Awareness of the role played by social support in the etiology and course of medical disorders has led to profound changes in care. Since the 1970s, mental health practitioners have focused on psychosocial treatment in addition to pharmacology. This trend was influenced by the observation that poor social support is linked with higher mortality (
1,
2) and poorer mental health outcomes (
3,
4).
Social support is defined as the belief or perception that one is cared for, is esteemed, and belongs to a social network (
5). Whether one feels supported is likely to depend on several dimensions. These include the size and density of the social network, otherwise known as the structural dimension; the individual's judgment of the adequacy of the social network, or the functional dimension; and the source of support—whether family, friends, or others (
6,
7). It is important to distinguish these dimensions because there is evidence that they play separate roles in promoting health or alleviating stress. For example, a study of depression among individuals with or without arthritis found that the structural aspect of the social network had a direct protective effect on health and that the network's functional aspect interacted with stress to alleviate depression (
8).
The role of the social network is different in schizophrenia than in other mental illnesses, such as depression. In most cases, persons with schizophrenia experience social dislocation, having lost their place in a network (
9,
10), and in many cases, they experienced social disadvantage and isolation long before their first presentation to services (
11,
12). Compared with the networks of those without schizophrenia, the social networks of individuals with schizophrenia have fewer members (
13,
14); have fewer subgroups (
15); have more unsupported connections (
16); give less satisfaction than desired (
17); and because patients are usually on the receiving end, are less reciprocal (
18).
The networks of persons with schizophrenia typically deteriorate over time (
19) and eventually are dominated by mental health practitioners instead of family and friends (
20,
21). A Quebec study showed that compared with welfare recipients, individuals with schizophrenia have better quality of life in terms of finances and other material domains but are less satisfied with the social support they receive (
22). In summary, low social support characterizes the lives of patients with schizophrenia throughout the course of their illness.
Assertive community treatment (ACT) increasingly has been studied as a mode of treatment for severe mental disorders (
15). It is characterized by an interdisciplinary team, low patient-to-staff ratios, and high availability of individualized care (
23). Several studies have demonstrated that ACT results in fewer hospital readmissions (
24), better medical compliance (
25), longer periods of sustained contact with the care team (
25–
27), and a reduction of homelessness (
28). However, these findings were not consistent across all studies (
29).
Despite the advantages of ACT, few studies have examined its influence on social support of patients with schizophrenia. Two reviews of the literature about ACT interventions up to 2001 (
23,
30) found that only three of 13 studies reported better social adjustment, defined as quality of social relationships and meeting role expectations, among individuals with schizophrenia.
Since 2001, at least four studies have compared social outcomes among individuals who received ACT or standard care. Two reported that the individuals enrolled in ACT had better social outcomes (
25,
31), but the other two found no differences in the social outcomes of the two groups (
27,
32). In Sweden, the availability and adequacy of attachment among mental health patients assigned to comprehensive case management improved at six-year follow-up (
31). Likewise, in the Lambeth Early Onset (LEO) trial in the United Kingdom (
25), compared with patients in standard community care, a higher proportion of patients in ACT were able to resume or maintain relationships.
By contrast, the Randomized Evaluation of Assertive Community Treatment (REACT) study (
32), in London, and an ACT study in the Netherlands (
27) reported no significant difference in social outcomes among patients in ACT or standard care. Some ACT studies have used measures of social outcomes that are not immediately concerned with personal relationships. For example, the OPUS study (
28) addressed housing and employment, and Essock and others (
33) used the indicator of living outside an institution as an estimate of social function. Overall, the LEO and OPUS studies suggested that although this finding cannot be generalized, ACT delivers superior social outcomes for first-episode patients.
This study examined whether over time patients who received ACT after a first episode of psychosis achieved a bigger social network and perceived greater social support than patients enrolled in standard care after a first or a second episode. It is based on a secondary analysis of data collected in the LEO trial, which compared outcomes among patients enrolled in a specialized early intervention that followed the ACT model or in standard care provided by a generic community mental health team (
25,
34). That study's main outcomes of interest were rates of hospitalization, symptoms, social functioning, and maintaining contact, but data about social networks were also collected. These data have not been previously reported.
