In European countries, such as the Netherlands, the number of compulsory psychiatric admissions has been rising since the 1990s (
1–
4). In the Netherlands, the increase includes both orders by the mayor for compulsory admission in emergency situations and involuntary admissions after recourse to the courts (court orders) (
4). The procedure for emergency compulsory admission has been described elsewhere and has much in common with the procedure for emergency detention under section 4 of the United Kingdom's Mental Health Act of 1983 (
5,
6).
In the Amsterdam area, the number of emergency compulsory admissions increased by 319% to 86 inhabitants per 100,000 population between 1979 and 2004 (
7). It is clear that this is an undesirable trend, resulting in negative experiences for the patients and a reduction of patient autonomy. Therefore, it is important to look for opportunities to curb emergency involuntary admissions by controlling risk factors.
Previous research has identified a diagnosis of psychotic disorder or manic episode, immigrant background, and a history of involuntary admission as risk factors for involuntary admission (
8). Several studies have found an inverse relationship between social network size and use of inpatient services among patients with psychotic disorders (
9–
11). So far, however, very little is known about the social and family background of patients admitted compulsorily. Do the quantity and quality of social support affect the risk of emergency compulsory admission for patients with a severe psychiatric illness?
One study in the United Kingdom showed that living alone with little or no contact with others raised the likelihood of emergency detention under section 4 of the Mental Health Act of 1983 (
6). However, the study's retrospective approach, including retrospective assessment of the social support factor, makes the outcome of this study less reliable.
In this study, part IV of the Amsterdam Study of Acute Psychiatry, we prospectively investigated a cohort of patients who had an emergency consultation in Amsterdam. We sought to determine whether the size of the social networks and the amount of social support and negative interaction reported by patients predicted emergency compulsory admission during follow-up. We hope that this study opens avenues for adapting treatment programs for this group of patients by focusing on the enhancement of social support to prevent unnecessary compulsory admissions and readmissions.
This study tried to answer the following questions: Are patients who live with other people less likely than patients who live alone to undergo an emergency compulsory admission? What is the influence of one's domestic situation (living alone or with others) on the relationship between network size and risk of emergency compulsory admission? What influence does domestic situation have on the relationship between subjective, qualitative aspects of social support, both positive and negative, and risk of emergency compulsory admission?
Methods
Study design and setting
This study was part of a prospective cohort study of all consecutive patients who received emergency consultations from the Psychiatric Emergency Service Amsterdam (PESA) and from the Acute Treatment Unit (ATU) between September 15, 2004, and September 15, 2006 (
5). The PESA is the main decision-making body for emergency compulsory admissions in the Amsterdam area (about 743,000 inhabitants). It provides 24-hour psychiatric emergency services, seven days a week. The ATU is a specialized outpatient emergency service that covers the Centre and Old West area of Amsterdam (about 200,000 inhabitants); it provides services during office hours only. Patients are referred by family doctors, police, emergency wards at general hospitals, and mental health care workers. During office hours, ATU takes the referrals of family doctors and mental health care workers within the specific catchment area. The PESA handles police referrals 24 hours a day. Three other catchment areas in the city are served by ATUs not covered by our study.
People who come into contact with the police are first screened at the police station by a community mental health nurse from the City Health Service. Individuals in need of immediate psychiatric consultation are brought by the police to the PESA's psychiatric emergency room. Patients who are referred to the PESA or the ATU by primary health care providers, such as family doctors or doctors from emergency wards, are often seen in their homes or at the referring emergency ward. Patients themselves have no direct access to consultations without a formal referral. In general, consultations are conducted on workdays between 9 a.m. and 10 p.m. by a team of residents, community mental health nurses, and a psychiatrist. Psychiatrists play an active role during consultations, either by acting as a supervisor or by seeing patients themselves. At other times, residents and a nurse work together during the consultations, and psychiatrists provide telephone backup. The PESA and the ATU use electronic patient files.
Criteria for inclusion
Two groups of participants were selected at random from among the patients who had at least one consultation with either the PESA or the ATU during the study period. One group consisted of patients whose consultation resulted in compulsory admission, and the other group consisted of patients whose consultation resulted in voluntary admission to a psychiatric hospital or crisis center, in outpatient treatment, or in no further intervention. Every patient in the compulsory-admission group and every fourth patient in the other group were asked to participate in the study. For pragmatic reasons we selected only patients with a fixed abode in Amsterdam whose command of Dutch was sufficient to permit them to be interviewed without an interpreter. We excluded people living elsewhere in the Netherlands or abroad and people with no known place of residence.
