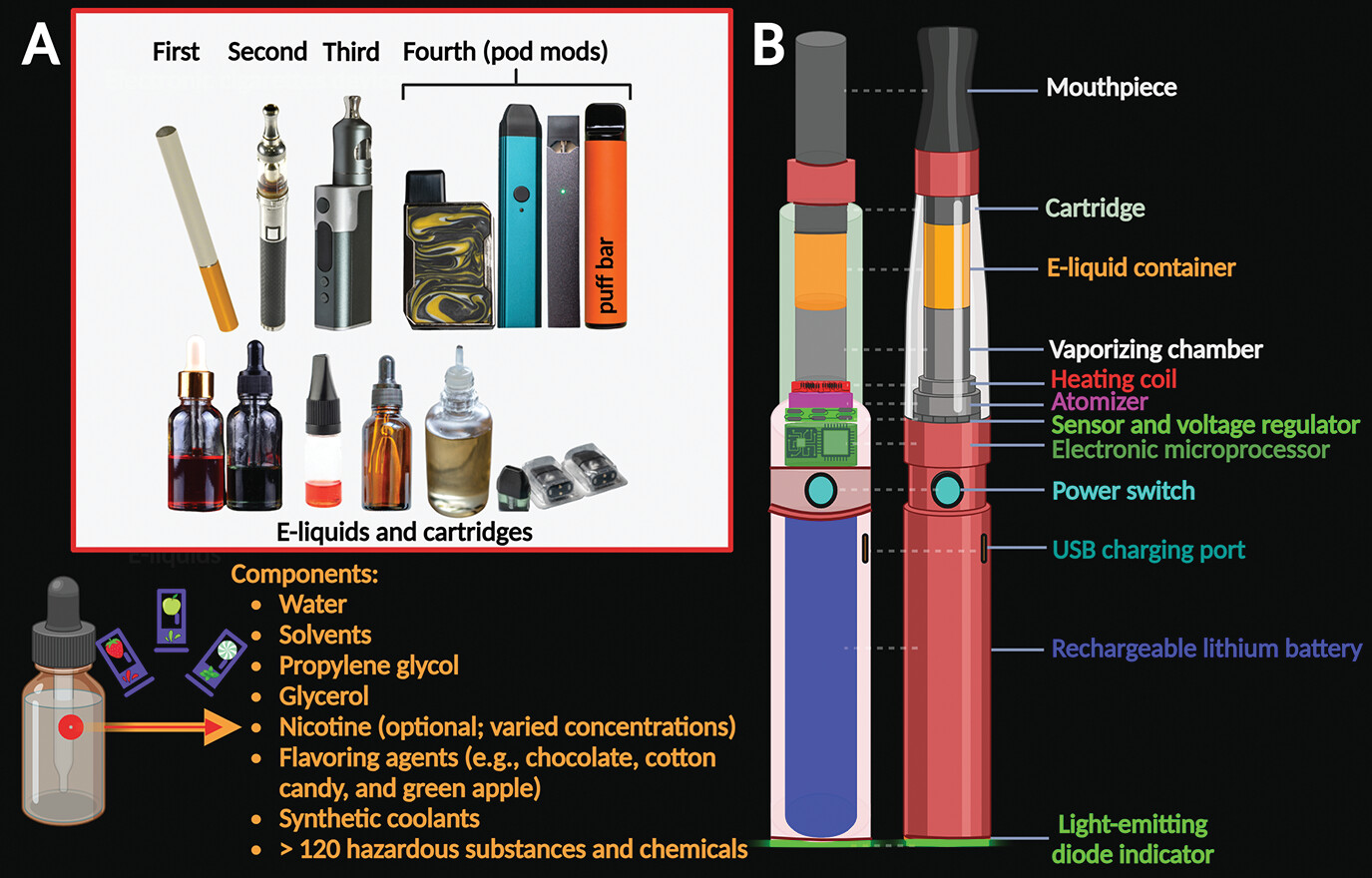
E-cigarettes (ECs), also known as vape pens, e-cigars, vaping devices, e-hookahs, mods, vapes, tank systems, electronic nicotine delivery systems (ENDS), and puff bars (fourth-generation ECs), are battery-operated electronic devices used to inhale a heat-generated aerosol from an e-liquid source (
2,
5,
11). E-liquids contain basic ingredients, including water, propylene glycol, glycerol, optional nicotine (available at various concentrations), and flavoring agents (e.g., chocolate, cotton candy, and green apple) (
4). E-liquids in disposable puff bars contain over 120 different substances, including cytotoxic chemicals (
2). Refill solutions, e-liquid cartridges, and emission vapors (i.e., aerosol mix of small particles in the air) contain many other substances and hazardous chemicals, including solvents, volatile organic compounds (e.g., benzene and formaldehyde), acrolein, acids, and synthetic coolants (
2,
4,
8,
11–
14). ECs can also be used to deliver marijuana. Using ECs is commonly known as “vaping” (
15) (
Figure 1).
