Mental health has generally been neglected for the world's poorest citizens—sometimes referred to with urgency as the “bottom billion.” This is true despite the fact that common mental disorders rank among the largest contributors to disability and functional impairment across income and that strategies to treat these disorders are similar to treatments for general medical priorities in terms of cost per disability-adjusted life year averted (
1–
4).
In recent years substantial progress has been made in the development of “treatment packages” for common mental health conditions in low-income regions, but less attention has been directed to the structural elements and implementation processes that determine how such packages can be best delivered on a large scale (
5–
8). Doing so will require greater attention to the architecture of delivery systems as well as the use of quality improvement methods that enable proven treatments to be disseminated effectively and sustainably. Other fields of global health, such as maternal and child health, have developed detailed frameworks that define health worker skill sets, describe core functional care pathways, incorporate performance improvement tools, and gather process and outcomes data that are positioned to guide implementation and supervision, as well as care at the point of service (
9). The emerging field of global mental health should do the same.
This Open Forum describes a planning framework that captures key tasks and principles for mental health care implementation. It addresses a Tower-of-Babel problem plaguing efforts at advancing needed investment in mental health, especially in low-income or poorly served settings. Commitments—for example, to “integrate” mental health into health care or to use “community health workers” to enhance access to mental health care—are voiced by Health Ministry decision makers, practitioners, and scholars. But how these ideas are used or the conditions of implementation needed to make them succeed vary widely.
This planning and implementation framework was developed for general use but began in order also to meet a specific challenge: to identify to a range of stakeholders the planning elements and steps needed for the integration of mental health services within two high-visibility global health initiatives: the Millennium Villages Project (MVP) and the Partners In Health system in Haiti, or Zanmi Lasante (ZL). MVP is a proof-of-concept project in ten countries and 14 sites throughout Sub-Saharan Africa that is intended to model an ensemble of scalable interventions that rely on local skill sets and capacity and that enable even the poorest communities to meet the Millennium Development Goals (MDGs) (
10). The MVP pilot site for demonstrating a scalable community mental health capacity is the Ikaram, Nigeria, site, a periurban village cluster of 20,000 people covering 44 square kilometers. Approximately 70% of the population lives on less than $1 per day. Health care is provided through the integrated work functions of government-certified and locally recruited village health workers, who are able to conduct simple diagnostic and follow-up procedures and, more specifically, through trained community health extension workers, who are linked across four primary care clinics. The proximate Federal Medical Center (FMC) is developing a mental health service capacity with input from MVP partners. MVP works with the Local Government Area (LGA) to develop strategies for scaling proven menus of interventions and delivery to meet the MDGs throughout the LGA. This is part of a national strategy in Nigeria to use debt relief funding to scale such proven sets of interventions nationally.
The ZL system in Haiti covers a catchment area of 1.3 million people, with health care provided through 12 Ministry of Health hospitals and clinics jointly run by ZL in the Central Plateau and Lower Artibonite regions and by a network of resident village health workers—called “accompagnateurs.” Care is provided almost exclusively by Haitians, with a total staff of approximately 5,500 providers, including 2,500 community health workers (CHWs). This framework is being used to guide comprehensive mental health expansion and integration at three pilot sites in the ZL network: Mirebalais, Petite Riviere, and Cange, where two-thirds of the population lives on less than $1 per day. In Mirebalais, ZL is in the process of completing construction of a national teaching medical hospital with mental health care capabilities.
Given the emphasis in both MVP and ZL on sustainable delivery of community-based, stepped health care using locally skilled individuals, these settings present unique opportunities to demonstrate that mental health treatment capacity for common disorders is possible to implement—and to scale—within larger systems strategies for delivery of primary care and success in meeting MDGs. Several of the authors are using this framework with MVP (GSB and HV) and ZL (GJR, EE, CO, GSB, and HV) as a planning checklist to coordinate action and develop implementation work plans. The details and implications of this framework were reviewed at multiple levels (for example, by providers, community leaders, Health Ministry officials, and employees of nongovernmental organizations [NGOs]) as an agreed-upon “map” for shared action in developing and expanding community mental health capacity in these systems. As of this writing, the implementation steps described by the first three implementation rules (discussed further below) are near completion in ZL and the first step of context analysis is being prepared in MVP. Future work will assess the value of this framework across these settings moving forward.
