Measures of treatment integrity are crucial in determining adherence to a specific program model and differentiating a practice from others (
1–
4). Treatment integrity is equally important to clinical research and dissemination of evidence-based practices. Accurate dissemination requires specification of the critical components of a given model (
5), development of operational definitions of the critical ingredients (
6), and development of standardized assessments of the degree of implementation (
7). In addition to assisting with dissemination, adherence to program models has been shown to be a predictor of consumer outcomes (
7,
8). The identification of evidence-based practices, together with the need for broad and accurate dissemination of such practices, has led to a general call for the development of methods to empirically validate adherence to program models (
9–
13). However, treatment integrity is often neglected in both research and practice (
1,
14–
16).
The illness management and recovery (IMR) program is an evidence-based approach to teaching consumers with severe mental illness strategies for setting and achieving personal recovery goals and acquiring the knowledge and skills to manage their illnesses (
17,
18). IMR was developed as part of the National Implementing Evidence-Based Practices Project of the Substance Abuse and Mental Health Services Administration (
19) and includes an implementation toolkit with a workbook, practice demonstration videos, brochures, and consumer handouts (
20). IMR prescribes the use of complex clinical techniques to support consumers in learning the curriculum, setting and achieving goals, and managing their illness. Interventions include cognitive-behavioral techniques (
21,
22), motivation-based strategies (
23), and interactive educational techniques. IMR's effectiveness has been supported by longitudinal (
24,
25), multisite (
26–
28), and randomized controlled trials (
29–
31). Collectively, these studies have shown positive treatment outcomes, with increased illness self-management and coping skills and reduced hospitalization rates (
26).
IMR, as with all the programs in the National Implementing Evidence-Based Practices Project (
32), utilizes a program-level fidelity scale. The IMR Fidelity Scale (
33) is a 13-item scale to assess the degree of implementation of the entire program rather than of an individual practitioner. Each item is rated on a 5-point, behaviorally anchored scale. This scale has been used in state implementation projects (
26). The sensitivity of the scale has been demonstrated by increased scores after training and consultation (
32). This type of program-level scale adopts a broad view of how services are provided by focusing primarily on structural aspects of the program (for example, size of the intervention group) or clinician skills in the aggregate.
Although program-level fidelity is important, integrity is a multipart construct including adherence, competence, and differentiation (
16). Therapist competence—“level of skill shown by the therapist in delivering the treatment” (
34)—may be more appropriate for programs requiring specific, nuanced clinical interventions. For instance, practitioners must understand the program model and have the skills to implement it (
8,
35,
36). Moreover, treatment integrity measures that assess actual use of knowledge and skills are crucial and are an advancement over assessment techniques that rely on self-report or chart review. Various evidence-based psychotherapy models, such as cognitive-behavioral therapy for psychosis (
37,
38), multisystemic therapy (
39), and adolescent substance abuse treatment (
40), often assess treatment integrity at the clinical interaction level. Integrity at this level has been linked to positive outcomes for consumers (
41). With the exception of some measures focused on practitioners' general knowledge (
42–
45), evidence-based psychiatric rehabilitation programs lack clinician-level instruments, particularly those addressing competence. Therefore, the goal of the project described in this report was to create a clinician-level competency scale for IMR and test its psychometric properties.
Methods
Creation of the scale
Two groups of subject matter experts (group 1: ABM, LGS, and MPS; group 2: KTM and MS) each independently created clinician-level IMR competence scales based on the IMR Fidelity Scale (
33) and on two unpublished instruments used to evaluate provider competence: the Minnesota IMR Clinical Competence Scale and the IMR Knowledge Test. The scale creators included an IMR model creator, three researchers with extensive experience in IMR implementation, and an experienced IMR clinical supervisor. The scale was developed to rate either live or audio-recorded sessions. The draft scales from the two groups included 15 and 24 items, respectively. The content of these items overlapped; however, one group included an item on recovery orientation (retained in the final version) and items pertinent to specific IMR modules (eliminated from the final version). Items were compared and reconciled.
