Neurobiological, neurochemical, and neuroanatomical changes after traumatic brain injury (TBI) often manifest in physical, cognitive, and psychological sequelae. Of these, symptoms of mental disorders are underrecognized and contribute to poor outcomes (
1–
4). Anxiety disorders and posttraumatic stress disorder (PTSD) post-TBI have received relatively less empirical investigation compared with depression (
5). The development of these disorders is not surprising, given the often traumatic nature and associated neurological changes post-TBI (
6). For example, one study reported that 44.1% of participants developed an anxiety disorder during the year immediately post-TBI (
5). A meta-analysis of PTSD post-TBI reported pooled incidence rates of 15.7% in the civilian population and 36.8% in the military population (
7). Both disorders are associated with poorer recovery from TBI, yet there is a scarcity of evidence-based guidelines for treating neuropsychiatric disorders post-TBI (
8).
The extant literature provides little guidance about standard pharmacotherapy recommendations with demonstrated efficacy for anxiety and PTSD post-TBI. This can be problematic, because symptom overlap between TBI, anxiety disorders, and PTSD (e.g., irritability, difficulty sleeping, anger, impulsivity, restlessness, and alterations in mood, and cognition) could lead to iatrogenic effects, polypharmacy, off-label prescribing practices, and side effects (
9,
10).
METHODS
Study Design and Data Source
We conducted a retrospective cohort study using data from the OptumLabs Data Warehouse (OLDW), which includes deidentified claims data for commercially insured and Medicare Advantage enrollees. The database contains longitudinal health information on enrollees, representing a diverse mixture of age, race-ethnicity, and geographical regions across the United States. It is representative of the general commercial Medicare Advantage market in the geographic area where it operates (
13). According to OLDW data, enrollees have comprehensive, full insurance coverage for physician, hospital, and prescription drug services. In the OLDW, anyone ≥89 years old is assigned an age of 89 years to maintain compliance with the Health Insurance Portability and Accountability Act of 1996. This study involved analyzing pre-existing, deidentified data and was determined exempt from institutional review board approval by the University of Maryland, Baltimore.
Study Participants
Participants included enrollees aged ≥18 years who were diagnosed as having TBI between January 1, 2009, and June 30, 2012, and who maintained continuous enrollment in medical and pharmacy benefits for 12 months before TBI and 24 months post-TBI (i.e., 36 months total). We defined TBI on the basis of the Centers for Disease Control and Prevention case definition (
14,
15), which includes International Classification of Diseases, ninth revision, Clinical Modification (ICD-9-CM) codes 800.xx, 801.xx, 803.xx–804.xx, 850.xx–854.1x, 950.1–950.3, and 959.01. We searched inpatient and outpatient claims for the presence of TBI defined as any of the ICD-9-CM codes in any position on the claim.
We defined the diagnosis of anxiety using ICD-9-CM codes 300.00–300.02, 300.09, 300.21, and 300.22. We defined PTSD using ICD-9-CM code 309.81. We searched for any of these codes in any position on an inpatient or outpatient post-TBI claim. Individuals who were diagnosed as having both anxiety and PTSD were excluded from analyses. We did not exclude individuals with pre-existing anxiety, PTSD, or any other psychological disorder for our primary analyses.
To investigate the treatment of anxiety and PTSD post-TBI outside of the treatment of other neuropsychiatric disorders, we conducted additional analyses in restricted cohorts. We created cohorts of individuals diagnosed as having anxiety or PTSD post-TBI who had not been previously diagnosed as having bipolar and manic disorders (ICD-9-CM 296.0x, 296.1x, 296.4x−296.7x, 296.80, 296.81, and 296.89), schizophrenia and schizoaffective disorders (ICD-9-CM 295.0x−295.4x, 295.6x, 295.7x, and 295.9x), other psychoses (ICD-9-CM 297.1x, 298.0x−298.4x, 298.8x, and 298.9x), other anxiety disorders (ICD-9-CM 300.1x and 300.3x−300.8x), or substance use disorders (ICD-9-CM 292.xx, 304.x, and 305.1x−305.9x). For this restricted cohort, we also excluded individuals diagnosed with depression (ICD-9-CM 296.20–296.25, 296.30–296.35, 300.4, and 311) at any time during the study period.