ECs have several components, including a cartridge or “pod,” where the liquid solution containing nicotine, flavoring substances, and other chemicals is vaporized upon activation of an electronic heating element in the device that is triggered by inhalation (
5). The heating element is powered by a rechargeable lithium battery (
15). The consumer can choose the nicotine concentration of the e-liquid that is loaded into the EC cartridge (
5) (
Figure 1). The technology of pod mods allows manufacturers to combine acid mixtures and other dangerous chemicals with nicotine salts or crystals to elevate the nicotine concentrations of their products (
2,
3). This design allows delivery of higher drug doses via relatively inconspicuous devices with reduced electrical power that closely resemble electronic USB drives (
2,
3,
16,
17). Popular pods contain approximately 59.2–66.7 mg/mL of nicotine, which is comparable to one pack of 20 conventional cigarettes (
3,
15,
18). Once the cartridge or pod is installed in the EC device, the user then inhales the vaporized products of the e-liquid into the lungs, and the residues are exhaled into the air (
5,
15).
It has been suggested, incorrectly, that ECs are less harmful than conventional cigarettes (
19). ECs are promoted as containing fewer chemicals, having lower levels of carcinogens, and producing fewer toxic agents than conventional cigarettes (
19,
20). However, they are not emission-free devices, and their aerosol emissions are not harmless (
5,
6,
11,
20). Bystanders to exhaled vaping fumes can be exposed to toxic aerosols and carcinogenic agents (e.g., acrolein, benzene, diacetyl, and formaldehyde) through second-hand or third-hand exposure (
6,
11,
21). Elements from second-hand EC vapor increase particulate matter in the air, which can be harmful and lead to preclinical forms of cardiovascular, pulmonary, and other diseases (
6,
7,
11,
22,
23). Third-hand exposure (through residual chemicals left on surfaces, skin, hair, and clothing following vaping) plays a role in the overall exposure of children to nicotine and a variety of toxicants (
24,
25).