We initially set out to create behaviorally specific anchors using a 5-point scale, to be consistent with the IMR Fidelity Scale. For five items we were able to create anchors with good agreement between investigators. However, we had difficulty specifying anchors for 11 of the items, and we used a more generic set of anchors for those items that was based on the work of Blackburn and colleagues (
46). Higher scores correspond to greater competence in administering the target IMR element. After the initial version was created, investigators independently rated recordings of IMR sessions and then compared and discussed ratings, rationale for ratings, and any discrepancies. Investigators revised the scale, anchors, and rating criteria on the basis of these discussions. This process was repeated until no major rating discrepancies existed and investigators agreed that no further changes were necessary. This process took 14 iterations. The resulting IMR Treatment Integrity Scale (IT-IS) includes 13 required items and three optional items rated only when the particular skill is attempted. [The scale is available online as a data supplement to this article.]
Reliability testing
Sampling.
Group sessions were audiotaped as part of a randomized trial of IMR for adults with schizophrenia. Participants were randomly assigned to either weekly IMR or control groups. Participants included veterans at the local Department of Veterans Affairs (VA) medical center, as well as consumers at a local community mental health center, with groups held at the respective facilities. Inclusion criteria were a diagnosis of schizophrenia or schizoaffective disorder confirmed by the Structured Clinical Interview for DSM-IV (SCID) (
47), passing scores on a simple cognitive screen (
48), willingness to participate in a group intervention, and current enrollment in services at either participating facility. Participants were paid $20 for each completed interview, but they were not paid for group attendance.
Group facilitators.
IMR and control groups were facilitated initially by a licensed clinical social worker and later by a doctoral-level clinical psychologist (ABM), both of whom had previous experience providing and consulting on IMR. Groups were cofacilitated by clinical psychology graduate students (including LGS, AM, NR, CT, and LW) with a range of clinical experience.
Procedures.
IMR groups were conducted according to the group guidelines in the revised IMR implementation toolkit (
49). A typical group included brief socialization, discussion of items for the agenda, review of previously covered material, presentation of new material (guided by educational handouts from the IMR workbook and taught using motivation-based, educational, and cognitive-behavioral techniques), and goal setting and follow-up. The control group consisted of unstructured support, in which group members chose discussion topics and facilitators encouraged participation and maintained basic group ground rules (for example, mutual respect and confidentiality). Facilitators were instructed not to use educational materials or IMR-related teaching techniques, such as cognitive-behavioral techniques, but rather to use supportive therapeutic techniques (for example, active listening).
For rating we randomly selected 60 IMR sessions and 20 control group sessions (without replacement, separate draws for IMR and control). Raters were four clinical psychology graduate students (AM, NR, CT, and LW) with experience providing IMR. Raters were trained by the scale creators; scale creators did not serve as raters. Each rater scored 30 IMR tapes and ten control group tapes, and each session was rated by two raters (each rater overlapped with every other rater on an equal number of sessions). Both raters independently scored each session and then discussed any discrepancies and reached a consensus rating.
This study was conducted between May 2009 and May 2011 and was approved by the Indiana University-Purdue University Indianapolis Institutional Review Board.
Analyses.
First we examined interrater reliability for the total IT-IS and individual items by computing intraclass correlation coefficients (ICCs); sessions in which a rater was also a group cofacilitator (18 sessions, or 23%) were excluded from this analysis. Systematic rater bias was assessed by comparing mean ratings of total scores across raters by using analyses of variance. The remainder of the analyses were conducted with one of the two raters' scores, randomly selected (except when one rater was a group cofacilitator, in which case the other rater's scores were used).
The second set of analyses examined the factor structure and internal consistency of the scale. We considered two potential factor structures—a one-factor structure and a two-factor structure (general therapeutic elements and IMR-specific elements). We used confirmatory factor analyses to compare the relative fit of the two models (
50,
51) and selected the best model on the basis of goodness of fit and parsimony. Descriptive statistics were examined for range, distribution, and ceiling-floor effects for individual items. Internal consistency was examined through inspection of item-to-total correlations and Cronbach's alpha. Given the meaningful difference between adherence (using prescribed elements) and competence (skill in using the elements), item analyses were repeated with just the IMR sessions (excluding the control sessions) to test the relationship between skill at specific IMR components within sessions.