Measures
We collected three types of data. First, the clinician collected data during the emergency consultation about the patient's age, gender, domestic situation, and DSM-IV-TR axis I diagnosis. We used four clusters of categories: schizophrenia or other psychotic disorder, manic state, depressive disorder, and other or no disorder. The last group included drug- and alcohol-related disorders if they were the patient's main axis I diagnosis, a wide variety of other diagnostic categories, and psychosocial problems in the absence of a DSM axis I disorder. The outcome of the consultation was also recorded.
Second, data were collected by research assistants during an interview approximately one month after the emergency consultation. The research assistants were five trainee psychologists and a team leader who graduated in human geography with experience in mental health care research. The entire process was supervised by the first author. During the interviews we counted the number of people in the patients' social network by using the Social Network Structure Questionnaire (SNSQ) developed by van Sonderen (
12). This Dutch ten-item self-report inventory maps the natural networks of people (partner, family, neighbors, coworkers, and people at school) who play a role in the patient's life. The SNSQ assesses the quantitative aspect of social support. We also used the 13-item Social Resources Questionnaire from the Multidimensional Health Profile (MHP) that was developed and validated by Ruehlman and colleagues (
13). This self-report screening instrument evaluates positive and negative aspects of social interaction, by including nine items that assess social support (possible scores of 9 to 45) and four items that assess negative social exchange (possible scores of 4 to 20). A score between 11 and 20 on negative social exchange implies a high level of negative interaction with family or friends.
Third, we collected data about the number of emergency compulsory admissions of each patient recorded in the Amsterdam Mental Health Care database during the two-year period after the interview.
Data analysis
We expected a clinically relevant difference between the voluntary and compulsory groups, and an effect size of approximately .5. To detect a difference of this kind in effectiveness between the groups (α=.05 and β=.80), 64 respondents were needed in each group. Because we expected a considerable level of dropout (50%) between the inclusion stage and the final follow-up measurement, we estimated that 125 patients per group would be required initially.
A bivariate analysis with a Pearson chi square test and an independent-samples t test for variables with normally distributed values or an independent-samples Mann-Whitney U test for variables with values that were not normally distributed was conducted to examine differences in sociodemographic factors, clinical presentation, mean sum scores on the SNSQ and the MHP Social Resources Questionnaire among patients with and without at least one emergency compulsory admission during follow-up. A bivariate analysis with Pearson chi square testing to examine the relationship between the patients' domestic situation and the number of members of their social networks was also conducted.
To prevent bias by intercolinearity in our multivariate analyses, we checked for the presence of couples of variables with a contingency or correlation coefficient greater than ±.6. To analyze the influence of effect modification, we conducted two multiple stepwise logistic regression procedures with the variables that were found by the bivariate analysis to be correlated (p≤.15) with having at least one emergency compulsory admission during follow-up.
We calculated the odds ratios (with a confidence interval [CI] of 95%) for the incidence of emergency compulsory admission during follow-up and scores on the SNSQ and MHP Social Resources Questionnaire, domestic situation, and their interaction terms. For interaction terms that proved to be significantly associated with the outcome measure, further analysis of the modification effect was conducted by means of bivariate analysis with Pearson chi square testing of the association between the SNSQ and MHP scores for patients who lived alone or with other people.
Finally, we conducted a multiple stepwise logistic regression procedure with the variables found by the bivariate analysis to be correlated (p≤.15) to develop a prediction model. First, we calculated the odds ratios and CIs for the incidence of emergency compulsory admission during follow-up by using numbers of network members as predictors. In the second step, the subscales of the MHP for social support and negative interactions were added. Domestic situation was added in the third step of the analysis.
Before introducing variables to the logistic regression analyses, we tested all possible couples of independent variables for intercolinearity by calculating the contingency coefficient for nominal-nominal or nominal-ordinal couples, eta for nominal-linear couples, Spearman's rho for linear-ordinal couples, and Pearson's correlation for linear-linear couples. We used SPSS, version 19, software.