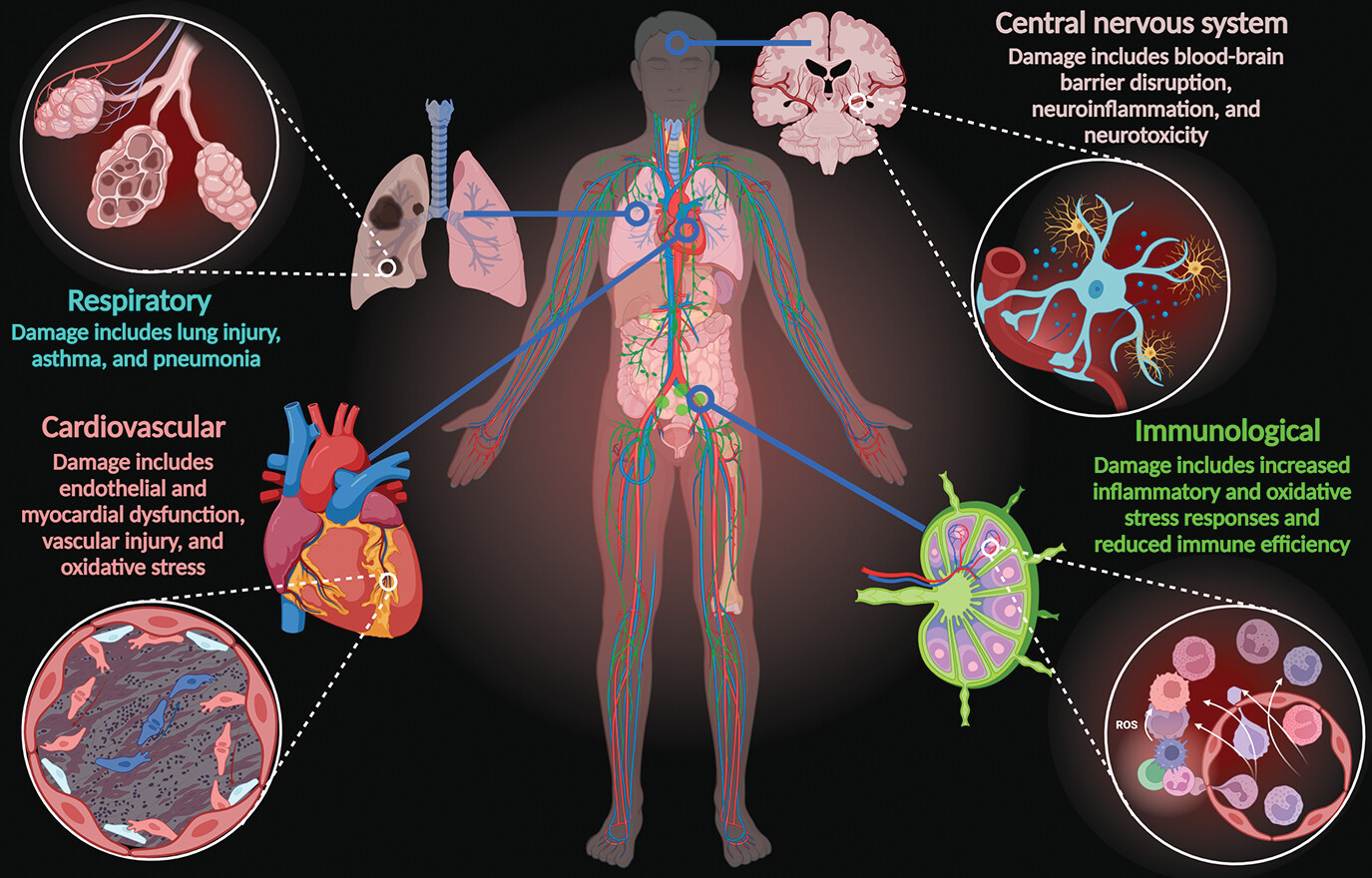
Vaping causes serious damage throughout the human body, including organs in the cardiovascular, central nervous, immunological, and respiratory systems. This damage is primarily due to the deleterious effects of toxic compounds that exacerbate oxidative stress responses and inflammatory reactions, causing endothelial dysfunction, cellular senescence, and subsequent disease sequelae (
2,
6–
10) (
Figure 2). The nicotine and nonnicotinic agents in ECs, including hazardous neurotoxic elements (i.e., aluminum, arsenic, chromium, cadmium, copper, lead, manganese, nickel, tin, and zinc) and other by-products, pose serious threats to the brain (
8,
13,
26,
27). To date, only a few studies have investigated the effects of these compounds on neurological function, mostly in animal models (
8,
28).
According to the Centers for Disease Control and Prevention, ECs “have the potential to benefit adults who smoke and who are not pregnant if used as a complete substitute for regular cigarettes and other smoked tobacco products” (
29). However, use of ECs may increase the risk of future cigarette smoking among adolescents and young adults (
30). The use of any form of tobacco product (smoked, smokeless, or electronic) by youths is considered unsafe (
15). The U.S. Surgeon General has concluded that exposure to nicotine during adolescence can cause addiction and impair the developing adolescent brain (
11).
