The novel coronavirus disease (COVID‐19) outbreak has impacted more than 200 countries/territories across continents with nearly 3 million confirmed cases as of the end of April 2020 (
1). As the first country identifying the disease, China may also first witness a wide range of negative impacts of the outbreak on society. Such negative impacts have a considerable influence in vulnerable populations. Women in pregnancy tend to be more emotionally susceptible to emergency events (
2), posing them at higher risk of stress and mental health conditions.
Depression in pregnancy or prenatal depression (PND) is predictive of postpartum depression (PPD) (
3) which is a type of mood disorder that occurs after giving birth and can lead to adverse consequences on mothers, offspring, and family (
4). Although the pathogenesis of PPD remains unknown, there are proposed contributors, such as negative life events (
2,
3). Stressful events encountered by pregnant women during this outbreak appear to be more prevalent, which can, in turn, intensify presence of PND and then higher risk of PPD.
Considering the recent outbreak as one of major sources of stressors among those susceptible, traumatic stress is likely to manifest and lead to post‐traumatic stress disorder (PTSD)—a mental health condition that occurs after experiencing a shocking, terrifying, or dangerous event such as emergency crisis and catastrophic disaster (
5). Distress and malfunctioning accompanied with the onset of PTSD require close observation. These mental health conditions which occur during the COVID‐19 may be neglected due to the more immediate issue of controlling the spread of COVID‐19.
Precautionary behaviors and associated psychological responses directly resulting from the novel virus outbreak have become the interests in the public and authorities (
6). The availability of this information may not only help assess the effectiveness of implemented measures but also form an insight of the outbreak's impact on mental health at later stages (
7). On the other hand, examination of the undertaken behaviors and the behavior‐induced psychological arousal enable us to characterize such changes throughout the outbreak development, which will help inform subsequent effective actions as well as healthcare improvements that require inclusion of mental health care.
In view of traumatic stress along with psychological and behavioral responses to be more pronounced in the general public during the present outbreak period, vulnerable subgroup population such as pregnant women are at higher risk. Females have been deemed to be more emotionally reactive against emergency situations and therefore more susceptible compared to their male counterparts (
8,
9). In addition, those in pregnancy who require routine prenatal care can be even more affected due to suspension of services. All these additive impacts posed on pregnant women call for increased awareness of their mental health, especially during this coronavirus pandemic. In addition, this improved mental health care should be extended to other vulnerable population including children, elderly adults and people with chronic conditions. Therefore, it cannot be over‐emphasized to assess pregnant women's mental health conditions under this very period when access to basic services and professional support can be difficult because of fear, lockdowns, and restrictions to many activities as currently occurring in many affected countries including China, United States, and others (
1).
Using a national‐based sample of pregnant women from all regions in China, we aim to assess presence of suspected PTSD and probable PND and to characterize infection‐induced preventive behaviors and psychological responses.
Methods
Study Design and Participants
We analyzed data based on a population‐based cross‐sectional sample of pregnant women from all regions in China. Participants were invited to complete a web‐based questionnaire. These participants were initially recruited from local hospitals distributed across the nation via a hospital‐based online education scheme for Chinese women during antenatal and postnatal periods. This online scheme allows local hospitals to assess participating pregnant women's health conditions and provide primary care to their clients on a web basis during their pregnancy. Informed consent from each participant were obtained when they participated in the scheme and when they endorsed to commence the questionnaire. Data analyzed for this study were collected from 1908 second or third trimester pregnant women between 13 and 16 February, 2020.
Outcomes and Covariates
Depression in pregnancy or PND was assessed using the Edinburgh Postnatal Depression Scale (EPDS), Chinese version. The EPDS is a 10‐item screening instrument designed to assess depressive symptomatology during the perinatal period to identify pregnant women at risk of PPD (
10,
11). EPDS scores range from 0 to 30 and each question is in four‐point format with possible scores from 0 to 3. Reverse scoring is also applied in the EPDS. Respondents are required to answer each question based on their feelings in the past 7 days. Participants with 13 or more points indicate a high risk of suffering with depression, classified as probable PND or moderate PND if diagnosis confirmed (
12), who should seek medical attention and urgent intervention if required. Participants who score 10–12, indicating experiencing depressive symptoms, are classified as possible PND or mild PND if diagnosis confirmed (
13). To maximize the applications of the EPDS and inform follow‐up interventions, we were also interested in the risk of PPD among pregnant women by assessing their depressive symptoms during pregnancy using this screening instrument.
