Researchers have documented excess and early mortality among patients with mental illness, yet most studies were restricted to patient populations in psychiatric settings (
1). Depression is a leading cause of morbidity worldwide (
2) and is associated with mortality among older adults (
3). However, whether depression is associated with premature mortality, and to specific causes of premature death, in the general adult population remains an unanswered question.
Although users of U.S. Department of Veterans Affairs (VA) services are typically older, the VA is the largest health care provider for the 1.6 million younger veterans who have served in Operation Enduring Freedom (OEF), in Afghanistan, and Operation Iraqi Freedom (OIF) (
4). In 2008, 17.4% of OEF/OIF VA patients were diagnosed as having depression, which was six times higher than in 2002; a majority of depressed veterans had comorbid diagnoses (
4). Thirty-five percent of veterans who returned from deployment in 2003–2004 and used VA services during the following year accessed mental health services (
5). Today many more veterans than in previous eras are utilizing VA health care, possibly because of policies that have broadened access to returning veterans. Therefore, although it is important to understand overall causes of mortality among VA patients, it could be particularly useful to understand causes of premature mortality as well.
The goal of this study was to extend prior research on depression and mortality among veterans and to examine specific causes and timing of mortality in this population. We examined the years of potential life lost (YPLL) associated with 13 causes of death as well as all-cause mortality among VA patients with or without depression. We addressed two related questions. First, do the ages at death and YPLL differ among VA patients with or without depression? Second, do the ages at death and YPLL among VA patients with or without depression differ by cause of death?
Methods
We assessed risks of mortality for all causes and for specific diseases and the mean age of death and YPLL among VA patients with or without a depression diagnosis. This study used national data from the VA Serious Mental Illness Treatment Resource and Evaluation Center (SMITREC) administrative data resources linked with National Death Index (NDI) data from the Centers for Disease Control and Prevention (CDC). SMITREC's administrative data resources include extracts from the Veterans Health Administration National Patient Care Database and incorporate data for all veterans who used inpatient or outpatient health services at the VA (
6). Specifically, these data include VA patient treatment files (PTF), bed census files, extended care files, and outpatient care files (OPC). The PTF and OPC data sets include demographic, diagnostic, and services utilization data. The NDI is considered the “gold standard” of U.S. mortality databases (
7) and was established for medical research.
Patients treated in the VA health system during fiscal year (FY) 2006 and who were alive at the beginning of FY 2007 were included in the study. We examined one-year mortality from the beginning to the end of FY 2007 for VA patients with or without depression during FY 2006. Patients with at least one inpatient or outpatient depression diagnosis (ICD-9 codes 293.83, 296.2, 296.3, 296.90, 296.99, 298.0, 300.4, 301.12, 309.0, 309.1, and 311) were included.
To calculate YPLL, we divided the study cohort into age groups, as follows: 18–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and 85 and older. Second, by using CDC life tables for 2007, we identified remaining life expectancy for the midpoint of each age group (
8). Finally, we calculated YPLL as age group midpoint + life expectancy − age of death. This method evaluates the impact of early mortality on an entire population, not just on those who died younger than a specified age (such as 65 or 75, which is commonly used in epidemiologic literature to represent premature death) (
9). This method assumes that risk of death in future years is approximated by the age-specific rates of death from all causes during the past year. Previous research found that the proportion of YPLL attributable to individual causes more closely resembles cause-specific mortality when derived from the remaining-life-expectancy method than by YPLL before age 65 (
9). Therefore, we calculated YPLL with the remaining-life-expectancy method as well as mean age of death for all VA patients with or without depression.
