Suicide is a leading cause of preventable death in the United States. The most recent data from 2007 indicates that the Western Mountain states continue to carry the heaviest burden of suicide in the nation (
1). A recent evaluation of state suicide rate and highest elevation demonstrated a correlation between altitude and regional variations in suicide rates (
2). Utah has remained among the top-ranked 15 states for suicide for more than a decade.
In 2001 the U.S. Surgeon General released a plan to guide the country's suicide prevention efforts over the coming decade and placed an emphasis on effective collaboration between public and private entities (
3). Many suicide prevention programs have been shown to be ineffective or have not been rigorously evaluated (
4). Suicidologists have recommended that prevention be focused on recognized high-risk populations within specific institutions (
5). Studies employing psychological autopsy methods have explored the diagnoses of suicide decedents, but a systematic evaluation of government agency contacts of decedents had never been attempted. In response to the paucity of evidence-based suicide prevention programming, the Utah Youth Suicide Study (UYSS) was initiated in 1994. [A description of the six phases of the UYSS is available in an online appendix at
ps.psychiatryonline.org.]
Phase I of the UYSS involved a study of government records of 151 youths who completed suicide to evaluate where they interfaced with government agencies. This epidemiological analysis identified a novel site of contact with the juvenile court system before death among youths who completed suicide (
6). Fortunately, Utah's Office of the Medical Examiner and Utah's Juvenile Court System each has a database that is both centralized and comprehensive. Sixty-three percent of the decedents were involved with the juvenile court system. An increased number of referrals to juvenile court was associated with an increased risk of suicide. The odds ratio for suicide completion among males referred to the juvenile court system seven or more times was 4.90 (95% confidence interval=3.27–7.35).
Government agency records were reviewed for 126 youths who consecutively completed suicide for involvement in the juvenile court and public schools (
6). Decedents were more likely to have had contact with the Utah court system (67%) than with Utah public schools (57%). School records are separate for each district; therefore, records for each decedent were searched in the geographic home school district and two neighboring districts. As in other states, many students who drop out of public school or enter private schools are not tracked statewide and are lost to the public school system.
Because of these findings, phase IV of the UYSS was developed to explore the psychiatric burden of the Utah juvenile court population. The Youth Outcome Questionnaire (Y-OQ) was administered to 719 juvenile offenders consecutively referred to the courts (
7). The Y-OQ screening tool assesses levels of psychiatric distress and dysfunction among youths and compares them with levels experienced by inpatient psychiatric, outpatient psychiatric, and community-based populations (
8). Individuals with cutoff scores equal to or greater than those of outpatient or inpatient populations merit referral. Results from this study of Utah youths referred to the juvenile court system over a one-month period indicated a high degree of psychopathology. Of 719 youths, 352 had Y-OQ scores above the outpatient cutoff score, and 17% had scores equal to or greater than the inpatient cutoff score. Furthermore, there was a positive correlation between the number of offenses and a higher Y-OQ score. From a public health perspective, the mental health community has an obligation to address the mental health needs of youths at highest risk for suicide.
Best practice: an early-intervention model for at-risk youth
Services for youths with mental illness within the juvenile court system are limited across the country (
9), and in Utah juveniles must accumulate many offenses over years before they are offered in-home services (
7). In phase V, the UYSS focused on the development of an early-intervention best practices model for mental health treatment—and by extension, suicide prevention—within the juvenile court system for young offenders with mental illness. Participants in this early-intervention pilot study included males age 13 to 16 in Utah's Third District Juvenile Court who had from two to 12 offenses. Twenty-two pairs of adolescents were matched on age, degree of mental health symptoms, and number and type of offenses. The research team agreed upon the closest match from the available group of subjects providing consent and then randomly assigned the two participants to either the treatment or control group. Participants had to have a minimum Y-OQ of 60, which is a moderate outpatient score, but those with the highest scores were prioritized.
The study protocol for the intervention group entailed provision of comprehensive, tailored, intensive, family-centered in-home services and psychiatric treatment services provided in a university mental health clinic for English-speaking males with two to 12 juvenile court referrals. Participants were excluded if they had a sex-related offense, had previously used an in-home family service, or had a diagnosis of autism or severe intellectual disability. Psychiatric assessment and treatments were conducted with provision of psychotropic medication when indicated and referrals for family or individual therapy as needed. The Families First Program provided the in-home treatment, which involved a behavior specialist who spent 80–100 hours with the family over a three-month period. Additional consultation was available for up to one year. The focus was on parenting skills and mentoring the youth. A case manager coordinated psychiatric services and completed the assessment tools. Core-team meetings were conducted to develop the treatment plan.