Methods
Sample
The study participants were a subsample from the LEO randomized controlled trial (
25,
34). Participants were residents of the London borough of Lambeth who were between 16 and 40 years of age and who presented to mental health services with a first episode of nonaffective psychosis between January 2000 and October 2001. Patients were randomly assigned to a specialized care or standard care team by using sealed envelopes. Outcomes were assessed at six and 18 months.
Both treatment arms adhered to medication guidelines of good practice prescribed by the Maudsley Prescribing Guidelines (
35), and both had access to good practice guidelines for the wider psychosocial management of first-episode psychosis and had equal access to psychological advice and cognitive-behavioral therapy (CBT). The assignment process was approved by the St. Thomas' Hospital research ethics committee, and patients provided written consent to participate in research interviews after being told of randomization (
25,
34).
The LEO parent study had a sample of 144 patients, of whom 71 were assigned to specialized care and 73 to standard care. Over the 18-month follow up, patients who received care from the specialized team had fewer relapses and readmissions to a hospital and significantly better social and vocational functioning, satisfaction, and quality of life. Symptom improvement did not differ significantly between groups.
The study described here included 57 patients in specialized care and 50 patients in standard care for whom data on social support were available at six- and 18-month follow-ups.
Study design and measures
The main outcomes examined by this study were the structure of social support as measured by social network size, the functional adequacy of social support as measured by the gap between ideal and perceived levels of support, and the impact of social support on clinical outcomes at 18-month follow-up.
One week after being assigned at random to the specialized care or standard care model, participants were interviewed by trained research staff to collect sociodemographic data about age, gender, race-ethnicity, living arrangement, and relationship status. At six- and 18-month follow-ups, the short form of the Significant Others Scale (
36) was administered to both groups by a trained researcher. A self-report instrument, the SOS asks the respondent to identify specific people who provide practical and emotional support. The respondent rates each person on a 7-point Likert scale on four questions: Can you trust this person? Can you talk to this person frankly? Can you share your feelings with this person? Does this person give you practical help? Responses range from 1, never, to 7, always. The respondent is also asked to assign an ideal rating for each of the questions.
The SOS has been shown to have good six-month test-retest reliability (
36) and has been used to measure social support of individuals with schizophrenia (
13) and to distinguish between levels of support desired by nonpsychotic and psychotic patients (
37). Two variables of interest related to support were examined: the number of significant others reported, or network size, and the gap between actual and ideal ratings for the four questions.
At six-month and 18-month follow-ups, patients' clinical state was assessed with the Positive and Negative Syndrome Scale (PANSS) (
38), and social functioning was assessed by using the Global Assessment of Functioning (GAF) (
39).
It was hypothesized that patients assigned at random to the specialized service would have improved social functioning at 18 months in terms of the size of their social network and its functional adequacy. We also hypothesized that improvement in negative symptoms would be associated with having a larger network.
Statistical analysis
We first analyzed how well the subsample of 107 patients represented the entire sample of 144 in the parent study. Independent-sample t tests were used to compare means for continuous variables. Chi square tests were performed on categorical variables. When cell sizes were low, Fisher's exact test was used instead.
To test the main hypotheses, linear regression was used to predict PANSS, GAF, and perceived support scores on the SOS at 18-month follow-up, and network size was the predictor variable. To adjust for bias that was due to unequal attrition by treatment group, the regression model was weighted by the inverse probability of being observed at 18 months. Statistical significance was set at α=.05. SPSS, version 18, and Stata, version 10, were used for analysis.