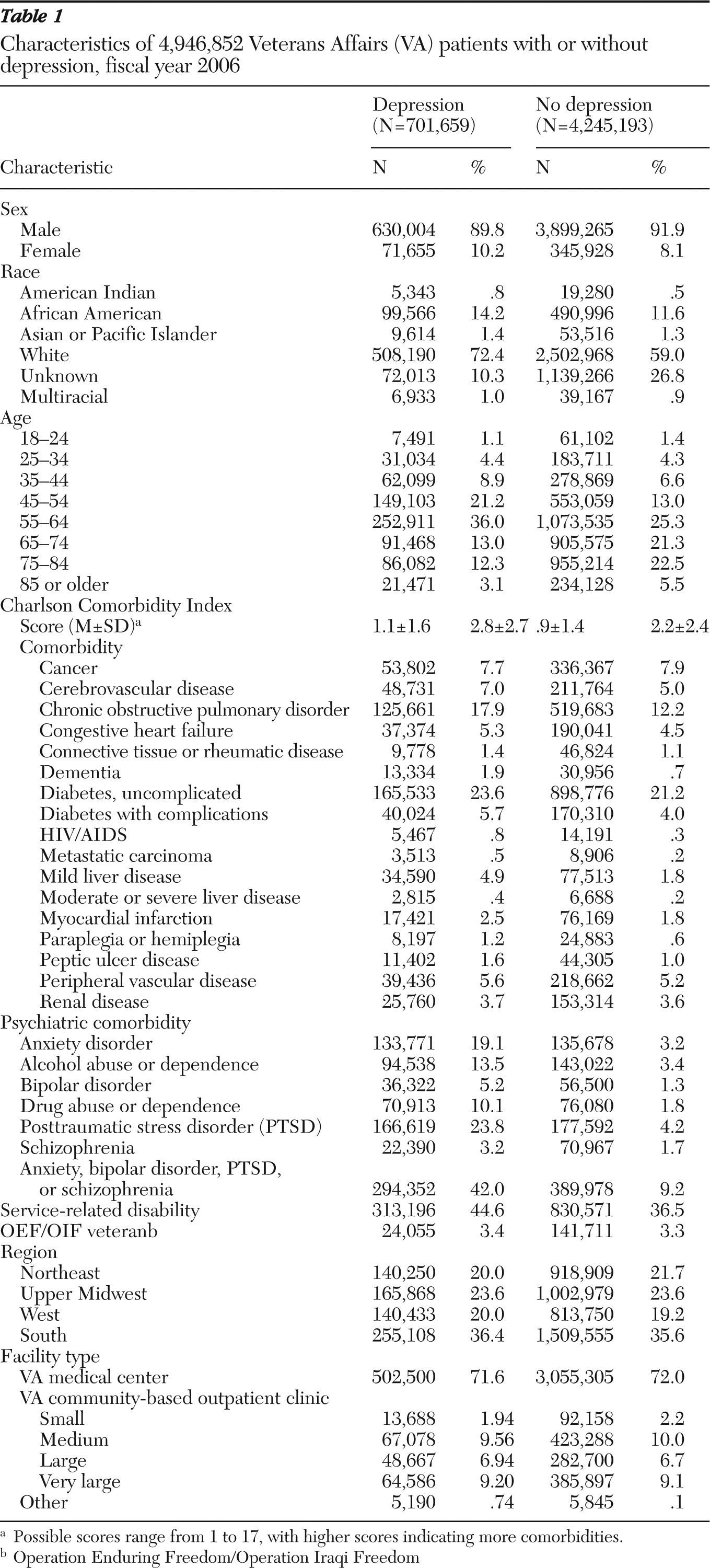
We compared these two groups overall and by sex, race, age, comorbidity, and, given the unique nature of the VA patient population, connection with VA services (service-related disability) and service in OEF/OIF. Second, we identified mean age of death and YPLL by cause of death.
Finally, we conducted sensitivity analyses to examine how comorbid psychiatric conditions (anxiety disorder, bipolar disorder, posttraumatic stress disorder, schizophrenia, or any of these four disorders) influenced the relationships between depression status and YPLL and age of death.
Results
A total of 4,946,852 patients met study criteria, and 14.2% (N=701,659) had a depression diagnosis during FY 2006. In FY 2007, a total of 167,069 (3.4%) patients died.
Table 1 shows the characteristics of the study population. Leading causes of death for all patients included heart disease (N=45,110, 27%), malignant neoplasms (N=44,179, 27%), respiratory disease (N=11,713, 7%), cerebrovascular disease (N=7,197, 4%), accidents (N=5,730, 3%), diabetes (N=5,598, 3%), nephritis (N=3,671, 2%), septicemia (N=2,389, 1%) influenza (N=3,400, 2%), suicide (N=1,684, 1%), liver disease (N=2,106, 1%), and homicide (N=318, <1%). These causes of death represented 81% of all deaths among the entire patient population.
