Attention‐deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder that is characterized by a persistent pattern of inattention and/or hyperactivity/impulsivity that interferes with functioning, development, and ability to perform daily activities, including academic participation (
1).
The prevalence of ADHD among adolescents in the United States has been examined in multiple studies. Using cross‐sectional, population‐based data from the National Health Interview Survey (NHIS), the estimated prevalence of diagnosed ADHD in U.S. children and adolescents was found to have increased from 6.1% in 1997–1998 to 10.2% in 2015–2016 (
2). Meta‐analytic results of 86 studies published between 1996 and 2011 (
N = 163,688) revealed that, while prevalence estimates reported by individual studies varied widely, the pooled prevalence of ADHD in children and adolescents is similar when defined by parent ratings, teacher ratings, or a best estimate diagnostic procedure (5.9%–7.1%) (
3). Using updated data from the NHIS, the weighted prevalence of child and adolescent ADHD was stable in recent years (2017–2022) at around 10% (
4).
While ADHD is typically seen as a disorder that most significantly impacts childhood and adolescence, ADHD can persist into adulthood. Information regarding the prevalence of ADHD in adults in the United States is limited and varies widely. A 2006 nationally representative household survey estimated the prevalence of adult ADHD to be 4.4% (
5). Some studies have shown regional increases in the prevalence of adult ADHD from 2007 to 2016, but there is a lack of national data (
6). A systematic review and meta‐analysis of six studies published between 1996 and 2005 revealed a 2.5% estimated pooled prevalence of adult ADHD (
7). Subsequent meta‐analytic findings of 11 studies (
N = 14,112 individuals) published between 1996 and 2011, results suggested a 5.0% prevalence of adult ADHD (
3)—approximately twice the prevalence found by Simon and colleagues (
7), suggesting an increase in adult ADHD incidence.
The variability of ADHD prevalence estimates has been attributed to differences in study methodology, diagnostic criteria, impairment criterion, and the source of information for ADHD symptoms (
8). Moreover, a lack of parental knowledge and awareness of ADHD symptoms may prevent parents from seeking evaluation and treatment for their child, thus significantly impacting the detection of ADHD (
9,
10). In addition, parental reluctance to pursue treatment can be magnified by perceived stigma, including fear of judgment from others and fear of ADHD medication (
9,
11). Teachers serve an important role in ADHD diagnosis through symptom recognition in the classroom. Informing parents of potential ADHD symptomatology and providing information to clinicians aids the ADHD assessment process and accurate diagnosis (
12). Lastly, lack of accessible care, extended wait times for appointments, lack of affordability, and inability to leave work to take their child to their appointments have been cited by parents as a barrier to their child's treatment (
9,
11).
Due to the conflicting findings of the data surrounding ADHD incidence in both adolescents and adults and the lack of analyses in recent years, our team proposed to apply a retrospective cohort design and joinpoint regression statistical analysis to estimate the incidence of new ADHD diagnoses among adolescents and adults using a large clinical sample. Importantly, this study examines new ADHD diagnoses between the years of 2016 and 2023 in order to investigate diagnostic trends before, during, and after the height of the COVID‐19 pandemic. Although there have been conflicting findings in the current body of literature, there are some indications of worsening ADHD symptoms and increases in diagnoses due to the pandemic (
13,
14). We hope our findings will contribute to the literature regarding the pandemic's impact on mental health and long‐term outcomes. By examining diagnostic trends prior to, during, and after the height of the COVID‐19 pandemic, the present retrospective cohort investigation aims to promote improved management of ADHD. Specifically, this study seeks to provide data to support future investigation in identifying potential modifiable risk factors, ensuring sufficient treatment resources, developing targeted interventions, and addressing diagnostic disparities.