The conceptual framework
The basic set of tools described here—five core skill packages and use of five key implementation rules (“5×5”)—were developed within these projects. However, they were developed in light of broader experience and evidence with the goal of developing strategies applicable to other low-income settings more generally. They address chronic obstacles to the establishment of mental health care in these settings. Such obstacles include few or inconsistently trained mental health providers; siloed provider roles; inadequate supervision; limited proactive identification of cases or engagement and follow-up; inconsistent diagnosis and matching of evidence-supported treatments to conditions; limited information regarding the need, use, or acceptability of services or the role of local beliefs and practices; and limited use of methods that capture clinical outcomes to support quality improvement. These obstacles, and their solutions, are also relevant to health systems in many developed countries. Indeed, addressing them in low-income settings is one area in which innovation in mental health may flow from low- to high-income countries (
11,
12).
The 5×5 framework builds on growing interest in ways to expand the range of potential providers of mental health care tasks (“task-shifting”) (
13) and establish consensus on priority target conditions and treatment packages as reflected in the
mhGAP Intervention Guide of the World Health Organization (WHO) (
7). WHO also developed a Mental Health Policy and Service Guidance Package (“the Package”), a compilation of planning strategies and standards for developing mental health institutions and for creating policies and oversight that support them (
14). The Package puts important emphasis, as does this framework, on issues such as quality improvement and systems planning.
However, technical documents such as these often have limited utility without a more concise and guiding functional description of a delivery model within which they become useful (
15). Such a framework is needed if the goals of integrated and accessible care and consensus about effective treatment are to overlap not only conceptually but also operationally. The Package (and similar guidelines) describes how policy or institutions for mental health should be established. But those efforts need a framework that more specifically organizes them around sustaining and spreading successful treatment. Such a framework can provide “how-to” rules for the WHO's
mhGAP Intervention Guide or other treatment manuals to bridge the gap between simply describing packages of treatments and establishing shared expectations of the resources, skills sets, and implementation methods needed to actually deliver them to scale.
The 5×5 framework is a planning checklist that helps coordinate communication and efforts across various stakeholders. It is not a detailed technical manual for performing the practices it highlights. But it does outline the key functional elements and tasks necessary to implement and scale effective care pathways. This is a needed step to align early and emerging efforts at scaling up care along shared strategies in terms of methods and priorities. Without some agreement and ongoing conversation over core elements of strategy and functionality, it is difficult to build, test, benchmark, or collaboratively develop mental health capacity at a global level. The framework fills this need by describing two components. The first is skill packages—the minimum set of skills that can be organized to provide a range of treatments, guide training and service priorities, and adapt generalized evidence to multiple contexts. The second component, implementation rules, is a set of principles and methods that drive implementation choices.
Specified skill packages
Many health care tasks can be performed by nonspecialist, “lay” CHWs. CHWs are a central feature of health care delivery in low-income countries, and there is robust evidence for their positive effects on multiple health outcomes (
16). Using diagnostic and treatment algorithms and technologies based on a small number of clinical signs, CHWs have proven to be effective in treating such conditions as pneumonia, malaria, and dehydration and in decreasing child mortality (
17,
18). CHWs can retain trained skills for several years. However, skill retention and quality performance require ongoing supervision and periodic training updates (
19). Consistency of supervision, clarity of decision-making rules, skill-based training— adapted to local needs—access to support when correct decisions are unclear to the CHW, and refresher training have all been shown to be important to CHW success (
20–
24).
