Measurement-based care is defined as the use of standardized quantitative measurement of patient symptoms to guide clinical decision making (
1). Measurement-based care has been found to improve patient outcomes when introduced into clinical practice (
2). Recent work has suggested various strategies for implementing measurement-based care (
1,
3,
4). This evidence-based practice has been used successfully in mental health care (
4–
8); however, studies demonstrate that its implementation is not widespread (
8). Previous work suggests that mental health care providers have been resistant to use a standardized symptom measurement tool, resulting in wide variation in clinical practices (
9). As evidence-based treatment guidelines have been developed and adopted in mental health settings, some have attempted to implement measurement-based care in routine practice (
10). However, the implementation of measurement-based care has not been easy; many providers are still resistant to changing their practice patterns (
9).
The objective of this study was to determine mental health providers' perceived value of patients' self-reported mental health symptom measurement and measurement-based care. Furthermore, we sought to explore how exposure to mental health symptom measures would affect providers' perceived value of the measure.
Methods
This project was carried out at the White River Junction Veterans Affairs (WRJ VA) medical center, which is a 60-bed hospital (including medical, surgical, intensive care, and mental health care units) that also offers a myriad of outpatient services (primary care, surgery, medical subspecialties, pharmacy, occupational and rehabilitation services, social services, vision and hearing services, and so on). It is one of eight VA medical centers (and 42 associated community-based outpatient centers) in the Veterans Integrated Service Network located in New England.
In 2004, the WRJ VA reconfigured its patient evaluation process as part of a quality improvement effort to improve access to mental health care (
11). The newly designed clinic was based on several models of integrated mental health and primary care. Many of those models advocate the use of a robust system for measurement of patient symptoms, and in 2005 the WRJ VA implemented the facilitated use of measurement-based care in the integrated primary care-mental health clinic. Standardized measures were collected from patients with the use of a tablet computer just prior to seeing the provider at each visit. The assessment included the Beck Depression Inventory (
12), the PTSD Checklist (
13), the Spielberger State-Trait Anxiety Inventory (
14), and the Medical Outcomes Study 36-item Short Form (mental and physical component summaries) (
15). On completion of the symptom assessment, a standardized symptom report, described in other work (
11), was printed and made available to the provider for review before or during the clinic visit. The results of the assessment were entered into the electronic medical record by the provider as part of the notes template.
As part of this project, providers were surveyed about their opinions of the measurement process and instruments used in the integrated mental health and primary care clinic. All providers (including psychiatrists, psychologists, therapists, nursing staff, and other professional staff) involved in the integrated clinic were surveyed. The survey inquired about the usefulness of patient data provided prior to the implementation of measurement-based care and again six months after the implementation had occurred. This project was approved by the Dartmouth institutional review board, and participants gave informed consent.
Results
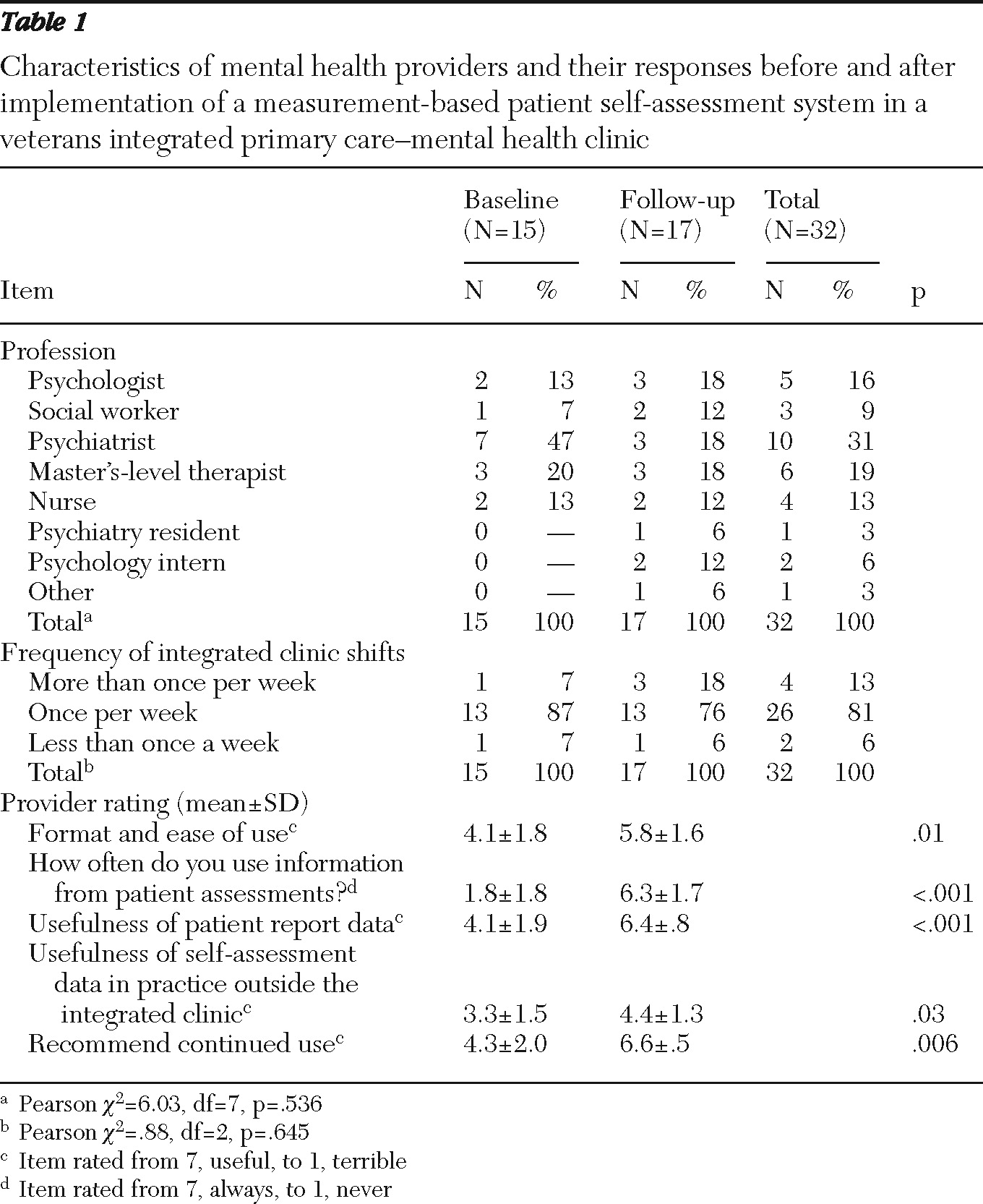
The type of providers responding to the baseline (N=15, 75% response rate) and follow-up (N=17, 85% response rate) surveys did not differ significantly by type of profession. Similarly, the frequency at which the providers were scheduled at the clinic did not differ between baseline and follow-up (