Informed consent and data security
Patients randomly selected for the study cohort received a letter with a request to participate in the study. In the follow-up to this request, patients were contacted by a research assistant by telephone, in writing, or in person at the patients' place of residence. As a result, patients received information verbally as well as in writing before they were asked to give written informed consent. The procedure was endorsed by the Medical Ethics Committee for Mental Health Care Institutions. Confidential information and participants' names were subject to medical confidentiality rules and were handled in accordance with the code of conduct for medical research developed by the Federation of Biomedical Scientific Societies.
Results
Composition of the study cohort
A total of 2,682 patients had at least one emergency consultation during the study period, and a group of 954 patients, evenly divided among those who had or had not been admitted compulsorily, were randomly approached and asked to participate in the study. Of those, 317 patients (33%) could not be contacted in spite of repeated phone calls or home visits; 243 (25%) refused to participate; 99 (10%) were too ill as a result of a psychiatric or general medical condition to give informed consent; 28 (3%) could not give informed consent because they did not speak sufficient Dutch and 15 (2%), including three who died before they could be contacted, did not give informed consent for various other reasons. This left a study cohort of 252 patients, 118 with and 134 without an emergency involuntary admission. Half the patients were interviewed within six weeks of the emergency consultation, and 75% were interviewed within ten weeks. Eight patients died or left the country during the first year of follow-up, leaving a follow-up cohort of 244 patients.