A smaller but growing literature on use of health workers for mental health care has drawn similar conclusions. Studies of the use of CHWs in low-income countries to treat depression are perhaps most relevant to these questions. Bolton and colleagues (
25,
26) showed that group interpersonal psychotherapy that was conducted by trained local residents significantly reduced depression and functional impairment in East African communities. Ali and colleagues (
27) found that local women trained as community counselors were able to treat depression effectively in Pakistan. In another study in Pakistan, Rahman and colleagues (
28) found that an adapted cognitive-behavioral therapy intervention implemented by trained “lady health workers” for women who were diagnosed as having major depression during their third trimester of pregnancy was effective both in treating their depression and in subsequent infant outcomes (episodes of diarrhea and likelihood of being immunized). In impoverished neighborhoods in Santiago, Chile, Araya and colleagues (
29) found that a program that used trained local workers to treat depression by providing enhanced psychological support and psychoeducation as well as support of medication management was effective in treating depressed women. Results from randomized studies of health workers who deployed psychoeducation, rehabilitation-focused interventions for schizophrenia, interventions for postdisaster trauma, and interventions in conflict settings also support the use of similar kinds of workers to manage condition-specific, but not highly specialized, psychological interventions (
30–
34). Similar task shifting has also been used in high-income countries.
Terms such as “community health worker” or “extension worker” have widely different usages in regard to sophistication of training and responsibilities. Not surprisingly, planning for mental health services too often stumbles over a debate about the right mix of providers. The emphasis of the 5×5 framework is to first specify a minimum set of skills, which can then be distributed along a flexible range of properly linked worker types and combinations. A delivery model of care is best thought of as a description of the minimum sets of skills that can support a range of care pathways. The planning task then is to distribute these tasks and related skills effectively across the range of available personnel, assisted by the right practice supports (the right information, summary clinical measures, triage rules for management, and so forth).
Depression is one of the most common and disabling mental disorders. It is also the best studied in terms of the fit between delivery design and effective treatment. Previous primary care-based quality improvement trials tended to focus solely on equipping clinic staff with skills for screening and diagnosing depression, and they were not successful (
35,
36). Multifaceted programs that link an ensemble of systematized care functions are necessary. Nearly two decades of randomized controlled trials in the United States and several other Western countries to improve care for depression in primary care provide a starting point to identify common elements of successful programs (
37). Although the settings and populations treated in these trials varied widely, all successful programs integrated “mid-level” providers from allied health professions to work with primary care providers to more closely screen and monitor patients for target symptoms, treatment adherence, outcomes, and side effects. In most of the trials these personnel used evidence-based counseling and were supervised through case and outcome review by psychiatrists in a structured way that divided labor between specialist and mid-levels on the basis of decision support algorithms and defined outcomes. Successful programs assisted this coordinated care by case registries that enabled proactive tracking of treatment use, follow-up, adherence, and response, which in turn enabled the provision of effective care and identification of patients who needed a change in, review of, or intensification of treatment. These features of collaborative and stepped-care methods and their importance to good outcomes inform the skill package and implementation rules described in this framework. They also provide a broad foundation of skills and management steps that overlaps with those that support care pathways for other common conditions such as anxiety (
38) and substance use disorders (
39,
40).
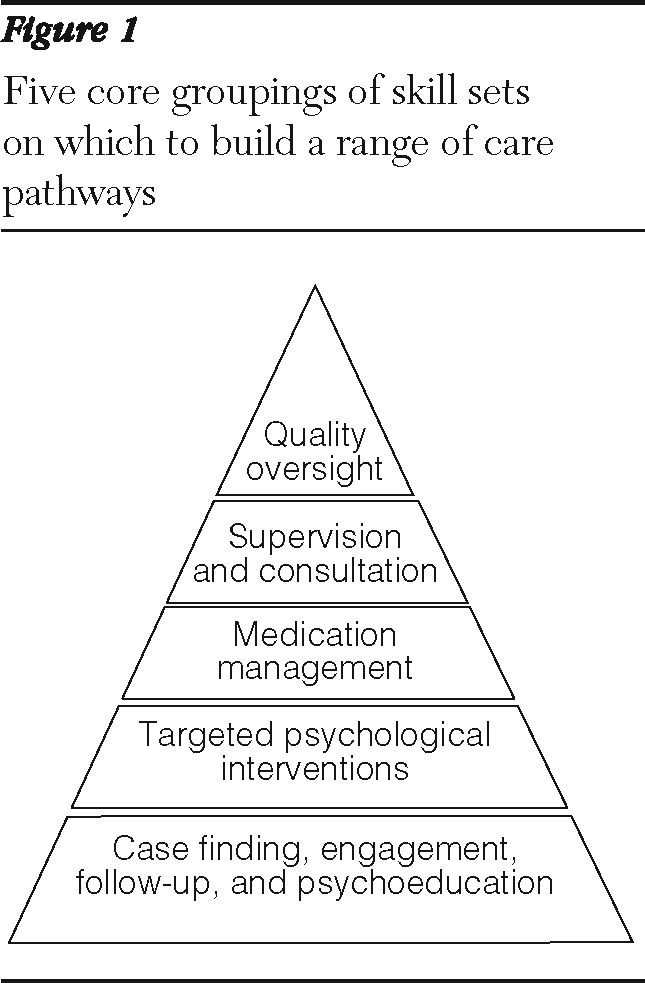
