Hospitalization is a potential performance measure that can be reliably measured in most health care systems. As a result it has been used in some studies as an outcome measure. A recent review of hospitalization as an outcome measure for schizophrenia services concluded that it is a good proxy outcome measure in randomized controlled trials (
1). Hospitalization has a significant impact on the lives of patients and families and reflects a clinical event that carries significant societal costs. It is influenced by a number of important process measures, including medication adherence and family education. Hospitalization as an outcome measure has been criticized because it reflects a negative outcome and implies a preoccupation with system-level costs rather than patient-centered outcomes (
1). Despite the potential value of hospitalization as a performance measure for mental health services, very little has been published about the relationship between it and other outcome measures. No published studies have examined the relationship between hospitalization in schizophrenia and clinical outcomes such as symptoms and quality of life. A positive relationship between hospitalization and other outcomes has been found in a prospective cohort study of patients with posttraumatic stress disorder (
2) but not in a study of patients with substance abuse (
3).
Hospitalization has been identified as an evidence-based performance measure of follow-up services associated with a first episode of psychosis (
4). It has been used as the primary outcome measure in a study to support establishing standards of care and as the primary outcome measure for a first-episode psychosis study of specialized treatment teams (
5,
6). A risk adjustment model for hospitalization in first-episode psychosis has been published to facilitate comparisons across different services (
7). We found no studies that have examined the relationship between hospitalization and other outcome measures in this population.
Methods
We used a prospective cohort design to assess the relationship between hospital admission, quality of life, and general psychopathology in a cohort of 606 persons who had had a first episode of psychosis and were followed over two years, between 1997 and 2003. Participants were enrolled into a first-episode psychosis program that serves a designated population.
Inclusion criteria were meeting criteria for schizophrenia or schizoaffective disorder as defined for DSM-IV diagnosis codes 295.10, 295.20, 295.30, 295.60, 295.90, or 295.70 and being between ages 18 and 65. Exclusion criteria included having more than three months of treatment with antipsychotic medications, mental retardation, not speaking English, having a major progressive medical or neurological disorder, and being younger than 16 years or older than 65 years.
The research project was approved by the local conjoint research ethics committee. In accordance with the local Health Information Protection Act and ethics committee guidelines, individual patient consent was not required because the project used deidentified data from administrative and clinical databases. All admissions to local hospitals are recorded in a single database.
We compared participants who were admitted with those who were not admitted. All participants were individually assessed at the time of enrollment into the program and then reassessed one and two years later. Clinical measures used in the assessments included the Quality of Life Scale (
8) and a measure of global psychopathology, the Positive and Negative Syndrome Scale (PANSS) (
9). Possible Quality of Life scores range from 0 to 126, with higher scores indicating higher functioning and better quality of life. Possible PANSS scores range from 23 to 161, with higher scores indicating higher levels of psychopathology. Participants were rated on clinical measures by clinicians trained to achieve an 80% agreement with a gold standard for taped and rated interviews. Information about hospitalization was collected from the regional administrative database.
We first examined the bivariate relationship between the demographic, socioeconomic, and clinical characteristics; quality of life; and hospitalization. The clinical assessments were conducted at fixed time points, specifically one year and two years after program enrollment. The hospitalization could occur at any point during the year. Significant variables in bivariate analysis were included in multivariate logistic regression modeling. Stepwise deletion was used to determine the factors to be retained in the final model. Statistical analysis was conducted in three steps with Stata, version 9.0 (
10).
Results
The baseline sociodemographic and clinical features of the sample are reported elsewhere for a study that used the same cohort (
7); 65% (N=396) of the sample were male, 82% (N=498) were single, 52% (N=317) had at least a high school education, 82% (N=502) were living with spouses or families, and 54% (N=328) were students, employed, or in a formal homemaker role. Seventy-one percent (N=424) were white, 14% (N=56) Asian, 2% (N=13) Latino, 3% (N=19) black, and 1.6% (N = 10) Native American.
Not all participants were assessed at one year and two years because some were discharged from the program and some missed an assessment. We compared those who were assessed and those who were not assessed on baseline demographic and clinical characteristics. There were no statistically significant differences between the groups other than age on program entry. Compared with those who were not assessed at both time points (year 1 and year 2), persons who received both assessments were slightly older (year 1, 26.4 years versus 24.1 years; year 2, 26.8 years versus 24.4 years) (p<.001).
Among the participants, 54% (N=325) were hospitalized before enrollment in the program. Twenty percent (N=122) were admitted during year 1, and an additional 13% (N=77) were admitted in year 2, for a cumulative 33% two-year hospitalization rate.