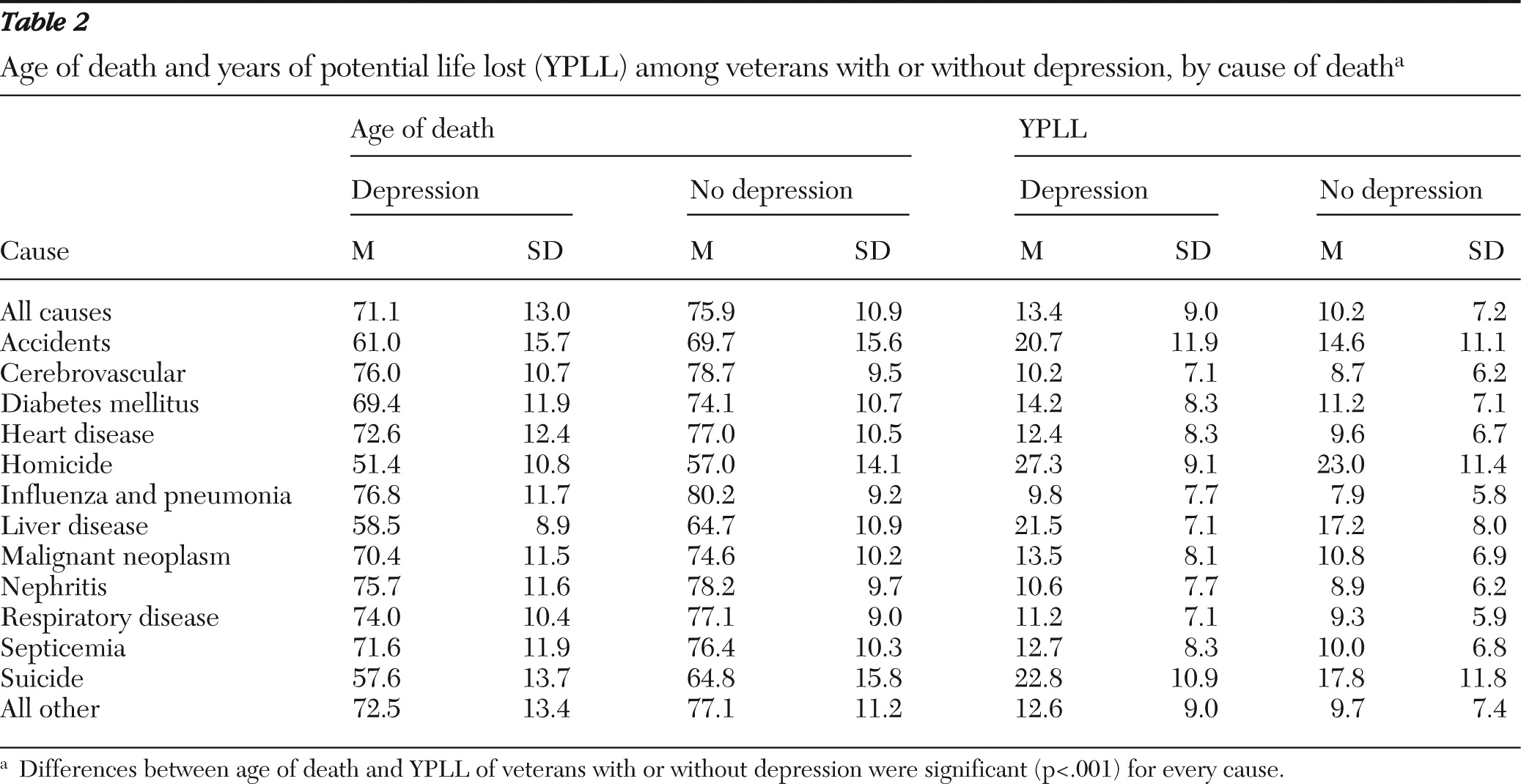
Table 2 illustrates age of death and YPLL for VA patients with or without depression. The mean±SD age of death was 71.1±13.0 and 75.9±10.9, respectively, for patients with or without depression. Death from all causes was associated with YPLL of 13.4±9.0 and 10.2±7.2, respectively, for patients with or without depression. Depression was associated with significantly earlier ages of death and more YPLL for all causes of death examined. Most deaths from unnatural causes (homicide, suicide, and accidents) occurred at earlier ages than deaths from natural causes; however, liver disease was also associated with earlier mortality. Unnatural deaths also accounted for the greatest differentials in YPLL and age of death between patients with or without depression.