These features can and should also be used in low-resourced regions, considering the emerging evidence and experience with innovative delivery of care approaches in these setting described above. This work supports our five core groupings of skill sets on which to build a range of care pathways (
Figure 1). These are proactive screening, patient education, engagement, and systematic follow-up with attention to treatment adherence and tracking of clinical improvement; targeted, evidence-based psychological techniques (such as motivational interviewing, behavioral activation, problem-solving therapy, and interpersonal therapy), which are psychosocial treatments that can be delivered by trained health care providers who are not mental health specialists; pharmacologic treatment; supervision and consultation from a mental health specialist, who focuses on patients who present diagnostic or therapeutic challenges and are not improving as expected; and systematic and data-based outcomes tracking and quality improvement (
41).
These skill packages bundle skills that sensibly group together tasks that are similar both substantively—in terms of the education and experience needed to master them as a set—and operationally—in terms of models to organize, train, and link people to do them. Level 1 skills—case finding, engagement, follow-up, and psychoeducation in
Figure 1—commonly describe the kinds of responsibilities given to primary care CHWs or even less trained health workers to simultaneously manage multiple health conditions. Extending their capabilities to include this skill package builds on their accepted roles as front-line care managers for a range of conditions. Extending their capabilities integrates mental health care on the “ground-floor”—that is, at the accessible points of contact for entry and follow-up that CHW-based systems can provide for primary health care in general.
Different systems may use different kinds of individuals for these roles. Level 1 skill sets are carried by a combination of “village health workers” and CHWs in MVP and by “accompagnateurs” and “agents santé”— trained health extension workers—in ZL. Level 2 skill sets could be acquired by college-level graduates with social work or psychology training as in ZL or, as planned in MVP, by a subset of CHWs given additional training. Level 3 skills can be managed by a subset of prescribing providers, including advanced practice nurses or physicians. In MVP registered nurses and physicians at local clinics have these responsibilities, and in ZL primary care physicians will have them. The plan in MVP is to support level 4 skill sets through the FMC mental health service. A regional expert mental health consultation team under development in ZL and based in the Mirebalais facility will have level 4 skills. The specialists who carry out tasks at level 4—or a capable public health manager—can also assume the responsibilities of level 5.
There is room for variation in matching skill level with a particular type of worker, as reflected in the literature describing use of different worker types for mental health interventions as well as in our experience exploring arrangements that are effective in diverse local settings. Thinking first in terms of key skill packages is a more useful starting point than first trying to resolve which provider or which type of professional is the right one for providing mental health care—or than deploying whatever provider type happens to be available. Skill package levels encompass discrete, replicable task bundles, and each level is defined in a way that is amenable to measurable process outcomes to track their effective use. Role assignments by level may differ on the basis of local resources and abilities of specific workers. In some areas, very limited resources will mean that a single person possesses several levels of skills. The main point is to encourage and drive deliberate and explicit planning and collaboration around a clearly defined set of tasks, skill sets, and the training strategies and accountability to enable, sustain, monitor, and link their performance.
Implementation rules
The sustainable use of an explicit map of skill sets to guide care delivery requires what we describe as guiding “implementation rules.” Skills obviously need to be more carefully specified than the general functions described here. But “drilling down” from this five-level skill set template should follow a replicable and appropriate logic that captures and sorts a range of implementation tasks—from designing locally coherent strategies to using support tools to guide best practice—and that establishes clear points of supervisory responsibility and performance feedback (
4).