METHOD
Data were obtained from Sisters of Saint Mary (SSM) healthcare system's Virtual Data Warehouse (VDW). The VDW was created and is maintained per Health Care Systems Research Network (HCSRN;
www.hcsrn.org) specifications. The VDW has captured clinical encounters from multiple healthcare systems since 2008, including over five million patients from both academic and non‐academic ambulatory and inpatient settings. The SSM healthcare system has locations in four states (Illinois, Missouri, Oklahoma, and Wisconsin) from which the majority of patients in the VDW reside. VDW variables are defined according to the network's specifications and are created from ICD‐9 and ICD‐10 codes, procedure codes, pharmacy orders, vital signs, laboratory tests, and demographics. Multiple studies have been published using this data source (
15,
16,
17,
18). VDW data does not require patient participation, is de‐identified, and protects patient privacy. Accordingly, the present study was approved by the Saint Louis University Institutional Review Board as non‐human subjects research.
Participants
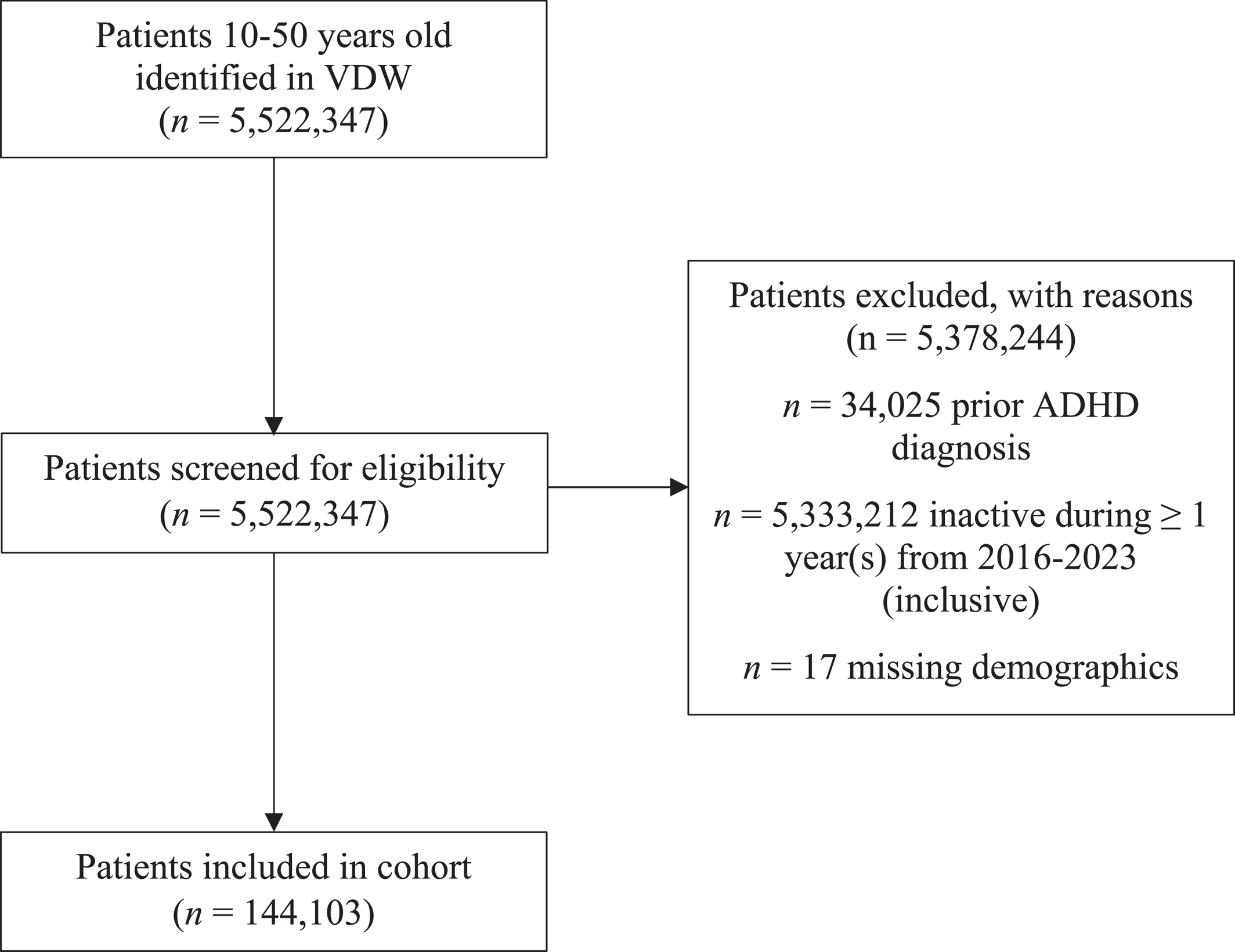
Patients without a diagnostic history of ADHD were selected for participation in this retrospective cohort study. To ensure patients were regular users of the SSM healthcare system, patients were required to have activity in each year of observation (2016–2023). 2016 was selected as the first year of observation because this was the first complete year of ICD‐10 implementation. Aligned with the study's objective of examining ADHD incidence rates among adolescents and adults, adolescent patients were included in the study if they were aged 10 to 18 years in 2016, and adult patients were included if they were between 19 and 50 years old during the same timeframe. To minimize the influence of substantial outliers and reduce data skewness, individuals over the age of 50 years were excluded, as ADHD is most commonly diagnosed before this age. Application of these criteria yielded a cohort of 144,103 eligible patients. For analytic purposes, the cohort was divided into two age groups: adolescents ages 10–18 years old (adolescent group) and adults ages 19–50 years old (adult group). Cohort selection criteria are outlined in