Post‐traumatic stress was measured using the simplified Chinese version of PTSD Checklist‐Specific version (PCL‐S) (
14). PCL asks respondents to indicate their degree of being bothered (five‐point format) in response to specific stressful life experience in the past month (
15). For the purpose of this study, the specific stressful experience was standardized as “the COVID‐19 outbreak since late December, 2019.” We used the abbreviated six‐item version in this study (
16). The six items were derived from the original 17‐item version with two items from each of three clusters (i.e., re‐experiencing, avoidance, and hyperarousal) and have been validated for psychometry properties (r=0.96–0.97 with the original total score). When using ≥14 as the cut‐off, the checklist resulted in sensitivity of 0.8–0.95 and specificity of 0.69–0.76 based on diagnostic interviews. This study adopted ≥14 as the cut‐off point to classify participants as at lower or higher risk of PTSD (
16). Due to the outbreak underway at the time of data collection, those at higher risk (≥14) were demoted as suspected PTSD.
We also evaluated multiple psychological and behavioral responses towards the COVID‐19 including anxiousness about infection of members within one's social network (five questions), specific psychological responses (anxiousness when staying at home, lack of security, and loss of freedom; three questions), precautionary behaviors (handwashing, use of facemasks, wearing gloves, and housebound behaviors; four questions) and psycho‐behavioral responses particularly related to pregnancy (anxiousness about miscarriage and premature birth, fear of antenatal check‐up and consultation, and cancellation and postponement of antenatal visit; six questions).
Participants' age, marital status, educational attainment, occupation, primiparity, presence of gestational complications, history of depression of any types were also collected.
Statistical Methods
Descriptive statistics were computed for all variables. Frequency and percentage were reported for categorical variables whilst mean and standard deviation were reported for numerical variables. Median and interquartile range were also reported for those non‐normally distributed numerical variables. Logistic regressions were also used to examine the association between probable PND and suspected PTSD adjusted for covariates and potential confounders. Adjusted odds ratios and 95% confidence intervals were calculated. All analyses were conducted in R version 3.6.2.
Results
Table 1 shows sample characteristics and relevant variables included in the study. Among a total of 1908 questionnaires returned, 1901 women provided valid data (mean [SD] age, 28.9 [4.7] years). All were married or cohabiting except 14 respondents. More than half of the sample population were educated to at least post‐secondary levels. Nearly half reported themselves as full‐ or part‐time employed, or housewife. Nearly half of women were primiparas. Our sample included pregnant women from all regions in China, and 5% of the respondents were from Hubei province in which the epicenter Wuhan is located, which is similar to the proportion of the whole Hubei population in China (4%, χ
2=0.11, df=1, p=0.739). There were 11% of participants with gestational complications, and 8% of them suffering with depression of any forms in the past.
Prevalence of probable PND (EPDS score ≥13) in the sample was 34% whilst more than half (58%) of the women reported depressive symptoms (EPDS score ≥10;
Table 1). In respect of specific symptoms (identified by each EPDS item), more than half of the women reported frequent depressive symptoms in terms of self‐blaming, anxiety/worry, panic/scare, and feeling burdened (see items 3–6 in
Table 2). The prevalence of suspected PTSD (PCL‐S score ≥14) among pregnant women was 40%. Women with suspected PTSD had 683% higher risk of probable PND compared to those non‐suspected (OR=7.83, 95% CI, 6.29, 9.75, p<0.001; Table
S1).