We also evaluated whether IMR competence was independent of when and where the session took place. To examine this, we correlated group date and IT-IS score and conducted an independent-samples t test comparing IT-IS scores by site. Finally, construct validity was examined through comparison of known groups. We hypothesized that IMR sessions would receive higher scores than control group sessions on the total scale and on the specific IMR subscales. We tested this hypothesis by using independent-samples t tests and excluding sessions in which a rater was also the group leader (given leaders' a priori knowledge of the group condition).
Results
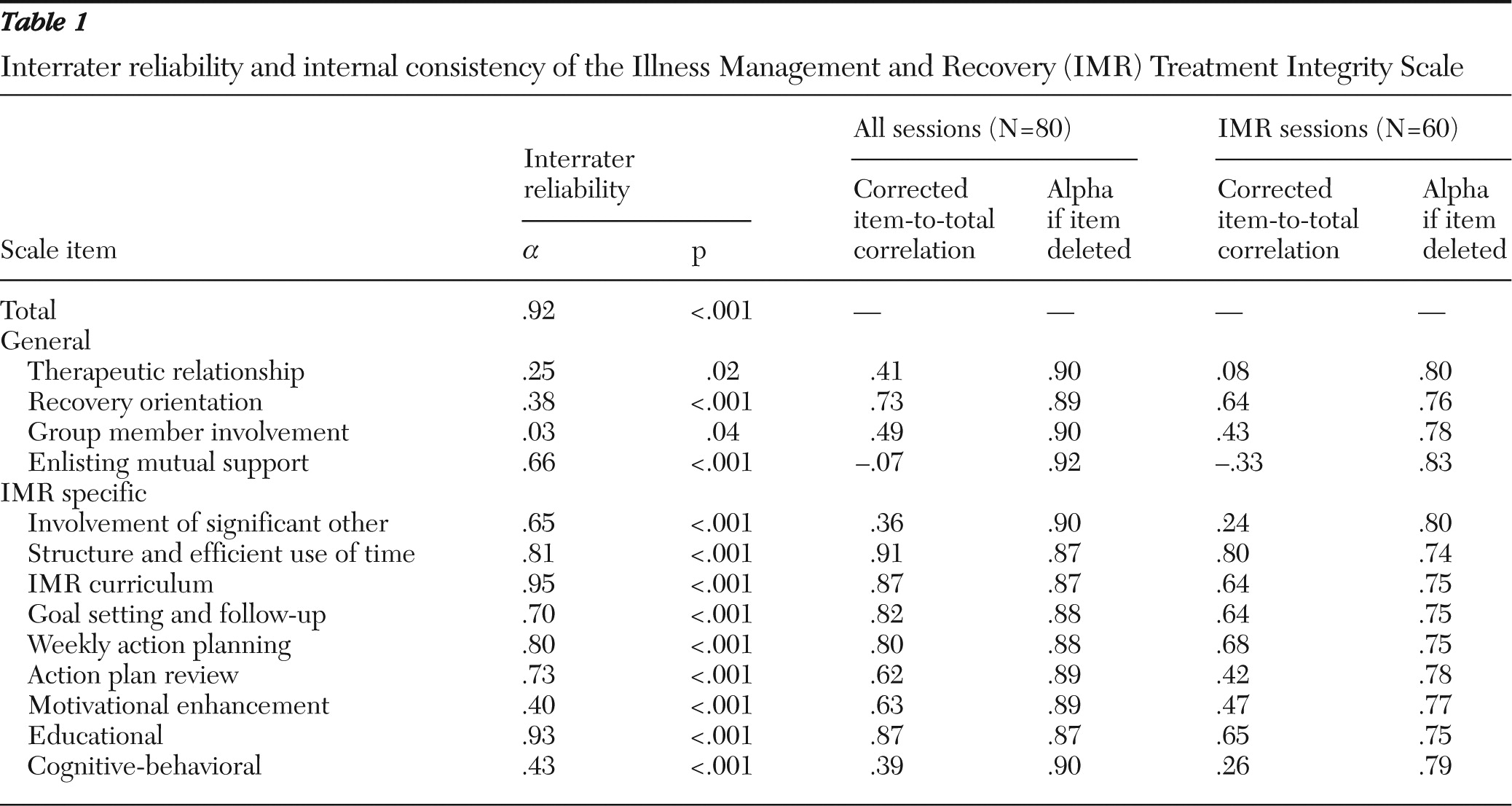
As shown in
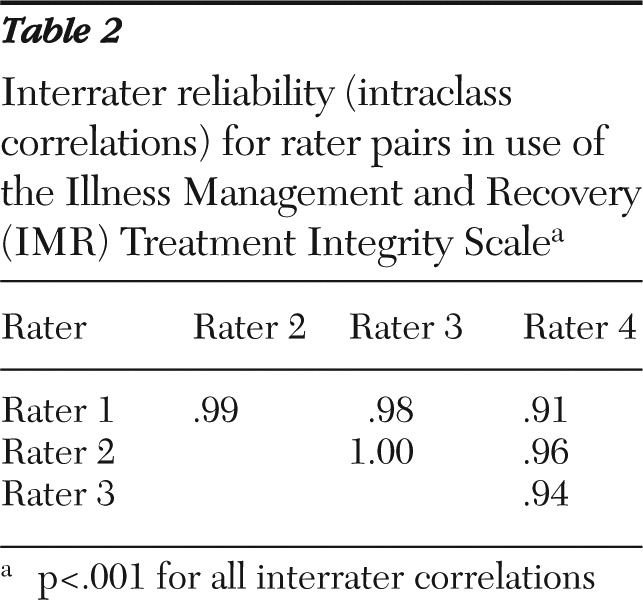
Table 1, interrater reliability for the total scale score was excellent (ICC=.92, p<.001). Reliability for individual items was variable, with ICCs ranging from .03 (group member involvement) to .95 (IMR curriculum). Interrater reliability tended to be worse for general therapeutic items and items using the generic anchors. Interrater reliability did not vary substantially by rater pair (
Table 2). Mean scores did not differ by rater: rater 1, 3.33±.82; rater 2, 3.38 ±.92; rater 3, 3.27±.77; rater 4, 3.41±.75). The remaining analyses were conducted with one of the two raters' scores.
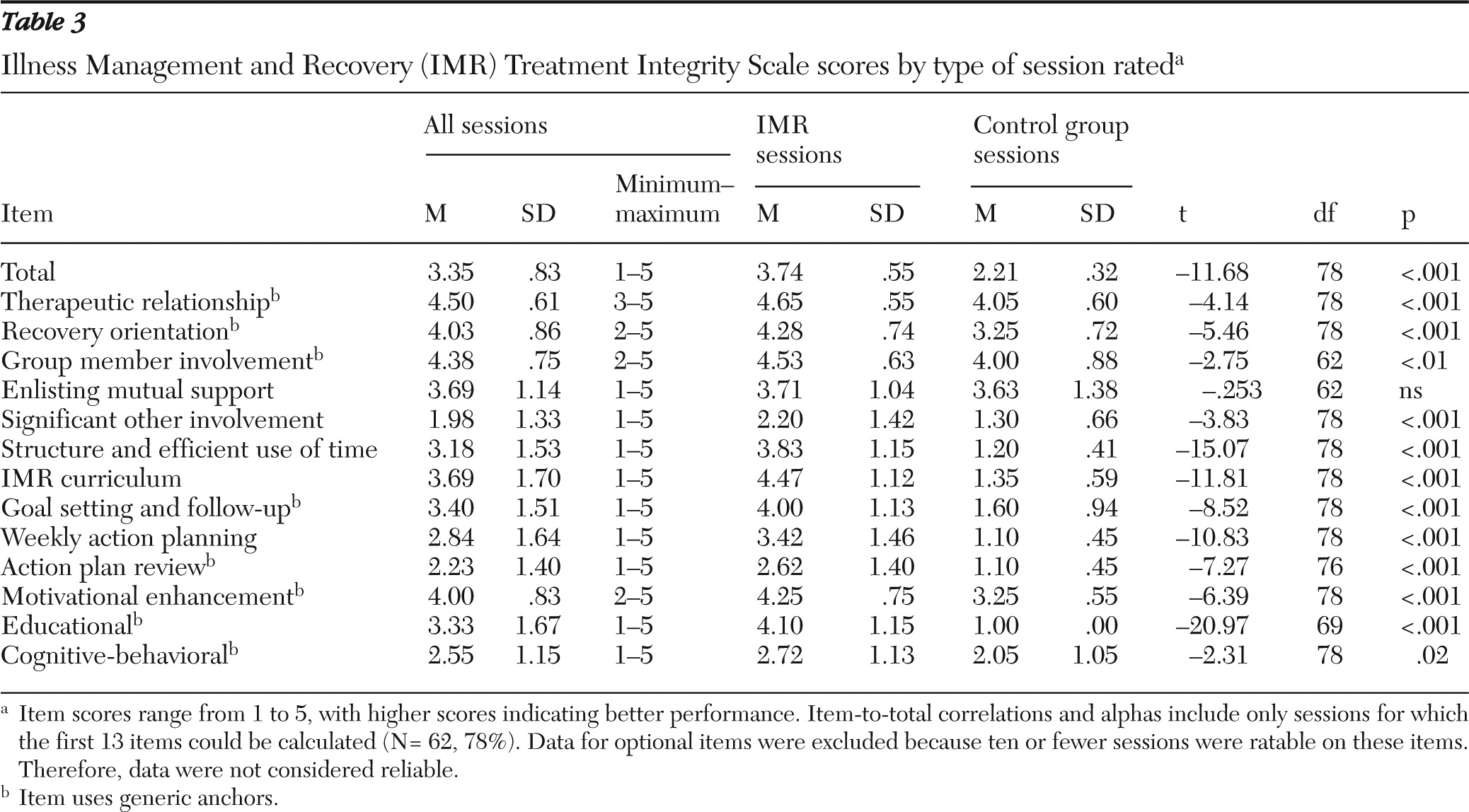