Those who were hospitalized in their first year differed significantly on Quality of Life score from those who were not hospitalized (N=78 hospitalized, mean±SD score=63.7±21.1; N=315 not hospitalized, score=72.7±23.7; t test p=.002) and at year 2 (N=40 hospitalized, 62.7±18.8; N=254 not hospitalized, 74.4±22.9; t test p=.002). The two groups also differed significantly on global psychopathology (year 1 PANSS score=54.5, interquartile range [IQR]=48–66, versus 51.0, IQR=41–63, Mann-Whitney p=.01; year 2 PANSS score=56.5, IQR=47–71, versus 52.0, IQR=39–63, Mann-Whitney p=.02).
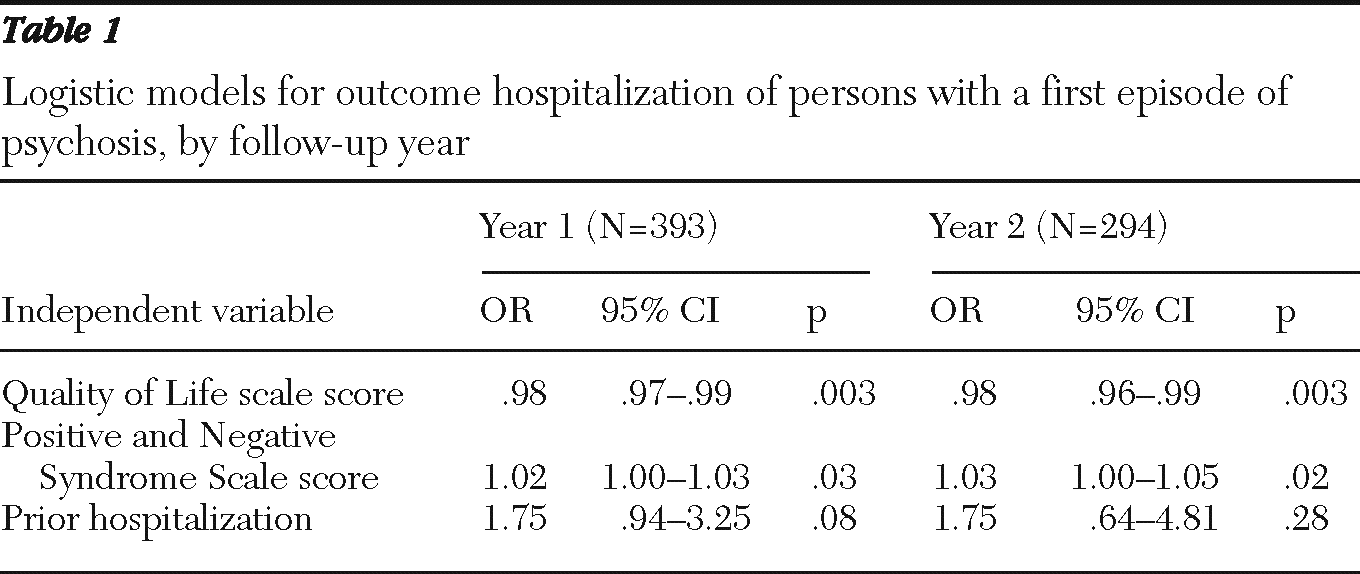
We developed three multivariate logistic regression models for each assessment (year 1 and year 2 follow-ups). The results are presented in
Table 1.
Discussion
This study demonstrated a statistically significant relationship between quality of life, global symptoms, and hospitalization of participants with a first episode of psychosis. These relationships persisted even when prior hospitalization was included in the regression model. Only 54% of these participants had a hospital admission prior to enrollment in the first-episode program, so outcomes reflect a whole system of care, including inpatient services, emergency services, and outpatient services. These results demonstrated a correlation between hospitalization and clinical measures but did not prove a causal relationship. It is possible that both baseline characteristics (
7) and process or treatment variables (
11,
12) interacted to affect all outcomes. However, it is beyond the scope of this study to separate out the impacts of these variables. This finding is congruent with results of a study of posttraumatic stress disorder (
2) but not with findings in a sample with substance abuse (
3). Our study differed from these studies in two important ways: first, because the participants in this study had a first episode of psychosis, and second, because in the other studies all patients started out hospitalized.
A limitation of the study was that it examined data from only one region; however, this health system is typical of other publicly funded mental health systems in Canada. Another limitation was that clinical data were not available for all participants, which was addressed by comparing baseline characteristics of those who were and were not admitted.
Conclusions
We have demonstrated that hospitalization of patients with a first episode of psychosis was related to two important independent clinical measures, quality of life and global psychopathology. This is the first such published report for a population experiencing first-episode psychosis and adds to the validity of hospitalization as an outcome measure for first-episode psychosis services.
Acknowledgments and disclosures
This study was funded with a grant from the Alberta Heritage Foundation for Medical Research, Health Services Research Fund.
The authors report no competing interests.