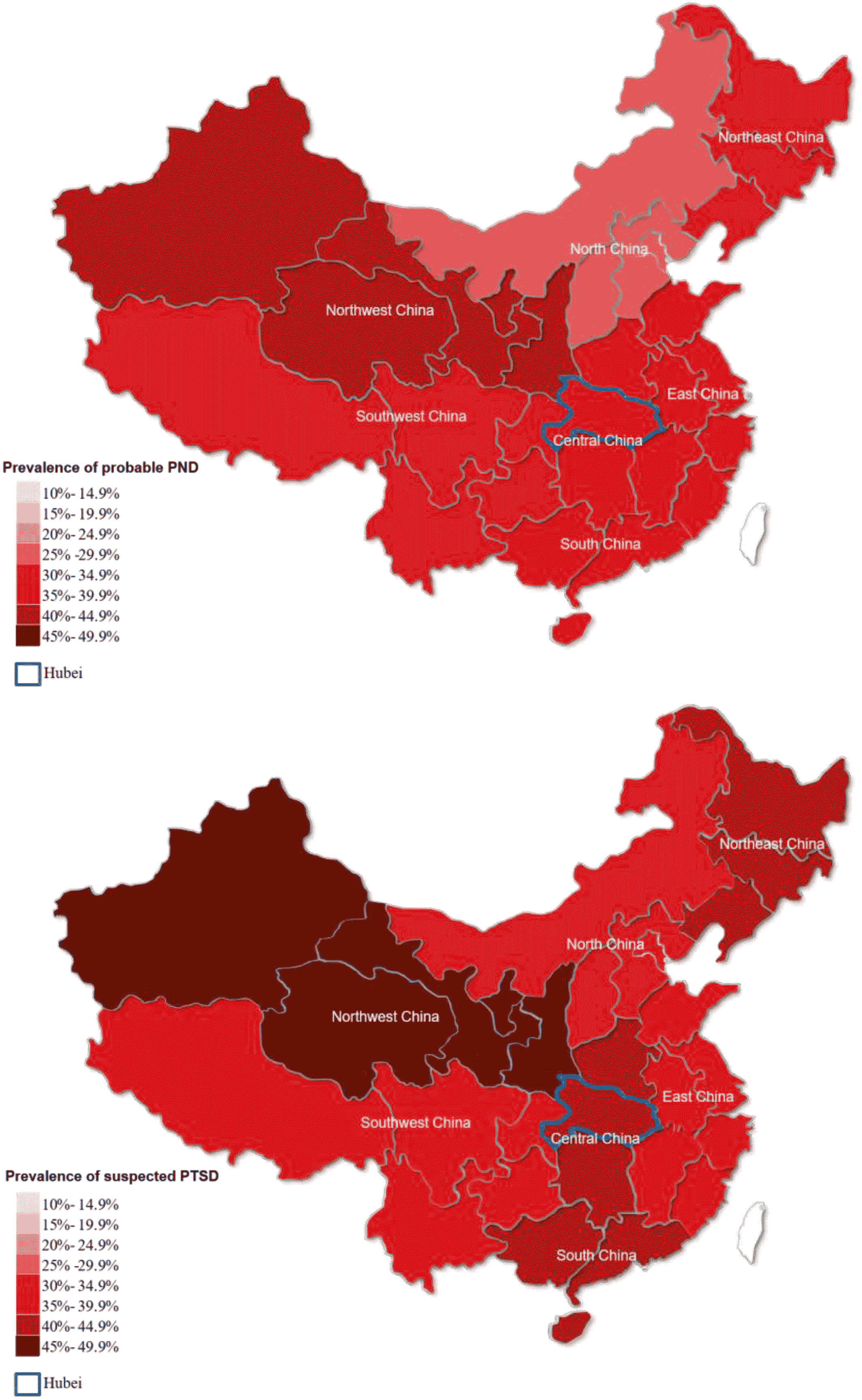
Figure 1 outlines the prevalence of probable PND (above) and suspected PTSD (below) across regions in China. The prevalence of probable PND ranged from 25% to 44% whilst the prevalence of suspected PTSD ranged from 35% to 48%. Comparing the prevalence of suspected PTSD between Hubei province in which the epicenter of Wuhan (COVID‐19) is located and non‐Hubei provinces, Hubei province had a higher prevalence than other provinces (49% vs. 39%, p=0.044).