Treatment
An expert panel with representation from the fields of psychiatry and pharmacy helped identify medications indicated to treat anxiety and PTSD. These included anticonvulsants, antidepressants, antipsychotics, anxiolytics, mood stabilizers, and sedative hypnotics. (For a complete listing of medications, see the
online supplement.) To identify receipt of psychotherapy, we searched for any of the following Current Procedural Terminology codes: 90791, 90792, 90832, 90834, 90836–90838, 90847, 90853, and 96150–96155. Treatment variables were recorded monthly after patients received a post-TBI diagnosis of anxiety or PTSD.
Demographic and clinical characteristics were obtained from the OLDW files. Identification of comorbid illnesses was based on the presence of ICD-9-CM codes on any inpatient or outpatient claim. Any comorbidity identified during the 12 months before the TBI was considered present at baseline.
Although information on the severity of TBI is lacking in administrative claims data, we previously used the setting of TBI diagnosis as a proxy for TBI severity (
16). In the present study, we used place of service codes for office clinic visits (codes 11, 22, 25, 71, 72), inpatient hospital stays (code 21), and emergency department visits (code 23) to identify the site of care at TBI diagnosis. Diagnosis in an inpatient hospital setting was considered suggestive of more severe TBI.
Statistical Analysis
We tested differences in distributions of variables between the anxiety and PTSD cohorts using chi-square goodness of fit and the Student’s t test. Individuals could receive a diagnosis of anxiety or PTSD at any time during the 24 months post-TBI; thus, individuals had differing amounts of follow-up time postdiagnosis. Analyses of treatment patterns were restricted to the first 12 months after individuals received a diagnosis of anxiety or PTSD, so that most individuals contributed to all months of follow-up. We assessed the 12-month average prevalence of medications and psychotherapy. We plotted results for the most commonly used medications on a bar graph by cohort membership (whole or restricted anxiety or PTSD).
To test the significance of group, time, and Group × Time trends for the most commonly used medications, we used Poisson regression with a log link. We conducted the analyses at the group level, and they were not adjusted for covariates. Rate ratios and 95% confidence intervals are reported. We conducted all analyses using STATA/MP, version 15 (StataCorp).
RESULTS
We identified 207,354 beneficiaries who were diagnosed as having a TBI and who met inclusion criteria. Of these, 42,475 (20.5%) and 1,232 (0.6%) were diagnosed as having an anxiety disorder or PTSD post-TBI, respectively.
Characteristics of the Sample
Individuals diagnosed as having anxiety post-TBI were older than those diagnosed as having PTSD (mean age=56.3 years [SD=20.0] versus 46.4 years [SD=16.8]; t=20.6, df=43,706, p<0.001) and were more likely to be female (69.1% versus 58.0%; χ
2=68.6, df=1, p<0.001) (Table
1). They were also less likely to receive a diagnosis in the inpatient setting (12.9% versus 14.1%; χ
2=63.2, df=4, p<0.001). Individuals diagnosed as having anxiety had a lower prevalence of psychological comorbidities than those diagnosed as having PTSD. For example, they were less likely to be diagnosed as having substance dependence disorders (28.9% versus 32.4%; χ
2=6.8, df=1, p=0.01) or bipolar disorder (10.0% versus 20.3%; χ
2=135.3, df=1, p<0.001). Among individuals diagnosed as having anxiety, 39.3% also received an anxiety diagnosis pre-TBI. Of enrollees diagnosed as having PTSD, 28.1% also received a PTSD diagnosis pre-TBI.