Table 1). Using a 7-point scale response scale (1, terrible or never, to 7, useful or always), providers answered a series of questions about the presentation and usefulness of patients' self-assessment information, including, How would you rate the format or ease of use and understanding of the surveys? How often do you use information from patients' assessments? How useful do you find the patient report data? How often do you use patient report data in your VA practice outside the integrated clinic? How would you rate the usefulness you get from the surveys? and Would you recommend the integrated clinic continue to use patient surveys?
At baseline, respondents rarely used the information presented in the patient assessments (mean±SD=1.8±1.8), and they reported the format (4.1±1.8) and usefulness of the patient report data (4.1±1.9) to be marginal. Similarly, they would only slightly recommend the use of patient surveys at baseline (4.3±2.0). At follow-up, respondents almost always used the information presented in the patient assessments (6.3±1.7), they reported that they found the format (5.8±1.6) and content (6.4±.8) of the patient report data to be very useful, and they highly recommended continued use of patient surveys in the integrated clinic (6.6±.5). As shown in
Table 1, comparisons between all baseline and follow-up questions yielded significant differences (p<.05). Of note is that neither the measures nor format of the report was modified between baseline and follow-up. In addition, no provider training on how to interpret the measures or implementation assistance was used.
Discussion
This work provides important clues to successful implementation of measurement-based care in mental health. Providers who had not been exposed to measurement-based care perceived it to be unhelpful, whereas the same providers found it highly valuable after brief exposure to it. Despite the enthusiasm for measurement-based care in the study clinic, there was only a small increase in the percentage of providers who reported that they used the measurement tools in their VA practice outside the project setting (from 20% to 23%). This suggests that developing a system of care that routinely collects patient data and reports it to providers in a timely, easy-to-interpret format may be the most important factor in implementing measurement-based care. A supportive environment that will assist with the logistics of the assessment and reporting (including patients' use of a touch pad and the printing of the reports and placement in the patient file) appears to be imperative to successful implementation. Furthermore, this work suggests that providers' lack of enthusiasm about integration of routine collection and reporting of patient symptoms may be a less important factor in implementing measurement-based care. Our findings indicated that this barrier was overcome by simply exposing providers to a measurement-based system.
This study was not without limitations. It was conducted at a small, rural VA medical center involving a limited number of staff, and the findings may not be generalizable to other integrated primary care-mental health clinics.
Conclusions
This study showed that mental health providers who had not been exposed to validated, standardized patient self-report instruments about symptoms asserted they would not find the information useful and reported a low rate of use in practice. However, after a brief exposure to the standardized assessment tool in this clinical setting, the same providers reported the information to be very useful and recommended that it be continued.
Acknowledgments and disclosures
The authors acknowledge Patricia Stender for conducting data entry.
The authors report no competing interests.