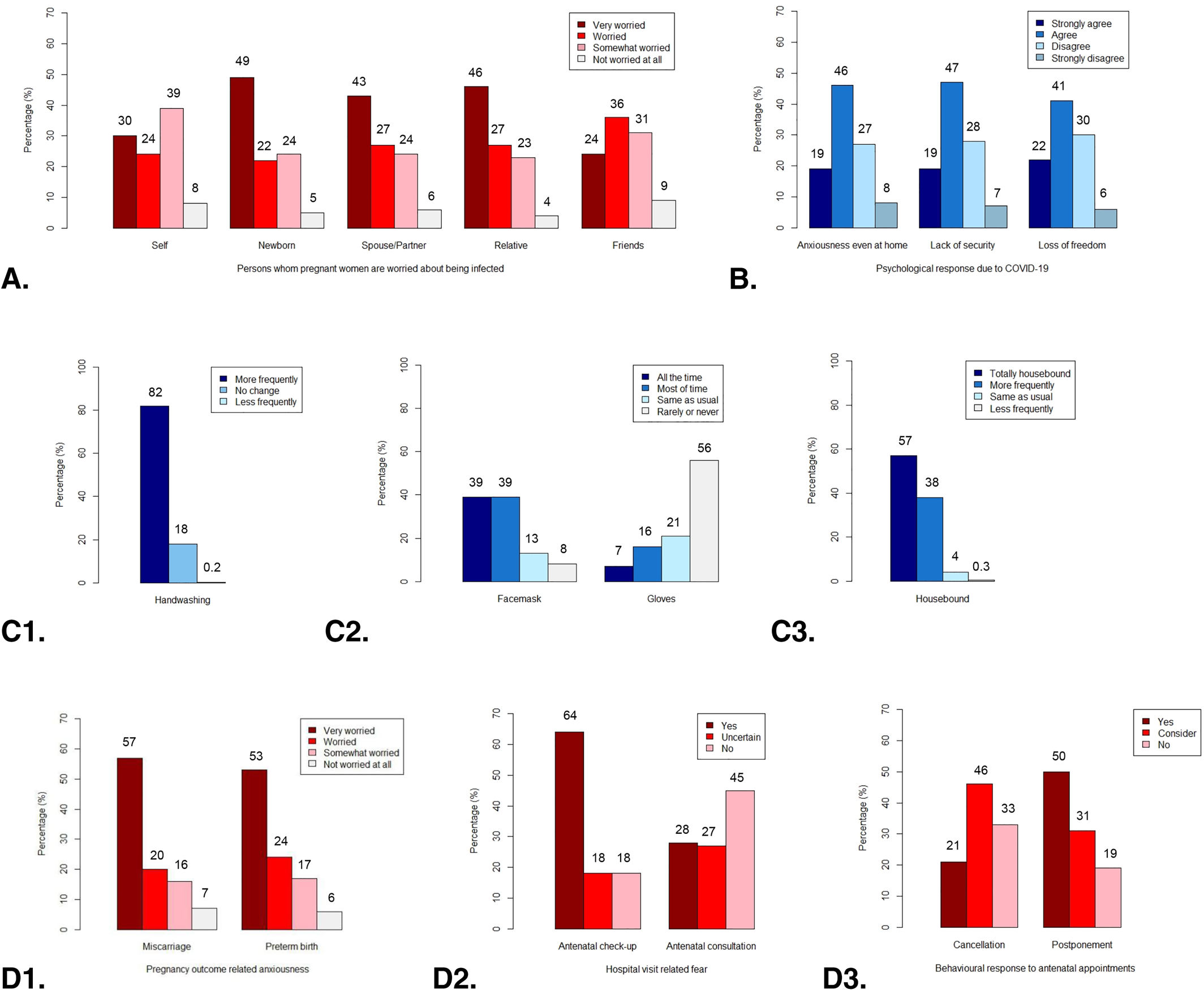
Figure 2 depicts the distribution of psychological and behavioral responses among the pregnant women. Details of the statistics are available in Table
S2. There were almost half of pregnant women expressing higher levels of anxiousness (“very worried”) about their incoming new‐borns contracting COVID‐19; higher levels of anxiousness expressed regarding their spouse/partner and other relatives also accounted for nearly half of the sample (see Panel A). In contrast, anxiousness about themselves and friends at higher levels tended to constitute a relatively lower proportion but still reached 30% and 24%, respectively. In addition to medium and lower levels, anxiousness about COVID‐19 infection were reported in the majority of the pregnant women ranging from 91% to 96%. This shows that only a minority of them (4%–9%) expressed completely no anxiety about infection of themselves or members within their social network. In respect of specific psychological responses (Panel B), including anxiety even during staying at home, lack of security, and loss of freedom, approximately 65% of respondents admitted undergoing these negative experiences due to the course of infectious outbreak (reporting “strongly agree” or “agree”). Stemming from the onset of this outbreak, increased frequency of particular prevention behaviors was reported by our respondents (Panels C1‐C3). To reduce risk of infection, more frequent handwashing comprised over 81% of the sample while less than 18% reported no change. Facemask use also became prevalent among pregnant women of which 78% wore facemasks all the time or most of the time. Nonetheless, there was a small proportion of women who reported never or rarely wearing facemasks. More frequent or complete housebound behaviors were also undertaken among 96% of women with more than half of them being totally housebound. By contrast, gloves wearing was less common with more than half not adopting such precautionary measure while only fewer than a quarter of women reporting wearing gloves all the time, most of time or sometimes.
In terms of psycho‐behavioral responses related to pregnancy (Panels D1–D3,
Figure 2), more than three quarters of women conjured up a feeling of anxiousness or extreme anxiousness related to miscarriage and/or premature birth if they were infected. Despite the ongoing COVID‐19 epidemic, nearly half of pregnant women indicated no feeling of fear for antenatal consultation undertaken in hospital. However, nearly two thirds of them in fact voiced in fear of antenatal check‐up in hospital. Regarding antenatal appointments, half of them preferred the postponement of their visit while approximately one‐fifth women opted for cancellation.