Representativeness testing and selection bias
The study cohort of 252 patients was compared with the 2,430 patients who fulfilled the inclusion criteria and were not included in the follow-up study. We conducted separate representativeness tests for the compulsorily admitted sample (N=118) and for the sample in which consultation did not result in involuntary admission (N=134). We compared each sample with the part of the population from which it was drawn.
Among patients admitted compulsorily, members of the study cohort were significantly younger than nonmembers (38±11 versus 43±17, p≤.001), and a smaller percentage were classified as psychotic (58% versus 70%, p≤.01). There were no significant differences between the groups in gender, country of origin, and domestic situation. Among patients who were not admitted compulsorily, the proportion of native Dutch was larger (75% versus 60%) and the proportion of non-Western immigrants was smaller (16% versus 34%) in the study cohort than in the population as a whole (p≤.001). There were no significant differences between the groups in gender, age, domestic situation, and diagnostic category.
Emergency compulsory admissions during follow-up
Sociodemographic and clinical characteristics.
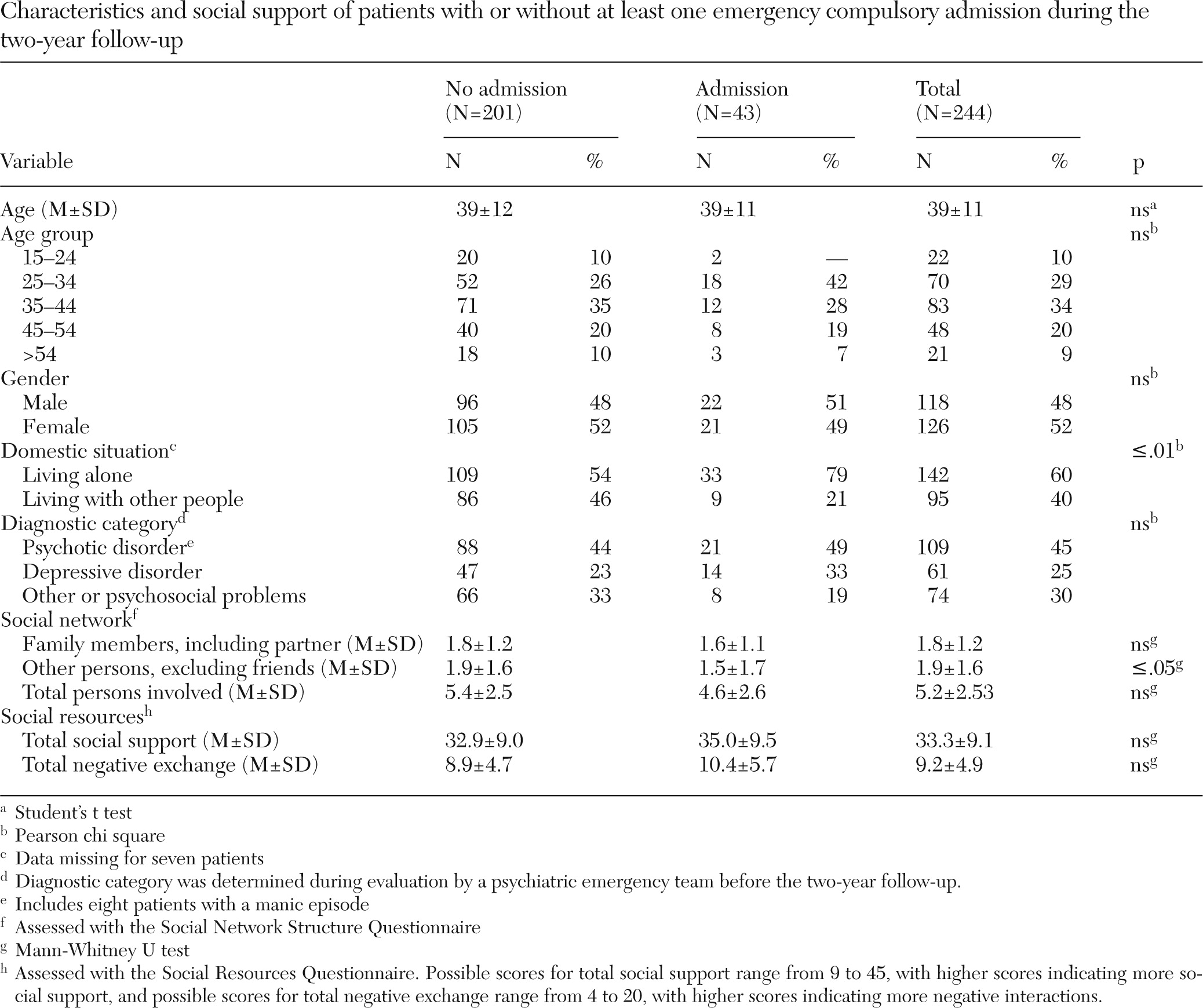
There were no significant differences in gender, age, or diagnostic category between patients with or without at least one emergency compulsory admission during follow-up (
Table 1).
Social support.