Results
Sample characteristics by treatment condition
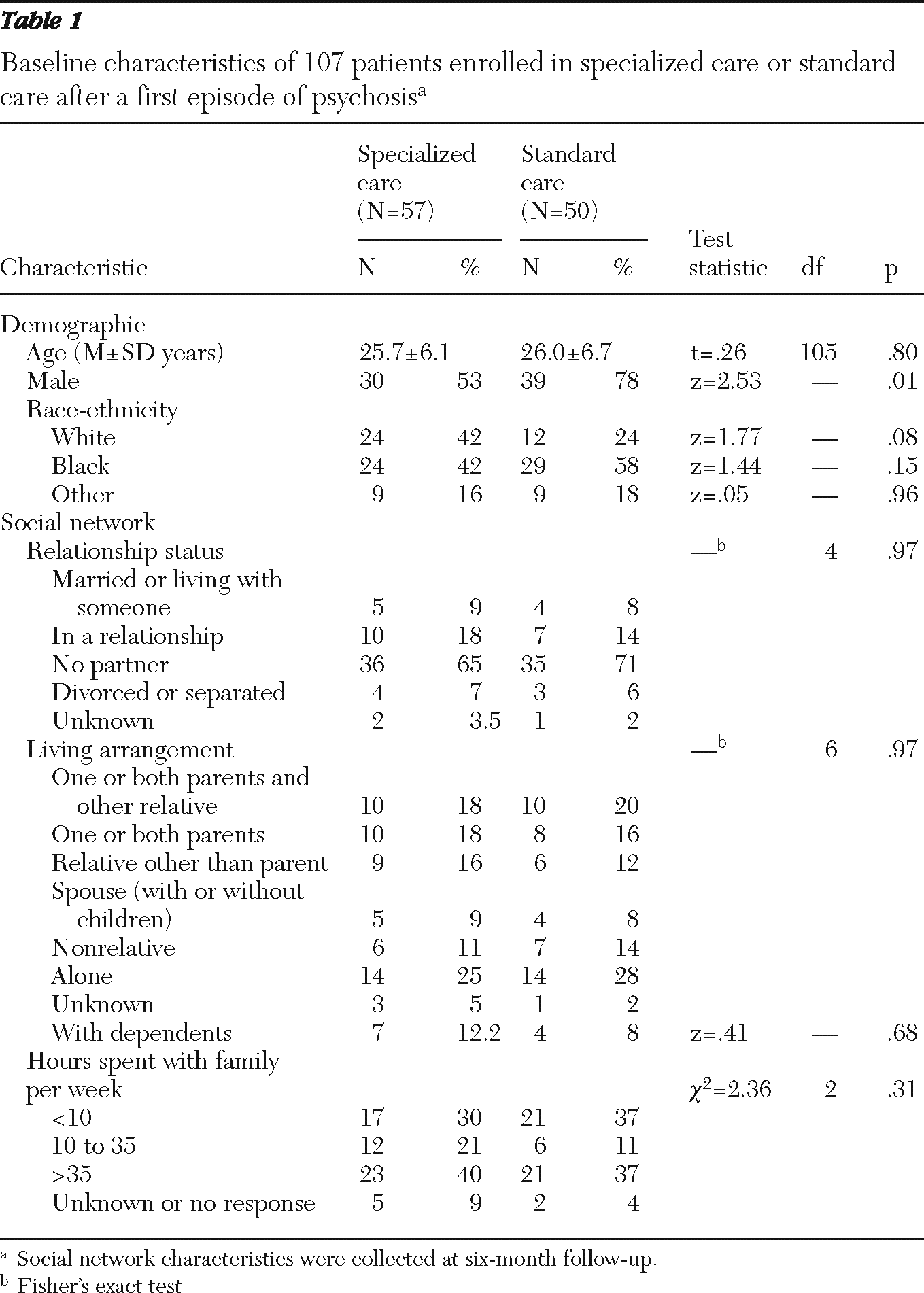
Table 1 shows the demographic characteristics at baseline and social network characteristics at six months for participants in the two treatment groups. Patients did not differ by age across groups, but there were slightly more males in the standard care group. A greater proportion of patients in specialized care were of a white racial-ethnic background, although the comparison did not reach significance. At least two-thirds of the patients in each group were not in committed relationships, and living alone was the most common living arrangement. The groups did not differ in the proportion of patients with dependents. In summary, except for gender, the specialized and standard care groups were comparable in demographic, relationship, and living characteristics.
Comparison of current sample with parent sample
The subsample and the parent sample were similar in age and in the proportion of participants who were male, but participants in the subsample were more likely to have recovered (χ2=6.19, df=1, p=.01).