The use of ECs has skyrocketed among U.S. adolescents and young adults since 2014 (
31,
32). In 2018, usage increased 77.8% over the previous year, the largest surge of youth tobacco consumption ever recorded by the Centers for Disease Control and Prevention (
33). Most adolescents and young adult users do not know that ECs may contain higher concentrations of nicotine than conventional cigarettes (
15,
34). Similar trends have been reported among youth in countries outside the United States (
35–
38). However, the United States dominates the global vaping market. By 2022, over 2.6 million young Americans reported current use of ECs (
39). Global market research reports indicated that ECs generated $22.45 billion in U.S. dollars in 2022 and a compounded annual growth of 30.6% was projected from 2023 to 2030 (
40).
The increased popularity and use of ECs seems to be linked (in part) to novelty and the alluring flavors of various e-liquid options (
41). The flavoring chemicals and additives of ECs are largely unregulated (
8,
14,
21). In 2020, the Food and Drug Administration enacted a ban on flavored EC pods in an effort to reduce accelerated use among young consumers (
42). A technicality in the ban, which did not include “disposable products” (i.e., puffs ECs), has allowed young consumers and suppliers to keep these devices in high demand (
2,
43,
44). At present, several thousand flavoring options and hundreds of brands are available (
14,
26). However, the explosion in EC use also suggests that users may be experiencing dependency to both smoking and vaping (
12,
45).
Studies in Animal Models and Humans
Subchronic exposure to e-liquid (without nicotine) hindered growth and development of nematodes, caused abnormal general neuromotor behavior, and impaired advanced learning and memory (
46). A study in mice indicated that chronic exposure (2 months) to vaporized elements from ECs resulted in toxic metal aggregation in the central nervous system, potentially leading to endogenous dysregulation, including metal dyshomeostasis and neurotoxicity (
47). Another study in mice compared the neurological effects of short-term exposure to EC vapor and smoke from conventional cigarettes over 14 days. The EC-vapor-exposed group showed neurotoxicity leading to neuroinflammatory responses (confirmed via tumor necrosis factor alpha expression in brain tissue), and comparable cognitive and memory impairments were observed in both groups. In addition, the EC group showed longer latencies to find food rewards, with a lack of improvement in spatial memory learning (
48). Taken together, these results link EC-induced neuroinflammation to deleterious alterations in cognitive and memory function (
46–
48).
It is well established that nicotine exposure during adolescence alters the structure and function of the developing brain, impairing several cognitive processes and increasing rates of mood disorders and addiction (
11). Deterioration in cognitive functions (e.g., attention, impulse control, memory, and reasoning) is linked to smoking conventional cigarettes during adolescence and early adulthood, increasing the risk of long-lasting mental health concerns (
49,
50). A recent cross-sectional study reported that EC use was associated with subjective cognitive deficits in U.S. adults (
51).
The toxicity of several commercially available EC refills across a range of concentrations (0.001%–1%) was analyzed with in vitro experiments using stem cells from mice and humans. Some samples had no cytotoxic effects, and others displayed high levels of cytotoxicity. Interestingly, cytotoxicity was not linked to nicotine concentrations but was linked to the amount and concentration of flavoring toxicants (
52). Popular flavors, such as caramel and butterscotch, potentiated levels of cytotoxic effects; thus, commonly known flavoring chemicals should not be assumed to be harmless (
52). Similar results have been reported in other studies (
16,
53).
Flavoring Additives and Other Toxicants
Menthol was introduced to conventional cigarettes in the 1950s and is also widely found in ECs (
8,
54). This popular flavoring agent increases nicotine bioavailability (
54), enhances nicotine reward-related behavior, and potentiates nicotine actions in midbrain dopaminergic neurons (
55). Menthol also promotes smoking initiation among youths (
56). Conventional menthol cigarette smokers are twice as likely to become lifelong smokers compared with conventional nonmenthol cigarette smokers (
57). The evidence suggests that menthol is a highly reinforcing sensory cue when paired with nicotine and promotes addiction.