The percentage of patients who had an emergency compulsory admission was significantly greater among patients who lived alone than among patients who lived with others (79% versus 21%, p≤.01). There were no significant differences between the two groups in the total number of persons involved or of family members involved in the patients' social networks. However, patients with at least one emergency compulsory admission during the follow-up had significantly fewer persons other than friends and family involved in their social networks (1.5 versus 1.9, p=.037). Pearson's product-moment correlation indicated that the total number of people involved and the number of persons involved other than friends or family in the patients' social networks were highly correlated (r=.759, p≤.01). To avoid bias by intercolinearity, the total number of persons involved was left out of the final prediction model.
Neither the social support subscale nor the negative social exchange subscale of the MHP Social Resources Questionnaire showed significant differences between patients with or without an emergency compulsory admission during the follow-up period.
Social support and domestic situation.
The mean±SD total number of people in a patient's social network was significantly higher among patients who lived with other people than among patients who lived on their own (6.1±2.6 versus 4.6±2.3, p≤.001). There was no significant association between domestic situation and scores on the two subscales of the MHP Social Resources Questionnaire (data not shown).
Predictors of outcomes.
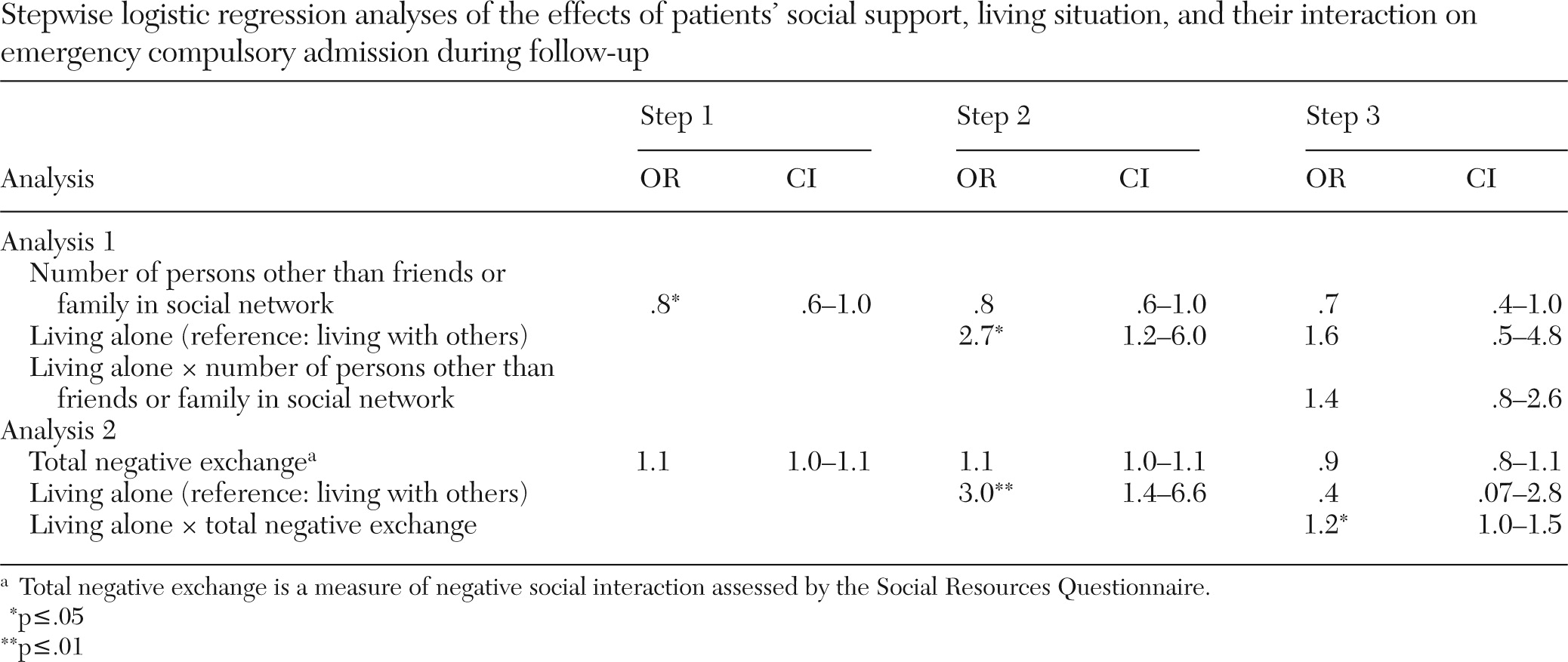