Clinical and social measures at six months
Neither the total PANSS nor the GAF scores differed between treatment groups at six-month follow-up. The mean network size was not statistically different between groups, although there was a trend toward bigger networks among specialized care patients. When members of the patient's network were classified by role, for example, parent or sibling, participants in the specialized care group tended to report more responses for each role, suggesting that their networks were denser.
A comparison of emotional and practical support subscales of the SOS showed no difference between groups in ideal and perceived levels of support. For all subscales, the perceived level of support was less than the ideal level. Likewise the gap in ideal and perceived levels of emotional and social support did not differ statistically between groups. In summary, no significant differences were found in either clinical outcome or social support measures between the two treatment groups at six-month follow-up (data available upon request).
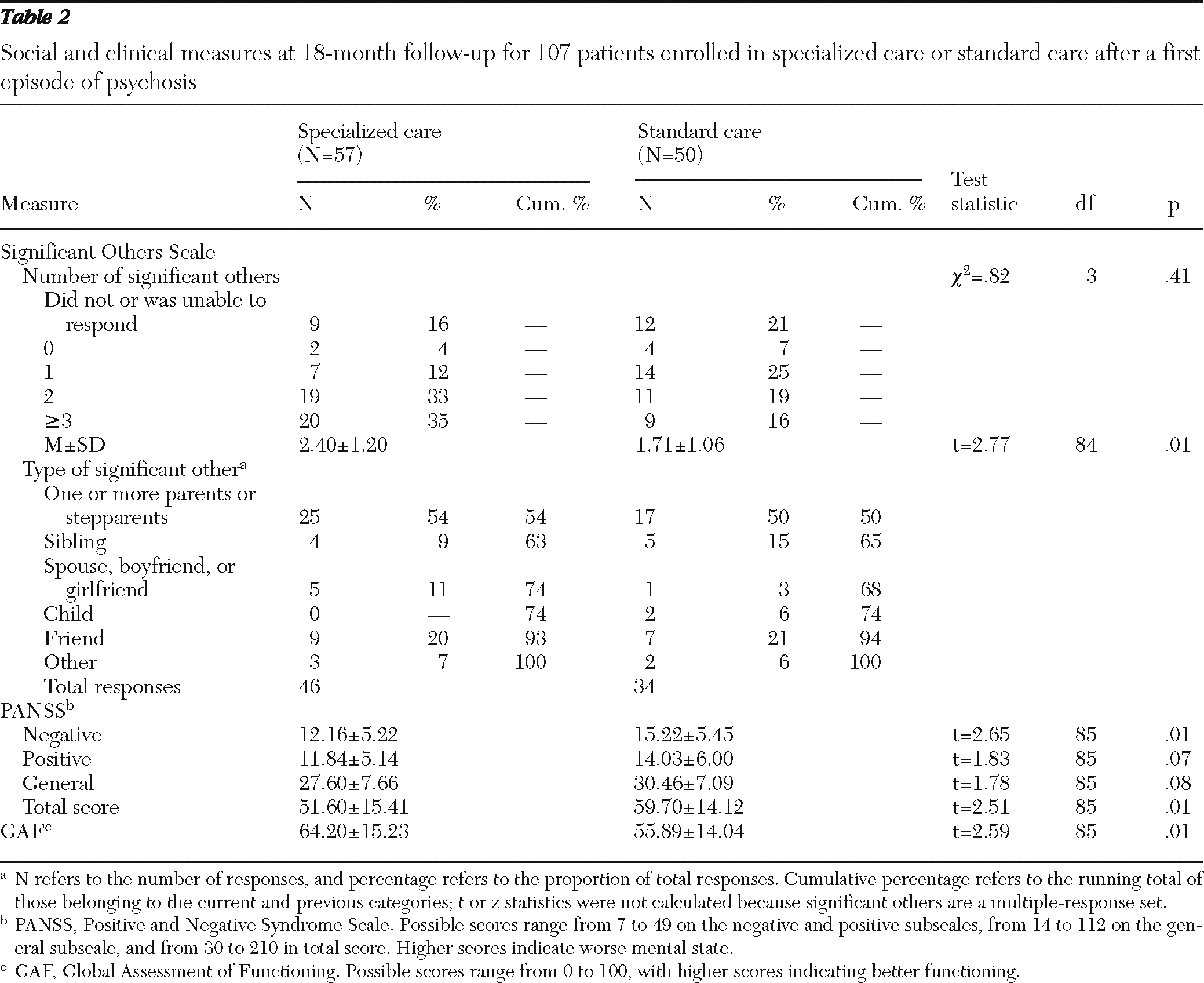
Clinical and social measures at 18 months
Table 2 compares social support and clinical outcomes between the groups after 18 months of follow-up. Participants in the specialized care group scored significantly better on the negative PANSS, total PANSS, and GAF, although we did not control for confounders that may have affected the analyses. In the parent study, symptomatic improvement did not vary between groups after adjustment for confounds (
25,
34).