Results from sensitivity analyses (data not shown) indicated that individuals with depression and any additional comorbid psychiatric disorder (anxiety disorder, bipolar disorder, posttraumatic stress disorder, or schizophrenia) had more YPLL and an earlier age of death than those without any psychiatric disorder. Further, those with any of the other disorders besides depression had more YPLL and died at an earlier age than patients with depression but not any of the other disorders. Finally, among people with no other comorbid psychiatric condition, people with depression died earlier and had more YPLL than those without depression.
Discussion
This work extended limited previous research (
10) on causes of death among depressed and nondepressed patients of an entire health system. We found that not only did depressed VA patients die younger and have more YPLL from unnatural causes than nondepressed VA patients, but they died younger and had more YPLL from natural causes. This information can be important for health system planning because although it may be important to focus on efforts to reduce unnatural death such as suicide, it is also valuable to recognize that depression is associated with earlier mortality from other diseases.
Depression may be a marker for early onset of a general medical condition that is related to premature mortality. For example, there is evidence that major depressive disorder is a risk factor for the development of heart disease, and increased plasma cortisol levels among patients with major depressive disorder have been documented (
11). There is much greater general medical comorbidity among depressed patients, but the direction of causality remains uncertain. If depression causes increased mortality, enhanced interventions are needed to treat depression among patients with depressive disorders. Alternatively, if depression serves as a marker of greater severity of other medical conditions, primary care clinicians may need to consider providing better monitoring of treatment of all medical conditions among depressed patients. Finally, if the problem is poor treatment compliance by depressed patients, treatment providers should assess adherence among depressed patients to treatment of all medical conditions, including depression.
Unfortunately, we cannot determine from our administrative data sources which of these theories explains our findings. Additional research is needed to examine how comorbid medical and psychiatric diseases, health behaviors, medication use, and other treatments interact to influence the relationship between depression and mortality.
Although this study provided unique information about a health system, there were limitations. This study focused on veterans treated by the VA health system, who are sicker than other veterans and the non-VA population and are mostly male. The sample comprised primarily veterans of earlier conflicts, including Vietnam and Korea, and the relationship between depression and mortality may differ depending on the era of military service.
The leading causes of death in the VA population were similar to those of the general U.S. population (
12). Furthermore, clients of several state public mental health systems also had higher YPLL and died earlier than the general population in those states (
13). Thus in examining mortality among VA patients, YPLL may be an appropriate metric, given that comparisons of rankings of causes of premature death have been made by treatment systems other than the VA health system, including other government-funded systems. Although previous research has examined the impact of insurance type (private, public, or none) on health outcomes, we do not know whether comparable studies outside the VA would have observed types of risks of early mortality and age of death that were similar to our findings (
14). Finally, it is important to note that because life expectancy is not uniform across age groups or even among individuals born in a given year, use of YPLL provides an estimate, not an exact assessment, of premature mortality.
Another potential limitation was the use of clinical diagnoses of depression. It is likely that we missed depression cases not detected during clinic visits. Furthermore, we were unable to determine the length of time that individuals experienced depression. Some patients may have experienced an acute or new episode during FY 2006, the baseline-assessment year, and others may have had a history of chronic depression. Our findings could be a conservative estimate of the impact of depression on mortality, or conversely, by detecting more severe cases of depression, we may have falsely inflated the association between depression and mortality.
Finally, adjusted models were beyond the scope of this brief report. It is possible that our findings may be explained or attenuated by an examination of service, sociodemographic, clinical, and treatment factors that may contribute to differences in mortality outcomes between depressed and nondepressed VA patients. Such models may provide important information for developing and targeting interventions.
Conclusions
VA patients with depression died on average five years earlier than VA patients without depression, and excess YPLL were observed for all causes of mortality. These findings highlight the importance of depression as a potential contributor to early mortality. Because depression is treatable, these findings raise the possibility that depression treatment could have a measurable impact on risk of early death. Furthermore, the results suggest that health system efforts to decrease excess mortality among depressed patients might need to focus on increasing quality of care and overall medical management for depression rather than target any specific medical morbidity that adversely affects longevity.
Acknowledgments and disclosures
This study was funded by grants IIR 10-176-3, CD2 07-206-1, and CDA 10-036-1 from the U.S. Department of Veterans Affairs Health Services Research and Development Service.
The authors report no competing interests.