Discussion
Our study found high prevalences of probable PND (34%) and suspected PTSD (40%) among pregnant women during the early stage of COVID‐19 outbreak (from January to early February 2020). The observed prevalence of these two disorders appeared to be much higher during the outbreak compared to those reported during the periods of no infectious disease outbreaks (
17,
18). The prevalence of probable PND observed during the ongoing traumatic event in this study is much higher than the previously reported estimates 5%–23% (
19,
20,
21). In terms of suspected PTSD, varying between degrees of exposure, the observed prevalence in this study is comparable to the upper bound of previously reported 30%–40% among direct victims and is much higher than 5%–10% in the general population (
18,
22). Our results also echo the recent findings (
23,
24) that the prevalence of mental disorders in emergency settings have been higher in past decades, indicating the potential of substantial population underdiagnosed and undertreated.
Women with probable PND assessed using the screening instrument EPDS in this study characterize the population who were experiencing depressive symptomatology during the unprecedented scale of disease outbreak taking place in China, which is deemed to be more extensively influential than the severe acute respiratory syndrome outbreak in 2003 (
25). Probable PND cases identified by the EPDS (score≥13) require emergency interventions according to the recommendations specified in existing guidelines (
26,
27). Depression during pregnancy was identified to be one of the strongest predictors for later suffering with PPD, accounting for moderate effect size (approximately 0.45), as shown in earlier studies (
3,
28). Our findings signify a pressing need that depressive symptoms occurring during prenatal period should be recognized and those at high risk should be closely evaluated or referred if needed. This is because severe conditions that are not treated will pose long lasting adversities to the health of the mothers and their children. This could also extend to the whole family and which increase the burden on the existing healthcare system (
29). Also, same for other chronic mental health disorders, early detection can result in reduced sequalae and better quality of life (
23). Being aware and open to tackling perinatal depression should be viewed as a high priority given the current emergency in China.