At 18-month follow-up, the specialized care group had a larger network than the standard care group. Patients assigned to specialized care reported a mean±SD of 2.40±1.20 significant others versus 1.71±1.06 reported by patients in standard care (t=2.77, df=84, p=.01).
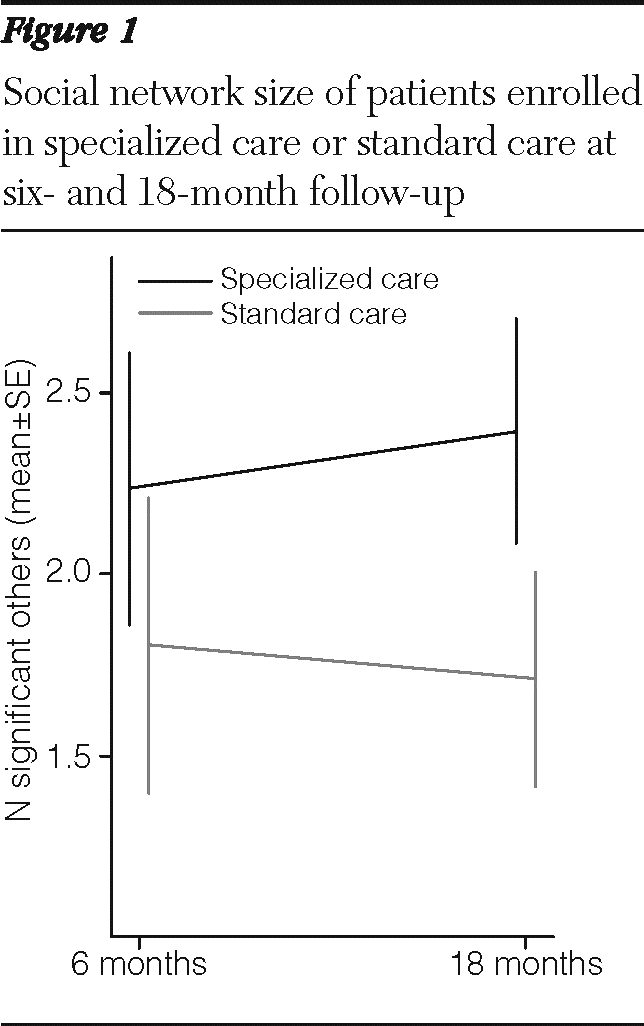
Figure 1 compares the groups' network size at six-month and 18-month follow-ups and shows that patients had only zero to three significant others.
By 18 months, the total number of kinds of relationships had decreased among both groups of participants since the six-month follow-up. This finding suggested that there was less variety in the kinds of relationships reported at 18 months than at six months. It was striking, for example, that 11 respondents reported living with dependents at baseline compared with only two at 18 months—a possible indicator of severed family ties or, alternatively, increased independence.