Receipt of Indicated Pharmacotherapy
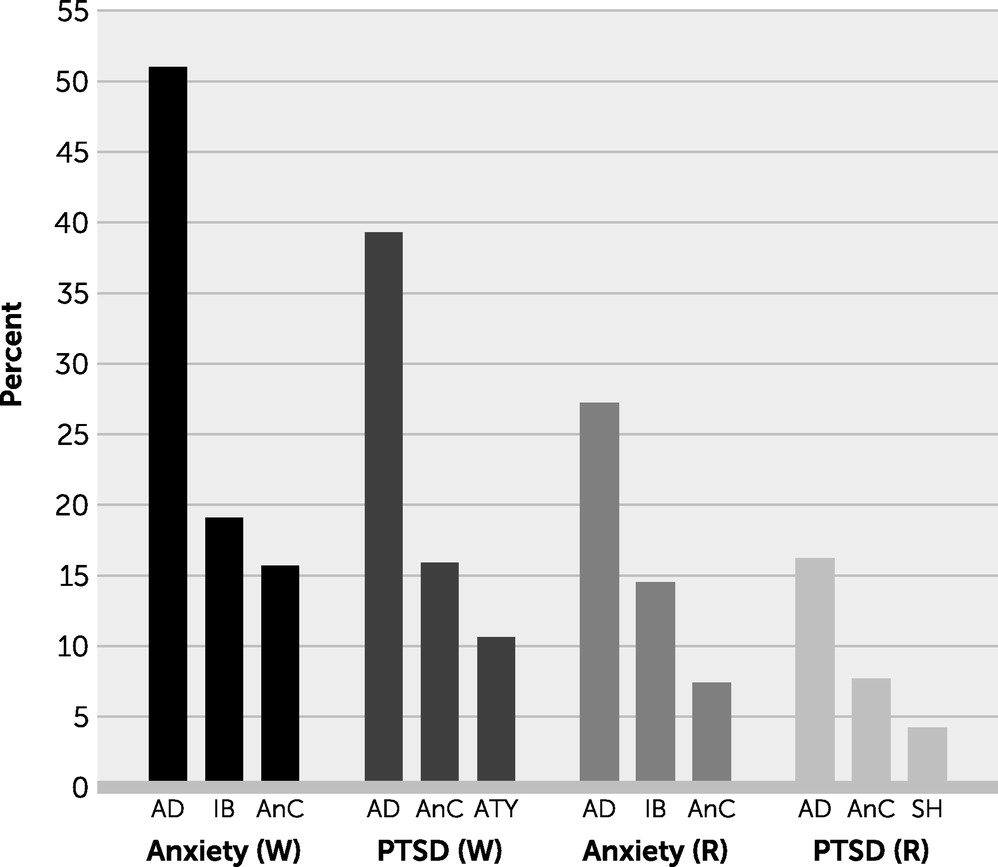
Most individuals who had been diagnosed as having anxiety received indicated pharmacotherapy at least once pre-TBI (58.4%) and post-TBI (76.2%) TBI. Similarly, most individuals who had been diagnosed as having PTSD received indicated pharmacotherapy at least once pre-TBI (53.7%) and post-TBI (75.2%). Among individuals who received pharmacotherapy after an anxiety diagnosis, the most commonly prescribed classes of psychotropic medications were antidepressants (51.0%), intermediate-acting benzodiazepines (19.1%), and anticonvulsants (15.7%) (
Figure 1). Among enrollees diagnosed as having PTSD, antidepressants (39.3%), anticonvulsants (15.9%), and atypical antipsychotics (10.6%) were the most commonly prescribed classes of psychotropic medications (
Figure 1).
In our regression models, compared with individuals who were diagnosed as having PTSD post-TBI, those who were diagnosed as having anxiety were more likely to receive antidepressants (rate ratio=1.19; 95% CI=1.13, 1.26) (Table
2). Conversely, the anxiety group was less likely to receive anticonvulsants than the PTSD group (rate ratio=0.87; 95% CI=0.79, 0.95).
Receipt of Psychotherapy
Few individuals who were diagnosed as having anxiety received psychotherapy at least once pre-TBI (5.8%) and post-TBI (19.1%). Among enrollees diagnosed as having PTSD, 11.2% received psychotherapy pre-TBI, and 36.0% received psychotherapy post-TBI. In our adjusted regression models, compared with individuals diagnosed as having PTSD post-TBI, those diagnosed as having anxiety were 66% less likely to receive psychotherapy (rate ratio=0.34; 95% CI=0.31, 0.38) (Table
2).
Restricted Cohorts
Among the 42,475 individuals diagnosed as having anxiety post-TBI, 11,076 (26.1%) were not diagnosed as having depressive disorder, bipolar disorder, schizophrenia, or substance use disorder during the study period. Of these, 27.8% had a pre-existing anxiety disorder diagnosis. Among the 1,232 individuals diagnosed as having PTSD post-TBI, 294 (23.9%) were not diagnosed with the aforementioned neuropsychiatric disorders during the study period. Of these, 16.3% had been given a diagnosis of a pre-existing anxiety disorder.