Rule 1: assess context
A first step for implementation is to assess local context. How is mental health understood, described, and addressed by potential users of mental health care? Ethnographic or similar qualitative analysis has become common in health intervention research in developing countries, and this approach should also be used routinely in implementation and management of services (
42,
43). Its primary use has been to adapt and modify treatments based on Western research or practice. Rahman and Patel, for example, in their health worker psychotherapy trials in Pakistan and India, respectively, described their preparatory qualitative and feedback work. Both started with evidence-supported hypotheses about care pathways and adapted them to the local setting (
44,
45). However, a long and continuing tradition in the ethnography of distress and mental illness casts doubt on how easy it is to carry out this adaptation. Some argue that treatments need to be “home-grown,” based on familiar practices and social strategies, and not adapted from elsewhere.
On the one hand, the prospects for disseminating and scaling effective care, especially within health systems in poor regions, are substantially reduced if they rely at every turn on extensive and lengthy local ethnographic assessments and treatment development. On the other hand, all health care is local, and whether in Nairobi or New York City, cultural, institutional, social, economic, and gendered frames of reference shape the success or failure of public health efforts. We see this tension between the local and the general not as an either-or commitment to culture that can be embraced or not but as a necessary, ongoing cycle to understand and harness. Clinical trials, whether for HIV medications or antidepressants, use standard methodologies to secure confidence in the generalizability of a tested intervention. Effective treatment of HIV still requires a mix of generalizable attributes of interventions, as well as local meanings and realities. The same is true in considering how information from a psychotherapy treatment trial in Boston should be used by therapists in Bangalore or Brussels. Managing issues of culture, adaptation, and context and using generalizable knowledge in local places is a routine, not exotic, challenge captured by the oft-described goal of linking evidence-based practice with practice-based evidence.
Therefore, the point of context assessment is not to answer the local question versus the general question (for example, “Is depression the same thing here as there?”). The purpose is to understand what it is here (rule 1) in order to plan how to enable local caregivers to use generally proven treatments in ways that may make local sense and to leverage local understandings and resources to be more generally effective (rule 2). Such understanding will also facilitate the creation of tools that make sense to local health care workers and users, supporting their ability to adjust their work in response to the clinical outcomes they get (rule 3) and thus capture how or whether local context in fact has an impact on the effectiveness of generally proven approaches (rule 4).
In both ZL and MVP, structured interview guides were developed to help workers understand how the local context shapes broadly identified functional features and capabilities of successful efforts to integrate mental health care (proven especially for depression) within primary care. The interview guides were designed to capture beliefs about the nature and impact of mental and emotional conditions and also to understand how people seek, or would seek, care for these conditions. Long before implementation of the skill set pyramid in
Figure 1 and the care pathways (see below, rule 2), workers should be asked specifically about the local acceptability of carrying out certain care and treatment functions. These include case finding and diagnosis, patient education and engagement, use of appropriate medications, use of specific psychosocial interventions (such as behavioral activation or interpersonal therapy), use of community-based support systems, systematic follow-up and outcomes monitoring, expert consultation and supervision (focusing on patients who present diagnostic and therapeutic challenges), and referral rules. Qualitative inquiry should be designed to obtain information about how these core features are understood, currently performed (or not), and locally relevant to help identify opportunities and barriers, such as stigma, to inform implementation of the core program components. Community residents should be interviewed, as well as area health providers, other community leaders, and potential partners from other sectors, such as religious leaders. The use of qualitative methods in health care implementation is an emerging area of best practice and can be done with varying degrees of rigor. But a rule 1 assessment should include at minimum a set of participatory queries that inform these concrete aspects of use and acceptability of interventions and the related understanding of mental health conditions.
Assessment should be ongoing. Qualitative feedback should move in parallel with what Mendel and colleagues (
46) have described as diffusion process stages—from assessment of the context for diffusion of a proven intervention (for example, attitudes, existing networks of belief and practice, and expectations), as reflected in our approach to rule 1, to features of the specific intervention captured in rules 2 and 3 (for example, acceptability, fidelity, and compatibility), and then to outcomes of the intervention and resulting change (rule 4).