Figure 1.
Analytic Approach
A new ADHD diagnosis, as defined by ICD‐10 code F90 in patient charts, was the outcome of interest. The trend in new ADHD diagnosis was analyzed separately for adolescents and adults using joinpoint regression (
19). Joinpoint analysis is a statistical method used to analyze trends over time and identify significant changes in those trends. The analysis fits a series of joined straight lines on a log scale to the trends in annual data points. The point where these lines connect is called a joinpoint. Each joinpoint denotes a statistically significant change in trend, using an alpha of 0.05 for all tests. Since joinpoint is a statistical method that focuses on modeling changes in trends over time rather than adjusting for other variables that influence the outcome of interest, we were unable to control for confounding variables. However, we were able to analyze the differences in demographic variables among participants, which are summarized in
Table 1. Due to the very large sample size of this study, we utilized Standardized Mean Difference percent (SMD%) in addition to traditional
p‐value when comparing cohort characteristics by age group. SMD% accounts for sample size, and, as a rule of thumb, any difference of 10 or greater indicates a meaningful difference between groups.
RESULTS
Overall sample characteristics are shown in
Table 1. The cohort consisted of 144,103 patients—16.1% adolescents and 84.0% adults. The mean age was 33.8 years (
SD = 12.0). The majority of participants were female (68.8%) and White (82.2%). The cumulative incidence of new ADHD diagnoses during the observation period was 7.2% (10,434 new diagnoses).
Table 2 shows annual incidences of ADHD sorted by year and age group. The annual incidence of ADHD in the total sample ranged from a high of 1.15% in 2017 to a low of 0.67% in 2020. The incidence among adolescents aged 10–18 years old (1.36%–2.89% annually) was more than twice as high compared to adults aged 19–50 (0.54%–0.95% annually).