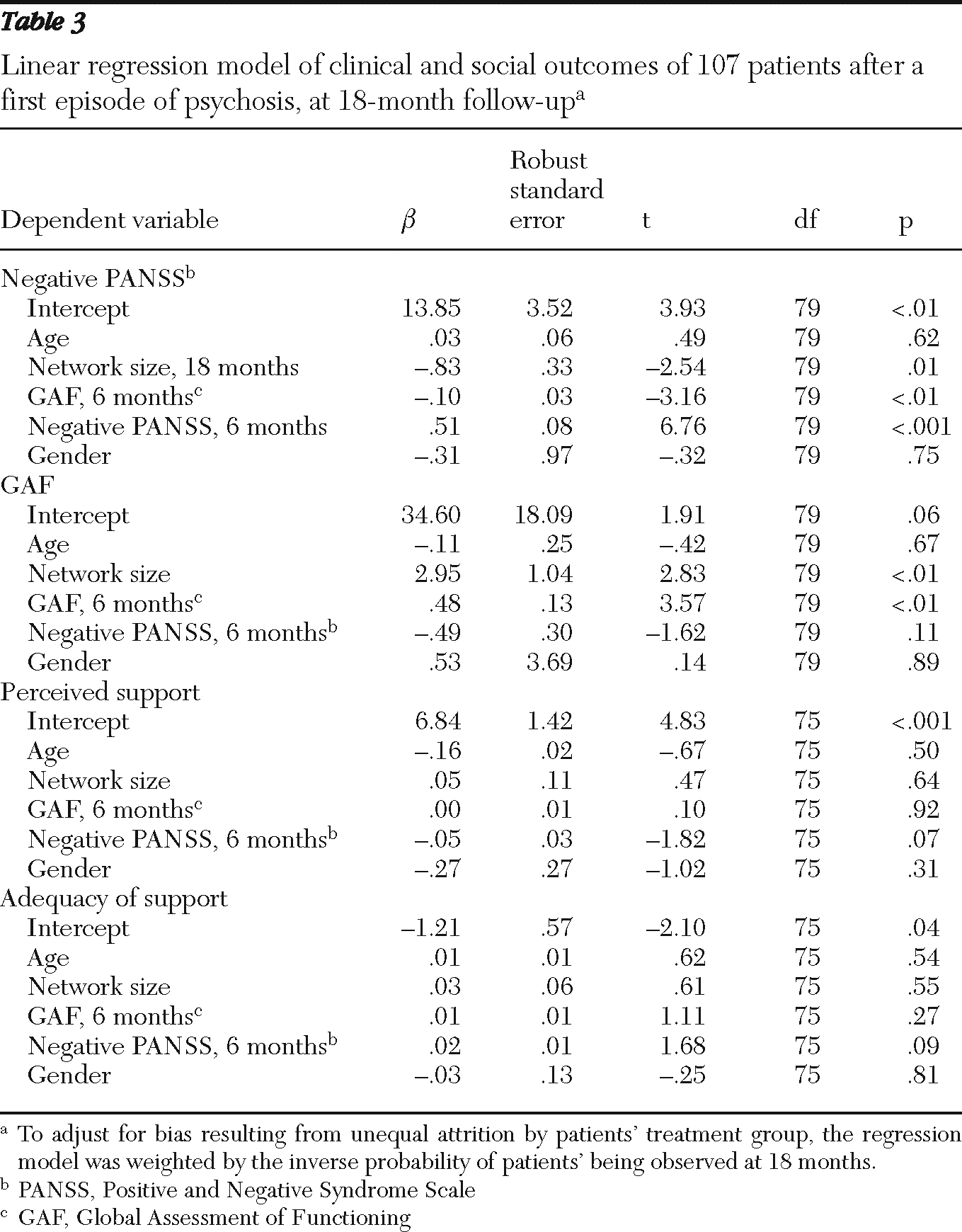
The linear regression model showed an inverse association between negative PANSS scores, the dependent variable, and network size after controlling for age, GAF and negative PANSS scores at six months, and demographic variables (
β=−.83, robust standard error [SE]=.33). Similarly, network size was associated with higher GAF scores (
β=2.95, SE=1.04) after control for the same confounders. Perceived support and the functional adequacy of support in relationships were both unrelated to network size and clinical and demographic variables (
Table 3).
Overall, the results suggested that the structural aspect of social support was associated with good prognosis at 18-month follow-up. However, we did not find a relationship between either the absolute level of support or the functional adequacy of relationships—in other words, the gap between ideal and actual levels of support—with prognosis.
Discussion
Higher social support for schizophrenia patients has been linked with superior clinical outcomes and social adjustment (
40,
41), but few studies have focused on the effect of ACT on relationships in early psychosis. The goal of this study was to assess the impact of an ACT program on social support by using data collected from the LEO study.