Rule 2: identify and map priority care pathways
The term “care pathway” is frequently but variably used. It is used here to refer to a description of the kinds of assessments, treatments, and care tasks—and their arrangement and sequence—to effectively address a defined target condition or “case” and to meet a similarly explicit, desired health outcome. A care pathway also identifies key decision points that trigger either a change in treatment or a transition in care or further evaluation. From these, the decision supports and clinical information that are needed for a team of people to collaborate efficiently and effectively can be identified. Even though we again use depression as an example, a care pathway does not have to be restricted to a standard illness diagnostic category, as long as it captures a recognizable and relevant set of symptoms and behaviors for which there is an effective and agreed-upon intervention. Several methods, for example, have been used to efficiently design brief screening and symptom-tracking questionnaires that elicit information about locally named syndromes that may overlap with other commonly used diagnostic categories; the questionnaires can be calibrated to identify meaningful morbidity (
47). Similarly, the designation of “common mental disorders”—sometimes referred to as CMDs—has a growing literature that supports its validity in non-Western and low-income settings. The term captures a replicable endorsement of a range of depressive and anxiety symptoms with an impairing level of distress that are responsive to certain interventions.
The value of a pathway is in organizing, applying, and detailing use of the five levels of skill sets so that they achieve effective care. Distress, disordered thinking, and emotional suffering do not come in neatly defined or expressed packages. But the thoughtful adoption of pathways after adequate assessment—pathways that are chosen to capture a discernible set of locally compelling conditions and needs—can anchor decisions about training, supervision, and management across skill levels. Furthermore, a care pathway that addresses a common or priority condition can be versatile. It can serve as the foundation for an expanded repertoire of work. The ability to refer patients to, provide, and supervise interpersonal therapy for depression delivered by community mental health workers (CMHWs), for example, brings with it a platform of basic skills and supervision systems that are readily adaptable to manage a range of associated challenges, such as certain anxiety responses to trauma. These skills and systems can be iteratively developed and refined on the basis of local needs and outcomes. Given the evidence of acceptability, use, and sustained impact in Uganda (
48,
49), and from our context assessment in Haiti, we expect to use interpersonal therapy as an initial psychological intervention in these areas and probably as a foundational intervention upon which to build further skills.
An explicit pathway coordinates planning by describing needed tasks and systematically matching them to available resources. For example, Unützer and colleagues (
50) have used a systematic integrated care team building process to facilitate implementation of an evidence-based program for depression care in a diverse group of over 500 primary care clinics. A systematic approach like this clarifies which tasks can be carried out by which available staff, and it helps develop operational workflows so that diverse teams in different environments can implement similar evidence-based and effective treatments. Above we described the value of thinking in terms of a skill-defined pyramid rather than a primarily personnel-defined pyramid. Several efforts have been undertaken to creatively provide mental health skills and points of contact through health workers, teachers, religious leaders, and so forth. Shared use of care pathways that operationalize treatment guidelines can prevent such efforts from being fragments rather than integrated parts of an effective ensemble that captures the range of tasks of evidence-based care.
Making pathways explicit also clarifies the training needed for workers at each skill package level. Best practices for training mental health workers at different skill levels are emerging, including iterative manual development during training with trainees, skill practice cycles that draw on a range of reinforcement and role-play teaching, and trainee feedback about the content of training (
51,
52).
Rule 3: specify decision support tools
Pathways are not just guides for assigning tasks but allow functional, sustainable, self-reflective, and continuously improving activities. Central to that functionality are decision support tools. Simply put, these tools help an individual to know when to do something and what to do. The recent popularization of attention to checklists in medical practice and in other high-risk industries reflects the broadening application of decision supports (
53). These include clinical pathway prompts and default action requests or suggestions, and screening and evaluation methods that allow more reliable and consistent case finding, tracking of progress, and highlighting or triggering of priority tasks or triage decisions. These tools have allowed health workers to assume responsibility for a range of health tasks and established care pathways. Such tools work best when they also capture important clinical information at the point of care, especially when they are linked to other information tools. For example, cell phone-based data entry and care prompts can also feed into a larger database for aggregate reports of patterns of use, needs, or outcomes that can inform and manage quality and supervision. MVP will build on use of these technologies in the management of maternal-child care pathways to support CHW-driven care mental health care pathway functions.