The 12-month study included data comparison at enrollment and at months 3, 6, 9, and 12. Outcome measurements included recidivism, days in court placement, and Y-OQ scores. Although the comparison group was not provided with treatment, parents were encouraged to seek treatment as usual in their community.
Y-OQ scores indicated significant improvement in the intervention group versus the comparison group (p<.001); the relative daily change in Y-OQ score for the intervention group versus the comparison group was −.073 (p=.007). [A description of the effect sizes is provided in the online appendix at
ps.psychiatryonline.org.] In addition to improved mental health status, the intervention group showed a trend (p=.22) toward decreased recidivism. Recidivism was defined as participating in one or more offenses after enrollment for 12 months. Seventy-seven percent of the intervention group did not reoffend after a year, compared with only 57% of the comparison group (p=.22). Of interest, reoffenses committed by youths in the intervention group were the same or lower-level offenses compared with those committed by youths in the control group. Youths in the control group had higher-level reoffenses, including violent offenses, such as assault.
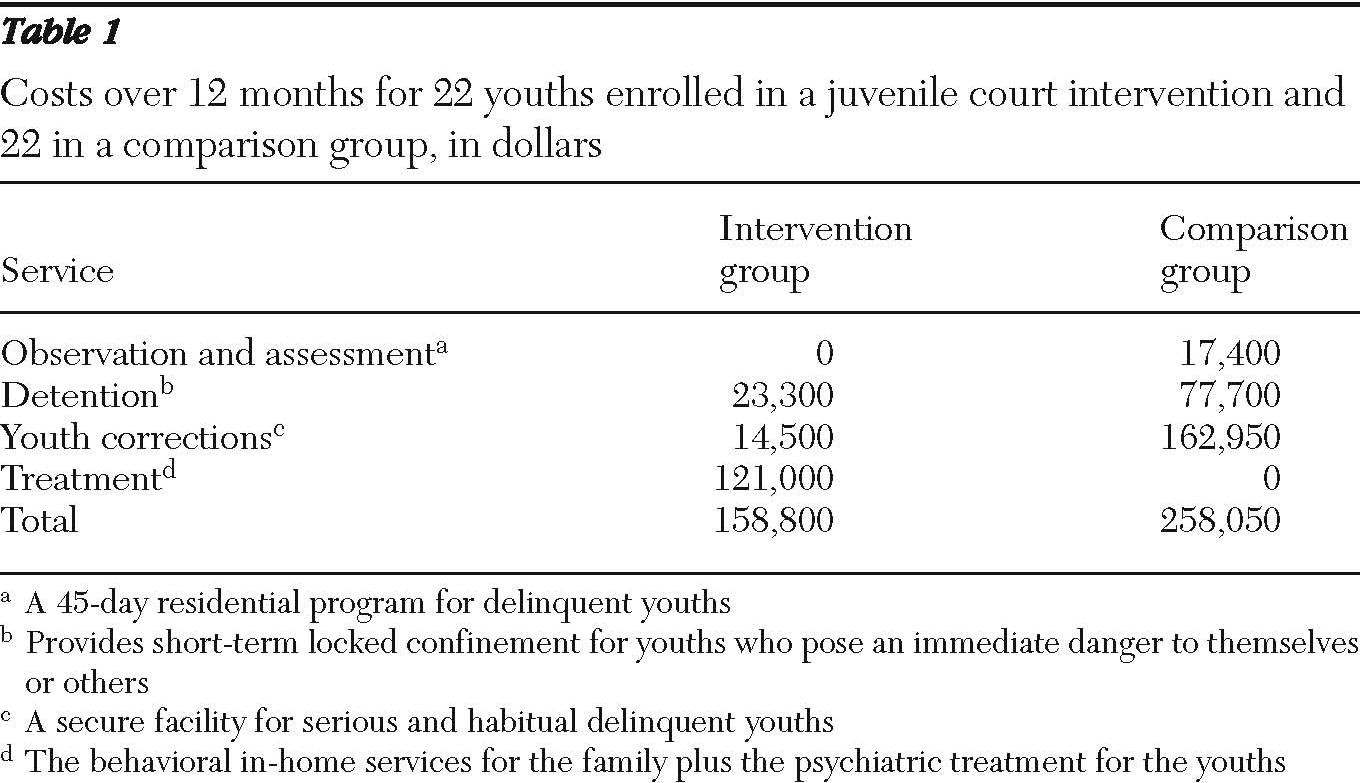
As shown in
Table 1, there were marked cost differences between the intervention and comparison groups at 12 months. The treatment services provided to the intervention group cost $121,000. However, if taking into account the cost of days spent in observation and assessment, at detention centers, and at correctional facilities, the total costs for the comparison group at 12 months was $258,050, compared with the total cost, including treatment, for the intervention group of $158,800. The comparison group spent significantly more days in correctional facilities than the intervention group (490 versus 58; p<.01) and in observation and assessment (87 versus 0; p<.04). Additional societal costs included the number of workdays that parents missed because of participants' misconduct, which totaled 82 days for the intervention group and 124 days for the comparison group.