Results of clinical measures for the patients receiving specialized or standard care did not differ at the six-month follow-up, but results on the negative PANSS and GAF for the two groups were statistically different at the 18-month follow-up. The favorable clinical outcomes were associated with social network size at 18 months. Network size differed between the groups at 18 months but not at six months. Taken together, these findings suggest that ACT improved negative symptoms and social support for individuals with early psychoses.
Given that the two groups had similar relationship and living arrangement profiles at the start of the study, the difference in network size at 18-month follow-up could have resulted from the family counseling intervention and psychoeducation afforded by an ACT model of care. By giving families insight into a patient's condition, ACT can promote better acceptance and less hostility. Living with a family member with schizophrenia can be burdensome (
42). Without support from professionals, family members can experience significant strain and become more susceptible to illness (
43).
Within the ACT model, a care team can provide informal instruction to families on how to establish rapport with a family member with schizophrenia. In addition, the persistent high availability of support provided by a dedicated care team probably encouraged the young patients in this study to return to work or study and pick up fractured relationships. This interpretation is consistent with the parent study's finding that compared with standard care patients, a greater number of specialized care patients were able to maintain, initiate, or resume relationships at the 18-month follow-up (
25,
34).
Our results were consistent with a previous study that reported that network size was a protective factor against rehospitalization (
19). Another study reported that although having more family contact predicted better social functioning at 18 months, it was linked with worse prognosis (
44). We did not find evidence of an adverse effect of kin involvement. Instead our results suggested that the total number of people who were sources of emotional, practical, and social support was the single most important factor in determining clinical outcomes. Our results agreed with an earlier study that found that degree of social contacts—whether with family, friends, or professionals—was related to functional ability at one-year, two-year, and five-year follow-ups (
45).
We did not find a significant difference between groups in the functional aspect of the social networks. Both groups rated their perceived levels of support lower than ideal levels. This finding suggested that patients in the specialized care group, who had a larger network size, made up for the gap between ideal and perceived support by having more people to whom they could turn. Although the structural and functional aspects of a network are distinct, it is possible that quantity might compensate for the discrepancy in ideal and perceived levels of support.
Hammer and others (
14) observed that the network size of schizophrenia patients is small (four to five people), but another study of individuals with serious mental illness reported that more than two-thirds of the sample had ten or more social contacts (
46). Although the figures reported here are not directly comparable, the network size of our sample was likely smaller. The results of the SOS assessments suggested that the patients identified only from zero to three individuals as sources of emotional and practical help.
Our findings confirmed that patients with schizophrenia experience a “network crisis” (
9) According to Lipton and colleagues (
10), this crisis occurs after the first episode—at which time the individual needs to come to terms with stigmatization and exclusion. Perhaps mental health practitioners can take an active role in reestablishing the bonds between patients and their social networks. The results of this study contributed preliminary evidence that ACT might be well-suited to fill that role.
There were several limitations to this study. First, we were unable to measure social skills at any point in the study because the SOS does not capture this dimension or other outcomes, such as quality of life and respect from peers (
47). Thus it is possible that the patients assigned to specialized care had a greater ability to form and maintain relationships. Second, we did not collect feedback from parents, family members, or friends about the role of the mental health teams in managing the patient's illness. Such feedback would be helpful in planning the kind of support families need to restore or maintain relationships with the patient. Third, because this study represented a secondary analysis of a subsample, its conclusion is not supported as strongly as the conclusions of the parent study. By contrast, the major strength of the study reported here is the use of data collected from a randomized clinical trial in which the groups being compared were similar in profile at randomization.
Conclusions
A secondary analysis of data from the LEO study provided evidence that patients enrolled in ACT achieved superior clinical outcomes at 18 months and that this achievement was related to the social network size at the 18-month follow-up, the end point of the study. Although patients in standard care experienced the deterioration of network size that is typical of schizophrenia, early-episode patients enrolled in an ACT model had maintained their network size up to 18 months after entering treatment.
Acknowledgments and disclosures
The authors report no competing interests.