Total and item means, standard deviations, and ranges are presented in
Table 3. In regard to the confirmatory factor analysis, goodness-of-fit indicators were compared between the one-factor and two-factor models. Values were as follows for the one-factor model:
χ2=167.78, df=64; standardized root mean square residual (RMSR)=.08; adjusted goodness-of-fit index (GFI)=.71; root mean square error of approximation (RMSEA)=.13; and Bentler comparative fit index=.88. For the two-factor model, these values were as follows:
χ2=244.03, df=63; standardized RMSR=.26; adjusted GFI=.67; RMSEA=.17; and Bentler comparative fit index=.78. Overall, results indicate that the one-factor model fit is a good fit and better than the two-factor model.
Regarding internal consistency, the items specific to group processes (group member involvement and enlisting mutual support) were not calculated for 18 sessions (23%) because those sessions were attended by only one participant. Therefore, alphas and item-to-total correlations were calculated for the 62 sessions for which all items could be calculated. Overall internal consistency was high both including and excluding the group items (Cronbach's
α=.90 and .91, respectively). As shown in
Table 1, item-to-total correlations ranged from very poor (enlisting mutual support, r=−.07) to very strong (structure and efficient use of time, r=.91). Alphas did not increase more than .02 with the removal of any item. When only the IMR session tapes were used, the overall internal consistency was weaker but still in the acceptable range (
α=.79). Individual items varied in item-to-total correlations; enlisting mutual support was negatively related to the total score.
As hypothesized, total IT-IS scores were significantly higher for IMR sessions than for control group sessions (
Table 3), supporting the construct validity of the scale. Means for items were higher for IMR sessions than for control sessions, with the exception of enlisting mutual support. The scores for the VA sessions (N=44, mean score=3.35±.86) did not differ from those for the sessions conducted at the community site (N=36, mean score=3.36±.81). The mean IT-IS score was also not related to date of the group session.
Discussion
This study provided promising preliminary results on the reliability and validity of the IT-IS, a newly developed measure of IMR clinician competence. The total scale had excellent interrater reliability and adequate item-level interrater reliability, despite some notable exceptions. The scale was internally consistent and best fit a one-factor model. As hypothesized, scores on the IT-IS did not systematically differ by treatment site, rater, or date of the session.