Stepwise logistic regression analysis of the number of persons involved other than friends or family, domestic situation, and their product term as predictors of outcome showed that neither variable alone, if adjusted for each other, nor the interaction term had a significant association with outcome (
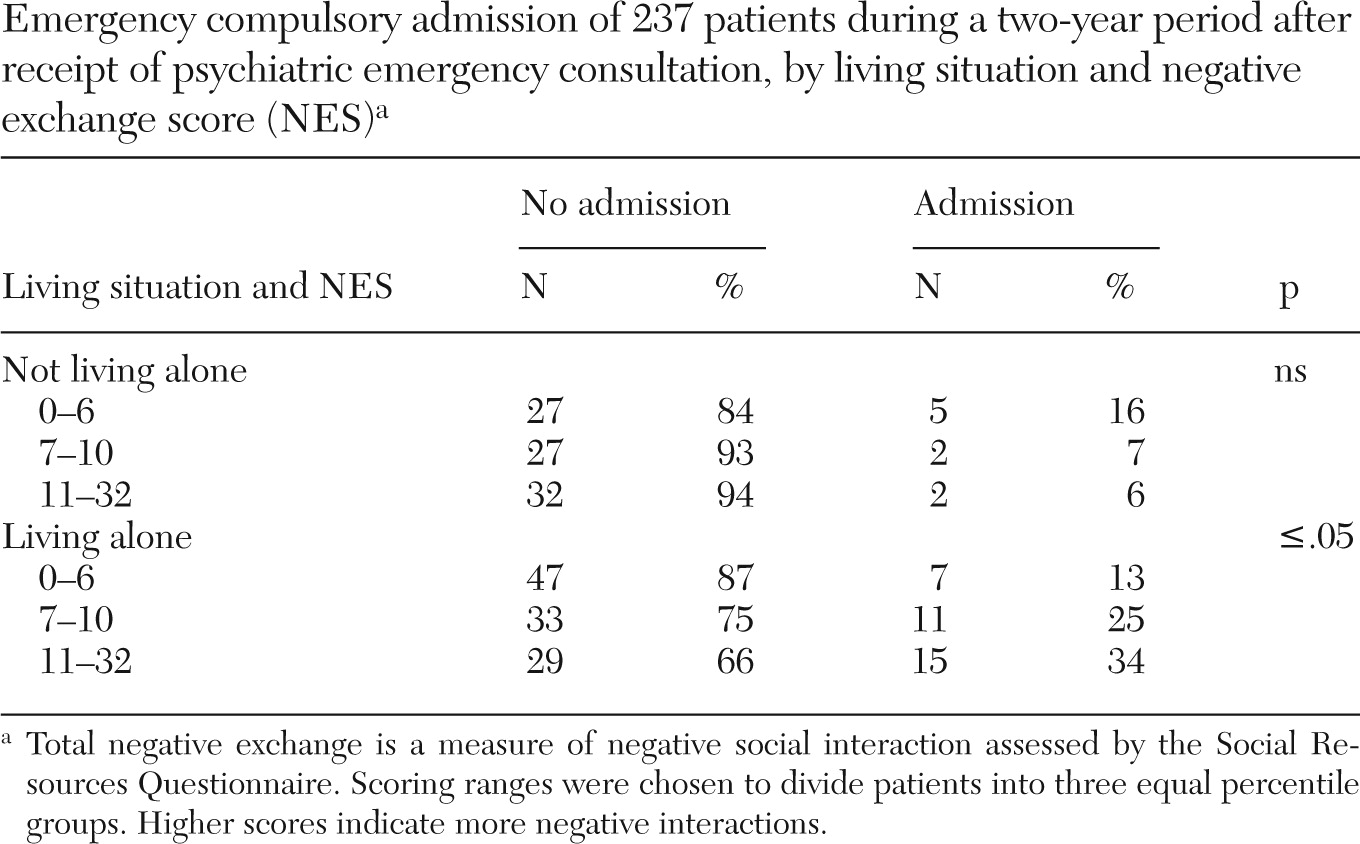
Table 2). The logistic regression analysis of negative exchange, domestic situation, and their product term as predictors of the outcome showed that when adjusted for the other two variables, the interaction term was significantly associated with outcome (p≤.05). Bivariate analysis of this relationship showed that risk of compulsory admission among patients who lived alone was significantly higher among patients with a high score for negative interactions than among patients with a low score (p≤.05) (
Table 3). There was no significant association between scores for negative interactions among patients who lived with others.
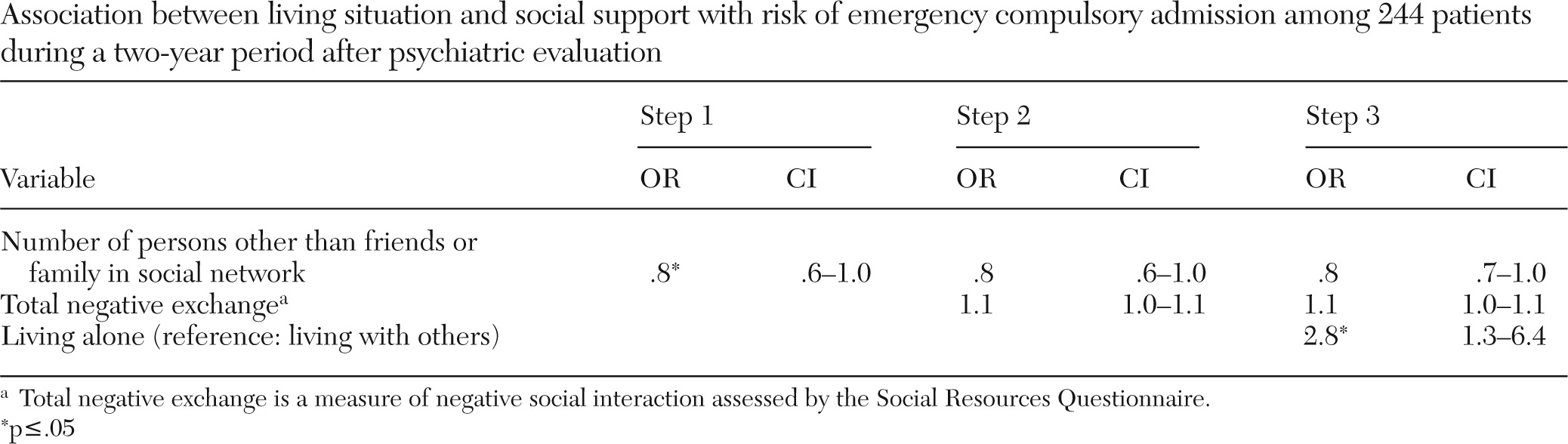
The final prediction model showed that having more persons involved other than family or friends was associated with a significantly lower probability of emergency compulsory admission during follow-up (p≤.05) (
Table 4). This association was no longer significant after the score on the negative social exchange subscale of the MHP Social Resources Questionnaire was added to the analysis. Negative social exchange by itself also was not associated in this two-variable model with the risk of emergency compulsory admission during follow-up. Adding domestic situation in step 3 of the model showed that living alone was the only independent variable that was associated with a significantly higher risk of emergency compulsory admission during follow-up (p≤.05).