Although throughout the article we primarily referred to probable PND, those population at less severe levels but demonstrating depressive symptoms to certain extent or considered as mild PND, that is, EPDS score≥10 but lower than 13, should not be neglected (
13,
30). As mentioned above, depression during pregnancy, especially the untreated forms, can contribute to subsequent presence of PPD. Therefore, during the prenatal period, assessment and reassessment in 2–4 weeks for women at this milder symptomatology level should be followed up to determine whether further healthcare support or treatment is required. Given the unfolding of PND being somewhat unpredictable, for example, mild symptoms at early stage but can persist or develop (
30), monitoring practice as well as women being aware of their mental health should be considered. This may help mitigate the situation where women do not recognize their depressive symptoms until after childbirth or feel embarrassed to seek help due to stigma (
13,
31).
High prevalence of suspected PTSD in our study represents the real‐time percentage of the Chinese pregnant population who are mentally affected by the current and ongoing pneumonia‐like disease. Given that such prevailing concerns on mental health problems may indicate crisis or unresolved trauma (
32), high percentage of positive scores on the PTSD checklist may speak up for the possibility of this psychopathology. High proportion of suspected PTSD cases identified in our study reflect the circumstance that mental health concerns become more prominent following the emergent outbreak itself. Large proportion of our sample who voiced their anxiety from aspects of psychological and behavioral responses also point up the nexus between traumatic stress and mental health problems. Special attention to outbreak‐related distress among pregnant women is urgently needed, which is in line with a recent call for mental health campaign (
7).
Given that the outbreak is ongoing, high prevalence of PTSD suspected cases could be potentially overestimated. Irrespective of such potential upward bias, its association with high PND prevalence observed in this study should not be deemed as unworthy of attention. In fact, history‐of‐depression‐adjusted odds ratio of probable PND is estimated to be 683% higher in those PTSD‐suspected cases compared to non‐suspected cases (Table
S1). This suggests the COVID‐induced stress could exert long‐term influence on postnatal affect. Apart from such psychopathological mechanism, it is also likely that unprecedented control measures, for example, city lockdown or community quarantines, have intensified such outbreak‐induced stress and, in turn, pose greater emotional impacts on pregnant women (
33). Given the measures being underway at the time of data collection, it is anticipated that the reported prevalence will prevail for an indefinite period depending on the progress of outbreak development and the effectiveness of recent and upcoming new measures. Such compelling results in this study articulate the potential devasting effects of acute diseases on pregnant women’s mental health, urging healthcare to be prioritized in such ever under‐resourced area of public health (
34). Besides, it is possible that part of the observed association between PND and PTSD can be explained by the highly correlated symptoms reported by those experiencing both conditions (
32,
35).
Notwithstanding the outbreak firstly taking place in China, sharply increasing cases (
1) reported in neighboring Asian countries as well as countries across wider regions imply that the identified traumatic stress‐linked mental health issues among pregnant women could be of upcoming worldwide concerns, following the circumstance that the COVID‐19 itself is now pandemic and has been announced as an international emergency by the WHO (
36).
There are several strengths and limitations in this study. Our study relied on the analyses of a national‐wide sample of pregnant women from all regions in China. We characterized the presence of psychological and behavioral responses towards the onset of outbreak and examined the associations between demographics, suspected PTSD, and risk of PND. Universal results across multiple variables between Hubei and non‐Hubei subsamples (see Table
S3) suggest mental health problems can be manifest and generalizable in a range of areas within the nation. Measurement of depression during pregnancy and risk of PTSD were based on the commonly used screening instruments (
12,
16). Diagnoses of specific diseases should always be carefully evaluated following structured clinical interviews administered by healthcare professionals. Due to the nature of design, we may not be able to infer the causality between outbreak impact and mental health outcomes. Limited available data at this stage may have confined our abilities in more descriptive and general analyses. Intricate and underlying relationships among variables of interest should be further elucidated when complex data become available. One of possible directions can be the influence of social media. Digital health may also contribute to our understanding (
37).
In conclusion, high prevalence of probable PND observed in our study suggests the transcending impact of COVID‐19 on mental health via potential traumatic stress. This calls for raised awareness of mental health issues in society and healthcare to be prioritized in this under‐resourced area. Special attention and support for the vulnerable subgroup population are highly needed. Contingent on the progression of such pandemic and the effectiveness of implemented measures, mental health care should become part of public health measures during the present outbreak and should continue to be intensified to empower the health system for post‐outbreak periods.