Two items are candidates for removal from the IT-IS. The item about enlisting mutual support did not distinguish IMR sessions from control group sessions and was negatively related to overall competence within IMR sessions. Conversely, therapeutic relationship did differ between the IMR and control groups, although it theoretically should not. Interrater reliability was also poor for this item, and it was only weakly related to the total score in the total sample. There was also a ceiling effect (mean=4.5) in the sample, which could account for the low reliability and minimal relationship to total score. Therapeutic alliance is an important common factor in psychotherapy and has been found to moderate the link between treatment integrity and treatment outcomes in other research (
52,
53). It is possible that wider variability of this item would be found if a larger number of group leaders were sampled. The scoring criteria for this item could also be revised to make it less lenient. Another alternative would be to supplement the IT-IS with other validated measures of common therapeutic factors (for example, the Working Alliance Inventory [
54]).
The construct validity of the scale was supported: IMR sessions were rated higher than control group sessions on the total IT-IS and on all but one IT-IS item. Structure and efficient use of time was most strongly related to total score and may be most indicative of an IMR session compared with an unstructured intervention group. However, this relationship may be less predictive of IMR when compared with other structured interventions, such as cognitive-behavioral therapy or cognitive-processing therapy. Future work is needed to examine how the scale performs when IMR is compared with other structured interventions. Within the IMR sample, action planning was most strongly associated with the total score and therefore may be most indicative of quality within IMR. In our clinical experience with IMR, assisting consumers to convert abstract recovery goals into tangible steps may be emblematic of IMR.
Implications
The IT-IS has several potential important uses. Clinically, the IT-IS can serve as a valuable training tool by specifying the critical elements of IMR and the behaviors associated with competent practice. In addition, the IT-IS can be used by supervisors as a tool to provide specific feedback and develop performance improvement goals (
55). From a programmatic standpoint, the IT-IS provides an indicator of variability between clinicians and could be used to assess and plan for additional training needs (
56).
In research applications, previous studies have used the IMR Fidelity Scale to monitor overall program fidelity. However, there may be significant variability in the quality of IMR implementation between practitioners within the same program. By monitoring competence at the level of clinical interactions, researchers can obtain a more fine-grained evaluation of the IMR process. An important next step will be examining the relationship between competence (IT-IS items), IMR mechanism of action, and outcomes.
Monitoring with both the IMR Fidelity Scale and the IT-IS would ensure faithful implementation and provide accountability for funding, regulatory bodies, and other stakeholders. The IT-IS complements and extends the IMR Fidelity Scale by assessing individual clinicians. However, there are some structural elements on the IMR Fidelity Scale that are not captured by the IT-IS (for example, group size, session length, and comprehensive curriculum) that would still be important to assess at the program level. We view the two scales as complementary, rather than competing, tools.
Limitations
This study had several limitations. The study used a fairly homogeneous sample of sessions, and the group sessions were cofacilitated by creators of the IT-IS or IT-IS raters (although only sessions rated by two raters who were not cofacilitators in the session were included in interrater reliability analyses). Although session recordings were blinded to the treatment condition and date of the recording, the raters' knowledge of the study and other treatment providers made true blinding impossible. Future studies should use raters who play no role in the intervention. In a related issue, the highly structured and technically specific nature of IMR makes it highly distinguishable from an unstructured control group. Future studies should use the IT-IS to compare IMR to other structured, but distinct, interventions, such as cognitive-behavioral therapy or social skills training, to provide a more rigorous test of known-groups validity. The IT-IS should also be evaluated in individual IMR sessions to ensure applicability across modalities. Finally, the IT-IS included three optional items that are rated only when the specific element is used. In the study sample, application of these elements was not sufficient to permit analysis of these items. Future studies should intentionally sample for sessions in which these elements could be rated.
Conclusions
The IT-IS is a promising measure of the competence of IMR practitioners. A revised version of the scale could be valuable in a variety of contexts, including clinical, supervisory, administrative, and research. Future studies are needed to replicate this study with independent raters and to extend the research to nongroup IMR.
Acknowledgments and disclosures
This work was supported in part by Health Services Research and Development grant IAC 05-254-3 from the U.S. Department of Veterans Affairs. Dr. McGuire's work as an investigator with the Implementation Research Institute, George Warren Brown School of Social Work, Washington University in St. Louis, is supported through an award from the National Institute of Mental Health (R25 MH080916-01A2) and by the Quality Enhancement Research Initiative, Health Services Research and Development Service, U.S. Department of Veterans Affairs.
The authors report no competing interests.