Linking care steps to a clinical score or reference has been most robustly demonstrated for depression and in countries with greater resources. An instrument commonly used for this purpose, the Patient Health Questionnaire-9, has been shown to have good concordance with blinded clinical diagnoses not only in the United States but also in a number of lower-income regions, including sub-Saharan Africa (
54–
56). Furthermore, several methods for rapidly constructing scales with local validity, such as expert concordance sampling, back-translation, and scale comparison are available (
57,
58). With the addition of disability measures, it is possible to identify clinically meaningful score thresholds that can trigger referral or other actions (
47).
Training strategies for mental health skills in developing countries have only recently been studied in their own right. The MVP and ZL efforts will rely on a training-of-trainers model for the components of the pathway (intervention and relevant clinical supervision skills and use of support tools), aiming to maximize participation of local providers. Both MVP and ZL will incorporate a phased transition of supervision, which has been used in other clinical trials of psychological interventions, such as trials of interpersonal therapy in Uganda, so that training is accomplished by local personnel and will include pre-post inventory of participant learning and trainee feedback on the effectiveness and relevance of training content. A psychopharmacology manual and training materials from previous trials in developed and developing countries, adapted after context assessment, will reinforce prescriber skills and inform design of CHW and CMHW decision supports for promoting medication adherence and identifying patients who need to be seen by a prescribing provider.
Rule 4: Use quality improvement practices
Health care is increasingly expected not only to adopt proven interventions but also to routinely and consistently gather and respond to information about how well care is working in real time—both at the individual and the systems levels. This represents a transformation in health care. Provision of care that is driven by quality improvement indicators or benchmarks and adoption of rapid performance improvement cycles are ways to address this goal (
59). The extension of these methods into developing countries lags behind the developed world; however, they have been increasingly used, such as to meet MDG targets (
60–
62).
Nevertheless, use of these methods for mental health care in lower-income countries is minimal, and barely discussed. Primary care settings in several higher-income countries are using these tools to implement evidence-based mental health care for high-need, poor, safety-net populations (
63). Their role in sustainability, expansion, and adaptability of mental health services in lower-income countries, especially when incorporated into overall health systems, should receive greater attention and should be routinely advocated for and practiced as a sine qua non of further work in this field.
The ability to assess the impact of care and patient outcomes and to improve clinical, training, structural, and other features relevant to the effectiveness of care relies on making quality improvement practices an integral part of care. The implementation rules described here—especially the use of care pathways with specified tasks, supervision roles, and associated decision tools and the ways that such pathways capture information about and set goals for practice—greatly facilitate quality improvement, which, in turn, makes other features of care more effective, adaptive, and informed (
64). Organizing mental health care from the outset in a way that allows ongoing hypothesis generating and testing and shared clarity of goals across levels and workers not only contributes to more ownership, effectiveness, and adaptability of practice but addresses the tension identified above in regard to globalized implementation and advancement of mental health care: how to establish both a general base of knowledge about the nature and names of illnesses and treatments and particular knowledge of the local context in which such treatments work and are revised.
Built-in feedback for improvement is important not only for the delivery of care but also for implementation. Both MVP and ZL efforts will use structured feedback to test functionality of tasks, roles, and tools and how they work together on a small scale. Feedback will be elicited from staff as to comfort and willingness to adopt interventions, staff fidelity to protocol steps, and patient reactions. Feedback will also include actionable process measures of pathway effectiveness and skill package use and performance such as referrals to clinics, number of screens initiated by the CHW, skill retention of workers over time, percentage of patients referred by CHWs who keep appointments for mental health care, frequency of use of electronic decision supports when applicable, and percentage improvement in clinical scale scores with treatment. Clinical tool and pathway development will use well-established, small-scale, rapid improvement cycles, specifically the plan-do-study-act-PDSA-method, which has been widely adopted for organizing performance improvement that is responsive to measurable goals (
65).