Receipt of Indicated Pharmacotherapy in the Restricted Cohorts
Among individuals diagnosed as having anxiety, but no additional neuropsychiatric disorders, 32.5% received indicated pharmacotherapy at least once pre-TBI, and 52.5% received the indicated pharmacotherapy at least once post-TBI. Of those diagnosed as having PTSD, 23.8% received the indicated pharmacotherapy pre-TBI, and 51.7% received the indicated pharmacotherapy post-TBI. Among individuals diagnosed as having anxiety, the most commonly prescribed classes of psychotropic medications as determined by average 12-month prevalence were antidepressants (27.2%), intermediate-acting benzodiazepines (14.5%), and anticonvulsants (7.4%) (
Figure 1). Among enrollees who were diagnosed as having PTSD but no additional neuropsychiatric disorders, antidepressants (16.2%), anticonvulsants (7.7%), and sedative hypnotics (4.2%) were the most commonly prescribed classes of psychotropic medications (
Figure 1).
In our regression models, compared with individuals who had been diagnosed as having PTSD post-TBI, those who had been diagnosed as having anxiety were 53% more likely to receive antidepressants (rate ratio=1.53; 95% CI=1.28, 1.82) (Table
2). The anxiety group was less likely to receive anticonvulsants than the PTSD group (rate ratio=0.77; 95% CI=0.60, 1.00).
Receipt of Psychotherapy in the Restricted Sample
Few individuals who had been diagnosed as having anxiety, but no additional neuropsychiatric disorders, received psychotherapy at least once pre-TBI (2.0%) and post-TBI (8.4%). Of enrollees diagnosed as having PTSD, but no additional neuropsychiatric disorders, few received psychotherapy pre-TBI (4.8%) and post-TBI (27.9%).
In our adjusted regression models, compared with individuals diagnosed as having PTSD post-TBI, those diagnosed as having anxiety were 75.0% less likely to receive psychotherapy (rate ratio=0.25; 95% CI=0.19, 0.31).
DISCUSSION
Our objective was to highlight differences in prevalence and patterns of psychotropic medication use and psychotherapy among individuals diagnosed as having anxiety or PTSD post-TBI. More than 70.0% received at least one pharmacological treatment indicated for anxiety or PTSD post-TBI in the whole cohort. Conversely, less than half participated in at least one psychotherapy appointment post-TBI. This aligns with national trends of medication being more common than psychotherapy (
17).
Previous studies examined the broad utilization of psychotropic medication and classes or among individuals diagnosed as having a singular disorder (i.e., anxiety or PTSD); however, to our knowledge this is the first study to provide comparisons between treatments for anxiety and PTSD (
18,
19). Psychotropic medication use post-TBI was higher in the anxiety cohort than in the PTSD cohort. As well, there was an increase in overall prevalence of psychotropic medication use in both cohorts in the post-TBI period. Despite this observed increase, past research suggests that individuals diagnosed as having anxiety or PTSD are less likely to receive indicated pharmacological treatment compared with similar individuals who had not received a diagnosis of TBI (
20).
Individuals diagnosed as having anxiety post-TBI were more likely to receive antidepressants than those diagnosed as having PTSD, even though the prevalence of depression was similar between groups. This difference in receipt of antidepressants should be examined in future research.
Intermediate-acting benzodiazepines were the second most commonly prescribed medication class (19%) for those diagnosed as having anxiety post-TBI. Use of benzodiazepines observed in our sample is more than double that observed in previous studies (
21–
23). The common use of benzodiazepines is concerning, because they are no longer considered first-line treatments for anxiety (
24). Further, strong recommendations exist against the use of benzodiazepines post-TBI because of concerns about cognitive and motor side effects and addictive properties (
25,
26).
To our knowledge, this is the first study to examine psychotherapy participation rates in a national sample of individuals diagnosed as having anxiety or PTSD post-TBI. Individuals with PTSD were at least twice as likely to participate in a psychotherapy appointment. Although enrollees diagnosed as having PTSD participated in psychotherapy at higher rates than those of enrollees diagnosed as having anxiety diagnoses, the low prevalence of psychotherapy is concerning. Psychotherapy is considered first-line treatment for PTSD, yet these results suggest that, among individuals with TBI, pharmacotherapy is more often utilized (
27,
28). This is disconcerting, given that psychotherapy mitigates concerns about dangerous medication interactions for patients with TBI. Generally, patients often cite barriers to psychotherapy participation, such as time and hassle (
29). Specifically, identified barriers to receiving treatment for neuropsychiatric disturbances post-TBI include lack of provider and patient psychoeducation, perceived stigma, inadequate mental health insurance coverage, and limited availability of mental health providers (
30). However, it is unclear whether these barriers contribute to the low prevalence of psychotherapy participation or to what degree clinical decision making is guided by other factors.