Discussion
Three major findings emerged from this study. First, of the social support variables, living alone proved to be the only independent predictor of emergency compulsory admission or readmission. Second, patients who lived alone proved to have a smaller social network. However, network size itself was found to have no independent impact on the risk of compulsory admission. Third, a high level of reported negative interactions with other people also exacerbated the risk of compulsory admission, but only among patients who lived on their own.
The fact that domestic situation proved to be an important predictor of emergency compulsory admission concurs with earlier findings. A study in the United Kingdom showed that living alone with no or little contact with others raised the likelihood of emergency detention under section 4 of the Mental Health Act (
6). In our study, however, the likelihood of compulsory admission during follow-up was not related by itself to the size of the network, most probably because the variables of network size and living alone were colinear to some extent. On average, patients who lived with others had a larger social network.
How exactly living alone, in combination with social network size, influences the risk of emergency compulsory admission is not clear. It is possible that the day-to-day presence of a partner or family member prevents psychiatric crises. One possible mediator of the impact of this presence may be the extent to which family members or partner help the patient stick to his or her treatment and adhere to prescribed medication. Earlier research found a relationship between network size and medication adherence, at least for patients with schizophrenia (
14,
15). This hypothesis merits further investigation, for example, through exploration of the relationship between living situation and treatment continuity, adherence to medication, and emergency compulsory admission and readmission.
Criticism by family members of patients with schizophrenia is associated with earlier first and second readmissions and with a higher rate of readmission (
16). Therefore, we expected scores for total negative exchange to be associated with a higher risk of emergency compulsory admission in our cohort also. On one hand, we found no independent relationship between the subjective, qualitative aspects of social support, either positive or negative, and the risk of emergency compulsory admission. On the other hand, a high score for negative exchange made compulsory admission during follow-up more likely, but only for people who lived on their own.
Domestic situation clearly modified the effect of negative interactions. It appears that patients who lived on their own were more vulnerable to negative interactions. This may be because their networks, on average, were less extensive. For example, seven good relationships may protect an individual from the stress caused by one or two bad relationships. If an individual's network happens to be small, the impact of negative exchanges may be much higher. More research is needed to understand better the balance between supportive and negative interactions.
The strengths of our study were the prospective design, the long follow-up period, and, in particular, the extensive assessment of patients' views about their social networks. This study suffered from a few minor limitations. First, individuals with psychosis were underrepresented in the compulsory admissions cohort. Second, non-Western immigrants were underrepresented in the cohort of patients who did not have a compulsory admission during the follow-up. Research indicates that the risk of compulsory admission is higher among some non-Western immigrant groups (
17–
19).Therefore, we may have failed to include enough patients with a high risk of compulsory admission during follow-up. However, it is unlikely that these small underrepresentations of patients with psychosis and of non-Western immigrants affected the outcome related to the association between social support and the risk of emergency compulsory admission.
Conclusions
This is the only study of which we are aware that has linked patients' views about their social networks and emergency compulsory admissions in a prospective, two-year follow-up. Of the social support variables, living alone proved to be the only predictor of emergency compulsory admission and readmission, and patients who lived alone had a smaller social network. A high level of negative social interactions increased the risk of compulsory admission among patients who lived alone. More research is needed to clarify the role played by a lack of social support as a predictor of emergency compulsory admission.
Acknowledgments and disclosures
The authors thank ARKIN Mental Health Care, Amsterdam, for financial support. The study was also supported by a grant from the Foundation for Support VCVGZ, Arnhem, the Netherlands. The authors thank the emergency psychiatric clinicians from the Psychiatric Emergency Service Amsterdam and the Acute Treatment Unit for their participation in the study.
Dr. Dekker and Dr. Beekman report receiving research grants from Eli Lilly and Company. Dr. Beekman also reports receiving grants and research support from Astra Zeneca, Janssen, and Shire and has served on the speakers bureaus of Lundbeck, Eli Lilly, and Continuum Psychiatrie. The other authors report no competing interests.