Farnesol, a sesquiterpene alcohol found in many foods, such as peaches and vegetables, is commonly added to ECs as a flavor enhancer (e.g., green apple) (
8,
58). This additive promotes reward-related behavior (via nicotinic acetylcholine receptors), amplifying the effects of nicotine on dopaminergic neurons in the ventral tegmental area and altering the function of dopamine and GABA neurons in the midbrain (
58,
59). Many EC constituents and flavoring agents chemically decompose during vaporization, which transforms them into different toxicants, and variations in heating temperature contribute to this process. Effects of these substances are unknown (
4,
8,
60).
A recent study investigated the long-term impact of maternal exposure to EC vapor on blood-brain barrier integrity and behavioral outcomes in postnatal mice. Vapor exposure led to cellular and molecular alterations, which are potentially associated with long-term neurotoxicity and cerebrovascular diseases (
61). These changes resulted in postnatal blood-brain barrier disruptions and neurodevelopmental and behavioral impairments (
61). The investigators concluded that maternal exposure to EC vapors was related to motor disabilities and learning and memory dysfunction among the offspring that persist into adolescence and adulthood (
61). These findings are relevant because the use of ECs among pregnant women (both smokers and nonsmokers) has increased since the introduction of ECs to the U.S. market (
62–
64).
Another in vivo study in mice demonstrated that nonnicotinic toxicants (e.g., volatile organic compounds, acetaldehyde, acrolein, and formaldehyde) of EC emissions appeared to abruptly alter the biological and molecular integrity of the blood-brain barrier by reducing gene expression of occludin, a protein essential for stabilizing the blood-brain barrier. Changes were observed within tight junctions of blood vessels in the frontal cortex, and paracellular permeability was increased in thalamic nuclei (
27). These alterations contributed to neurovascular dysfunction that promoted neuroinflammation, resulting in cognitive deficits (
27,
60).
Endothelial cell-derived microvesicles are both biomarkers and mediators of vascular health and pathogenesis in humans (
65). Activation of endothelial cell-derived microvesicles in EC users decreased activation of nitric oxide synthase in microvascular endothelial cells and production of nitric oxide in the brain (
9). These changes caused further biomolecular and cellular alterations in the blood-brain barrier, resulting in vascular dysregulation in the brain and increased risk of cerebrovascular diseases (
9,
66).
Conclusions
ECs do not seem to be a safer alternative to conventional cigarettes during smoking-cessation therapy. They appear to share similar chemical profiles (nicotine, nonnicotinic toxicants, and other emitted substances). Therefore, users may experience equal or possibly higher pathophysiological alterations, resulting in many health issues and higher risks for certain chronic diseases (e.g., asthma and cancer), as well as neurological conditions (e.g., addiction, stroke, cognitive dysfunction, and neurodevelopmental disorders). Bystanders exposed to second-hand or third-hand EC vapors also appear to be at higher risk for these diseases.
Furthermore, the nonnicotinic constituents in ECs potentiate epigenetic alterations, cellular dysfunction, neuroinflammation, oxidative stress, neurotransmitter dysregulation, and other abnormalities. ECs without nicotine also appear to have substantial detrimental effects on vital central nervous system regulatory components, such as the blood-brain barrier. The added flavorings, solvents, acids, synthetic coolants, volatile organic compounds, and other toxicants, including aerosolized by-products and metabolites of e-liquids, warrant attention, because flavorings seem to have increased the popularity of ECs among adolescents and young adults. Popularity of ECs has also increased among pregnant women, nonsmokers, and former conventional cigarette smokers.
Additional studies are needed to fully understand effects of the chemical constituents (especially nonnicotinic compounds) in e-liquids and their vaporized by-products, which are physiologically and pharmacokinetically uncharacterized. Flavoring substances are largely unregulated based on their clearance for ingestion. However, they are not intended for inhalation, and the exposure of respiratory and nervous tissue to these substances has not been properly studied. The popularity and increasing usage of e-liquids raise major concerns for public health.