We observed differences in the characteristics of individuals with anxiety and those with PTSD, which may influence treatment decisions. There is a 10-year age difference between those with anxiety and those with PTSD, and there is a large sex difference. Our results suggest that, post-TBI, older women are more often diagnosed as having anxiety, whereas younger men are more often diagnosed as having PTSD. Further, the percentage of individuals with pre-existing mental health disorders was high. This is consistent with other nationally representative studies that observed significant associations between TBI and lifetime mental health disorders, and it provides support for the hypothesis that people with comorbid psychiatric concerns are more likely to engage in activities that result in TBI (
31,
32).
Those diagnosed as having PTSD had a higher prevalence of substance use disorders. Thus, emerging from these data are questions about how certain characteristics relate to diagnosis and subsequent treatment decisions. This question is prompted by the observation that receipt of medication differs by diagnosis, despite the significant overlap in indications. Similarly, although psychotherapy is recommended first-line treatment for anxiety disorders and PTSD, enrollees diagnosed with PTSD were significantly more likely to participate in psychotherapy.
The prevalence of PTSD in our sample was lower than expected. For example, other studies have estimated PTSD prevalence post-TBI at between 10% and 24% for mild TBI and at 27.1% for severe TBI (
33–
35). In contrast, only 0.6% of our nationally representative sample of individuals with a TBI diagnosis also had a PTSD diagnosis. In this study, we excluded individuals with comorbid anxiety and PTSD diagnoses, but had we included them (N=2,317), the prevalence of PTSD would have increased to only 1.7%. Reasons for the discrepancy between PTSD prevalence in this study and that in the extant literature are unknown but could include both patient and provider factors. For example, clinicians may believe that PTSD is a stigmatizing diagnosis, or they may lack expertise and experience in diagnosing PTSD. The extent to which this or patient-level factors such as demographic characteristics contribute to receipt of a PTSD diagnosis should be explored in future studies.
The following limitations must be considered when interpreting these results. First, diagnoses were obtained from administrative claims data; therefore, diagnostic accuracy for the primary disorders (anxiety and PTSD) and secondary (comorbid disorders) is unknown. Similarly, the severity of the disorders is not known. The implications of these limitations are well documented in the extant literature, which uses administrative claims data (
16). Nonetheless, the results reflect the current state of PTSD and anxiety diagnoses submitted for reimbursement in a large national sample of individuals with TBI. A significant limitation of administrative claims data is that the indication for medication fills is absent. The same problem exists with psychotherapy; however, unlike with medication, we can confidently state that the beneficiary attended the psychotherapy appointment.
Second, there are limitations specific to this study. Individuals diagnosed as having anxiety or PTSD pre-TBI were not excluded from the sample. This poses a challenge for drawing conclusions about treatment trajectory related to new-onset anxiety and PTSD post-TBI; however, this sample represents patients in the community who are likely to present for psychiatric services post-TBI. Relatedly, we did not examine receipt of medication in isolation of psychotherapy. Future studies should consider focusing on specific medications. This information may provide insights about specific drugs and lead to better recommendations about prescribing practices post-TBI. Our time-trend analysis was conducted at the population level and was not adjusted for differences in characteristics between the anxiety and PTSD cohorts. This may have had the effect of introducing bias into our between-groups effect estimates.
Similarly, information about the type of psychotherapy (e.g., supportive therapy, cognitive-behavioral therapy) may elucidate service gaps for specific populations. Relatedly, an investigation into the interaction between demographic characteristics, diagnosis, and treatment decision making warrants attention. This is important for clinical decision making and ensuring that patients receive the best treatment options based on clinical evidence.
To our knowledge, no study has examined anxiety and PTSD treatment post-TBI using administrative claims data. To inform treatment decisions, evaluate adherence to guidelines, and direct future pharmacological and psychotherapeutic studies, it is imperative to understand how individuals with anxiety and PTSD post-TBI are treated in the community. As well, this study highlights the gap between research and clinical practice. One study estimated that medical advances take 17 years, on average, to become incorporated into common clinical practice. Incorporating medical advances requires clinician behavior changes, patient expectation changes, and information dissemination changes (
36,
37). The present study revealed a first look at the treatment patterns at a monthly level post-TBI, which could not be achieved on a large, encompassing scale outside of administrative claims data.