Expanding the best practice reach
Encouraged by the reduction in psychological distress and dysfunction and in recidivism among high-risk youths in the juvenile court treatment group, funding was acquired in 2006 via a three-year grant from the Substance Abuse and Mental Health Services Administration (SAMHSA) under the Garrett Lee Smith Memorial Act. The monies were utilized to expand upon this best practices model by including all offenders within the state's Third District Court system (covering metropolitan Salt Lake City and two neighboring counties). The goal was to evaluate whether an evidence-based psychiatric treatment model for at-risk teenagers in the juvenile court could be expanded to a larger population.
Over 2,000 adolescents volunteered for computer screening at multiple sites over the three-year SAMHSA grant (2006–2009). A total of 803 adolescents screened positive (Y-OQ score of ≥46 or suicidal ideation), and their parents were notified. Only 192 (21%) initiated contact with the case manager. Of those who requested treatment, only 73% continued at the psychiatry clinic after the initial evaluation and recommendations. The remaining participants demonstrated an average reduction in Y-OQ score of 33 points during the time they were enrolled in the grant-funded program. An 18-point reduction is considered a significant improvement (
8). For the adolescents in treatment, 74% became less suicidal over time, 13% stayed the same, and 13% got worse. The goal of expanding the model to larger populations was achieved, and many lessons were learned to help guide future service implementation.
Discussion
To our knowledge, Utah is the only state to allow suicidologists access to data on suicide decedents from all state government agencies. A limitation of this study was the lack of a statewide Department of Education student database. In addition, Utah has a relatively homogeneous population that is disproportionately white and of the Mormon faith, warranting caution when extrapolating the results to more culturally diverse states. The low participation rate may be a reflection of the high level of psychosocial stress experienced by families with adolescents in the court system. Future programs should focus on enhancing voluntary participation and should consider mandatory treatment for the highest-risk individuals.
Nevertheless, multiple studies have concluded that most youths who complete suicide are not receiving psychiatric treatment or taking psychotropic medications at the time of death (
6,
10–
12). The UYSS findings indicate that juvenile offenders with multiple referrals are at highest risk for suicide completion, and yet mental health resources have not been directed nationally to this vulnerable population. The juvenile court system is unique in its ability to maintain contact with juveniles on probation through their 21st birthday. Thus it is the best portal for mental health screening and referral of high-risk youths for appropriate mental health treatment as part of a suicide prevention effort.
Conclusions
Historically, U.S. programs for suicide prevention among adolescents have focused on public schools (
13). One of the most important findings of the UYSS was that adolescents who completed suicide were often in contact with the juvenile court system. Furthermore, youths in this system were at increased risk of suicide as the number of offenses increased. Undertreated offenders with mental illness can be readily identified with the Y-OQ at an early stage of their interface with the juvenile court system. A novel program for the treatment of juvenile offenders with mental illness was found to be successful and was then integrated into a large government agency.
Acknowledgments and disclosures
The authors thank the following individual contributors: Brandon Callor, for coordination at the Utah Office of the Medical Examiner; Michelle Moskos, Ph.D., epidemiologist, for project development; Ray Wahl, administrator for the Utah Third District Juvenile Court; Steve Alder, Ph.D., Department of Family and Preventive Medicine, University of Utah, for statistical analysis; Sarah Halbern, M.S.P.H., research analyst; Wayne Arner and the Families First in-home program; and Gary Burlingame, Ph.D., Brigham Young University, for use of the Web-based Youth Outcome Questionnaire. The Utah Youth Suicide Study started in 1994 with funding from the Utah Department of Health.
The authors report no competing interests.