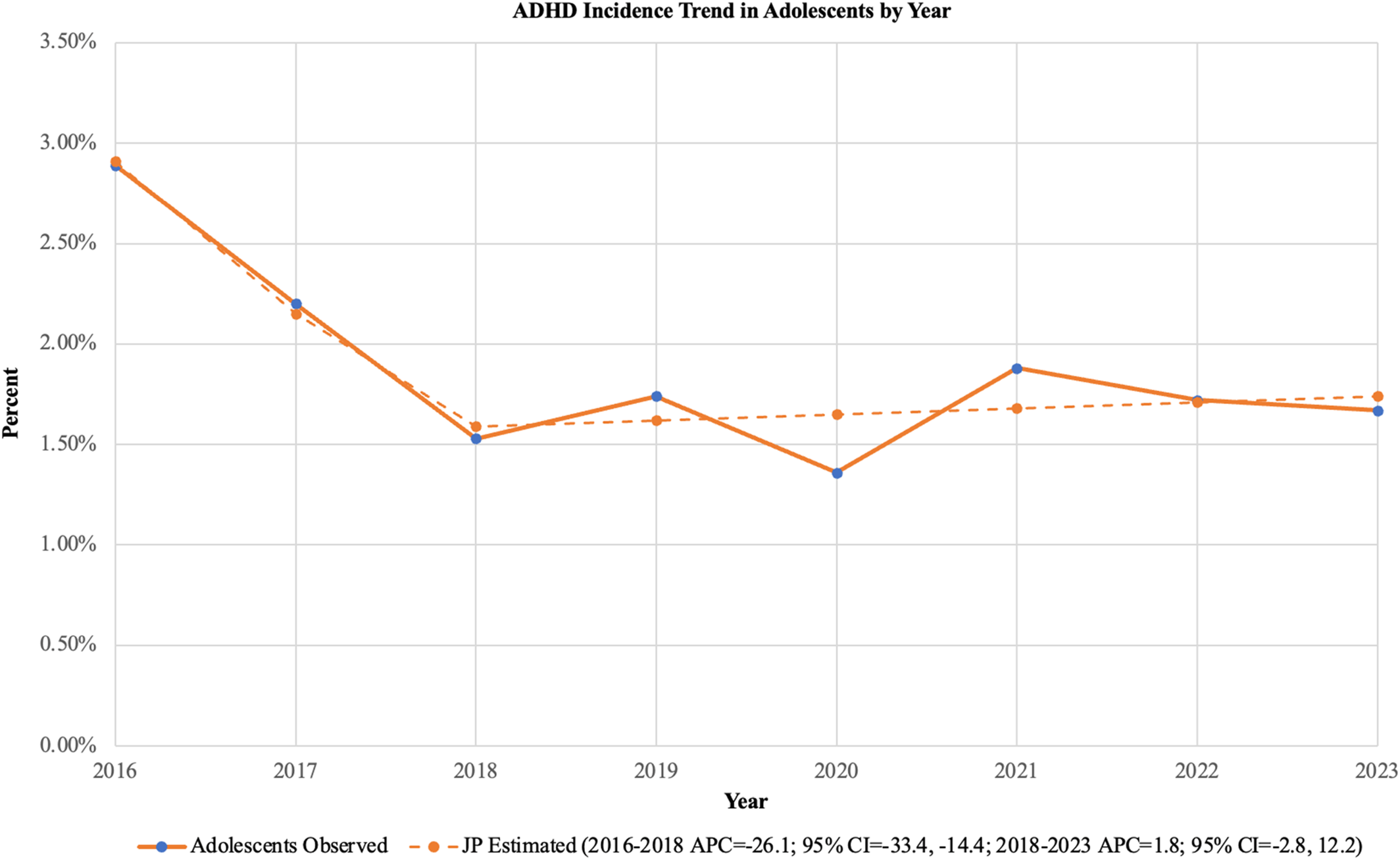
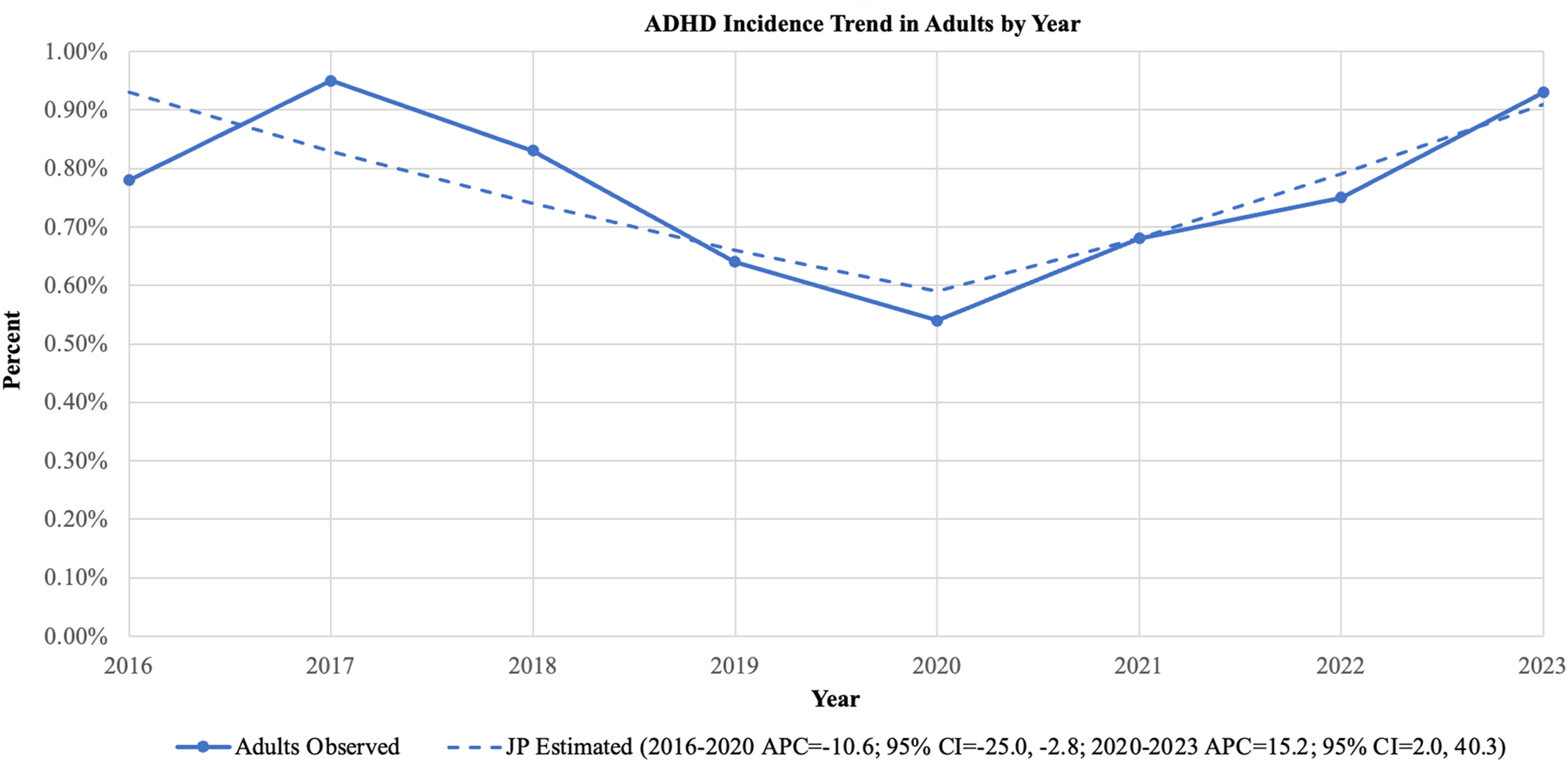
Figures 2 and
3 display the observed and regression estimated rates of ADHD diagnosis by year.
Figure 2 shows that, among adolescents, the observed ADHD incidence was 2.89% in 2016 and fell to 1.67% in 2023. The joinpoint regression detected a significant change in trend in 2018. The trend from 2016 to 2020 showed a statistically significant decrease. Between these years, the relative decrease in ADHD incidence was 26.1% annually (APC −26.1%; 95% CI −33.4%, −14.4%). However, the trend from 2020 to 2023 did not show a statistically significant change.
Figure 3 shows that, among adults, the observed incidence of ADHD started at 0.78% in 2016 and ended at 0.93% in 2023. The joinpoint regression detected a significant change in trend in 2020, and both of the segments (2016–2020 and 2020–2023) showed a statistically significant change. Between 2016 and 2020, the relative annual percent change (APC) was 10.6% (APC −10.6%; 95% CI −25.0%, −2.8%). Between 2020 and 2023, the trend reversed, and the average relative increase was 15.2% (APC 15.2%; 95% CI 2.0%, 40.3%).