Rule 5: address sustainability, capacity building, management
Increased attention from a growing number of NGOs and health ministries to providing care or training in mental health care will have limited long-term impact on treatment gaps without a focus on how to address the sustainable capacity to support these skill sets and use these rules. The efforts in ZL and MVP were designed specifically to do so. In both, existing staff within existing institutions through a training-of-trainers process will participate in training health workers and other clinical staff. Also, rule-specific tasks will be performed in tandem with local institutions in order to transfer program implementation and planning skills. In the MVP pilot, for example, agreement to the full model and to providing the roles it calls for was obtained from the Local Government Authority (for clinic resource decisions, job category specification, participation in systems-level performance improvement, and so forth), the proximate Federal Medical Center (training, referral within an established care pathway, and performance improvement and supervision roles), and health worker and clinic staff (for assuming skill sets that comprise care pathways and using decision supports).
It may be difficult for many NGOs or academic centers partnering to develop mental health services in developing countries to realize the full scope of these skill set-based care pathways and implementation rules that are being used in MVP and ZL. MVP and ZL were attractive partners precisely because they had already accomplished the “prework” of systems change in overall health services design that was locally engaged and already using a care pathway model with tiered health workers for providing general primary care. More modest approaches obviously will and should continue in low-income settings. Use of more targeted interventions to address immediate needs are inevitable in postdisaster or postconflict conditions.
However, the presence of multiple NGOs or other agencies in these settings represents a missed opportunity to lay groundwork for a more comprehensive system, including embedding and linking skill sets across the range of settings—schools, civic and religious organizations, and primary care clinics—which is essential for an effective community strategy (
66). A concise, shared nomenclature of basic tasks and programmatic steps to work toward can help realize this potential. If nothing else, a shared framework can better highlight the functions or skill packages that a particular project does not provide, so that efforts can be made to track and fill those gaps. In a process of building, or rebuilding, services, a shared and concise reference such as 5×5 can mobilize consensus and attention to what resources to ask for and build towards.
Community mental health as a global project
Low-income countries can bring together a group of people to manage the skills and rules described here, even if only in a pilot program or a single region. However, the feasibility of a scalable approach does not by itself create the resources needed to undertake it. The right framework can, however, help maximize limited resources and lend clarity and consistency across disparate funders, budgets, NGOs, and other stakeholders as to the targeted purposes and uses of needed investments in mental health. The overall MVP approach has been to build delivery capacity within credible, even if not yet realized, funding assumptions (for example, G-8 per capita pledges) that meets widely agreed-upon benchmarks (for example, the MDGs, cost per disability-adjusted life year, or illness episode averted). This approach assumes that resources will shift to where they are needed and shown to be effective. There are indications that this is happening (
67,
68). Providing care through well-meaning but fragmented projects is not sufficient. Providing care within an overall systems approach that relies on credible, sustainable funding assumptions for scale is the direction work in global health has begun to take. Global mental health efforts also need to do this well. This will require clearer planning frameworks that align disparate stakeholders along a common direction and drive relevant funding projections. The 5×5 and similar frameworks can also address the widely acknowledged need for research and technical support for operational, training, and costing strategies for scale-up of proven treatments in the developing world to work within a shared language and set of objectives (
69).
Stigma and discrimination remain obstacles to reaching people in need in every part of the world. When care is not effective or accessible, stigma proliferates. One way to overcome stigma is to engage existing opportunities to strengthen health systems, as this framework does. In our experience, lack of clarity and broad consensus about how, not whether, to act on mental health needs is too often the real obstacle. The kind of community-engaged capacity for mental health treatment described here also becomes an opportunity for earlier intervention and preventive initiatives. Finally, frameworks such as this can contribute to improved care in high-income countries. Such care is often fragmented and unresponsive to outcomes, with little matching of service mix to population need or integration with overall health care. A truly global conversation about how to structure and implement care can have truly global benefits (
12).
Acknowledgments and disclosures
The authors acknowledge the input of Pamela Collins in early discussions of this planning work.
In the 12 months before acceptance of the manuscript, Dr. Kessler was a consultant for Johnson & Johnson Pharmaceuticals, Plus One Health Management, and Shire US, Inc. He served on advisory boards for Plus One Health Management and Johnson & Johnson Pharmaceuticals and received sponsored research support for epidemiological studies from EPI-Q, Pfizer, Inc., and Shire US, Inc. Dr. Kessler owns shares in DataStat, Inc. The other authors report no competing interests.