DISCUSSION
When examining the trends in new diagnoses of ADHD in a large clinical sample of adults and adolescents, a change in trajectory was found among both adults and adolescents. Among adults, a significant downward trend in ADHD incidence between 2016 and 2020 was followed by a significant upward trend between 2020 and 2023. Among adolescents, a significant downward trend was noted between 2016 and 2018, whereas the incidence rate was relatively stable between 2018 and 2023.
These findings indicate that the incidence rate of ADHD diagnoses among adults and adolescents has fluctuated over the years, with distinct trends observed during different time periods. Fluctuations in incidence rates are likely due to a complex interplay of various factors, such as increased knowledge and destigmatization of ADHD, changes in diagnostic practices, increased access to healthcare services and treatment‐seeking patterns, and the impact of the COVID‐19 pandemic on mental health. Increased awareness and destigmatization of ADHD can lead to more diagnoses being made, resulting in higher incidence rates. As knowledge about ADHD symptoms improves among healthcare providers, parents, and teachers, more cases may be identified and diagnosed. Changes in diagnostic criteria or guidelines for ADHD can also influence incidence rates. For example, the expansion of ADHD criteria in the DSM‐5 compared to previous editions may have contributed to an increase in diagnoses (
20). However, variations in diagnostic practices and assessment methods across clinics and regions can lead to differences in incidence rates (
21). Some clinics may be more stringent in diagnostic assessment methods and applying diagnostic criteria (e.g., full psychoeducational assessment), while others may be more lenient (e.g., use of brief screening measures), likely resulting in lower and higher incidence rates, respectively. Access healthcare services and treatment‐seeking patterns can influence the identification of ADHD in both directions. Lastly, the COVID‐19 pandemic had a substantial impact on mental health, including some indications of worsening ADHD symptoms and new‐onset diagnoses of ADHD (
13,
14,
22), which may have contributed to our findings of an increased ADHD incidence rate among adults.
Our study is one of few that evaluates trends in new ADHD diagnoses in both adults and adolescents in recent years, including before, during, and after the height of the COVID‐19 pandemic. Other strengths include a large, community‐based sample that utilizes data from over five million patients. The results of the present study should be interpreted in the context of several limitations. Importantly, joinpoint regression analysis does not account for covariates. However, our study sought to reflect the actuality of new ADHD diagnoses that were provided in a clinical setting. As such, accounting for individual‐level covariates was not included in our analytic process. The demographic variability of the cohort is another limitation. Specifically, the cohort consisted of a higher percentage of White individuals and females. As such, findings may not generalize to other racial‐ethnic and gender identities. Additionally, patients included in our cohort utilized services from the SSM healthcare system which has locations in four states (Illinois, Missouri, Oklahoma, and Wisconsin). As such, we cannot be certain that our findings would be fully generalizable to other healthcare systems across other regions of the United States. Lastly, evaluating the underlying factors that contributed to the trends in ADHD incidence was outside the scope of the present study. The present study should inform future research to make claims regarding the underlying mechanisms contributing to the changes in incidence rates.
This study is one of the largest retrospective cohort studies evaluating the incidence rates of new ADHD diagnoses among adolescents and adults in clinical practice between 2016 and 2023. Overall, results indicate fluctuations in ADHD incidence rates in recent years, with well‐defined trends observed for both adolescents and adults. Downward trends in ADHD incidence were indicated among adults from 2016 to 2020 and adolescents from 2016 to 2018. During the years of the COVID‐19 pandemic, our findings indicate stability in new ADHD diagnoses among adolescents and an upward trend in new ADHD diagnoses among adults. In advancing our understanding of ADHD diagnostic trends in clinical practice, accurate diagnosis and management of ADHD can be promoted. Findings from this study support future investigation in identifying potential modifiable risk factors, ensuring sufficient treatment resources, developing targeted interventions, and addressing diagnostic disparities.