Posttraumatic stress disorder (PTSD) is a widespread problem among veterans and is often chronic and debilitating. Although the exact prevalence is impossible to determine, PTSD is estimated to affect hundreds of thousands of veterans in the United States and the numbers affected will likely keep growing (
1,
2). One recent report showed that between 2002 and 2008, nearly 50,000 new cases of PTSD were diagnosed among returning soldiers (
3).
Although symptomology is varied, PTSD is associated with impairment in social functioning, sleep, anxiety, and anger and recently has been increasingly linked with cases of suicide by veterans (
4–
8). Studies show that veterans with PTSD have high rates of physical symptomology and mortality (
9,
10). Because of the widespread and serious nature of PTSD, the U.S. Department of Veterans Affairs (VA) designated it as one of the “signature injuries” caused by recent conflicts (
11,
12).
Because of the growing number of PTSD cases, additional services are needed to successfully manage veterans. Yet little is known about factors affecting veterans' use of VA-based outpatient care—the most common avenue for treatment (
13). This gap in knowledge is a critical oversight that impedes efforts to plan for additional services.
The behavioral model of health service utilization by Andersen and Newman (
14) and Anderson and Bartkus (
15) has been widely used to understand help-seeking behavior. According to the model, use of a service is influenced by predisposing, enabling, and need factors. Predisposing variables refer to patient characteristics that exist independent of the illness, such as gender, age, marital status, and other individual demographic characteristics. Enabling variables refer to the means by which individuals can access care, such as proximity of the service and number of services available. Need variables refer to the severity of an individual's illness.
Data examining predisposing among veterans show mixed results, largely depending on the subpopulation of veterans and the type of services studied. For example, research found that men and women use inpatient VA-based care at equal rates but that women used less general outpatient care and more outpatient-based mental health services than men (
16,
17). Patterns of care among veterans of different marital status and race are more variable and are not well understood. In particular, studies have shown higher levels of mental health utilization among unmarried versus married individuals among the general populace (
18), yet this result has not been replicated consistently among veterans (
19–
21). Studies of the relationship of race and service use have yielded mixed results in both VA and non-VA samples (
22–
26).
Increasingly, research to understand how utilization is associated with service era is emerging. Soldiers returning from Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) are beginning to show different diagnosis and help-seeking patterns than veterans of prior eras (
16,
27). Enabling and need variables appear to have a more consistent impact than predisposing factors on use of services by veterans of different service eras. The VA is unique in that health care coverage is partly determined by the extent to which the disability is connected to service history (service connection) and, to a lesser extent, income. Accordingly, service connection and income are often correlated with service use (
28,
29). Proximity to care, comorbidity, and condition severity typically also show consistent associations with service use in veteran populations (
19,
22,
30–
32).
We conducted a retrospective chart review to understand personal characteristics that affected veterans' use of VA-based outpatient health care for PTSD. We focused our examination on characteristics derived from the Veterans Health Administration (VHA) Medical SAS Datasets, which have been used to examine patient outcomes and service use during the past two decades (
33–
35). Research on the VA databases has shown them to be a valuable resource for health services exploration (
36).
Our objectives were to describe veterans' utilization of outpatient services for PTSD and determine factors associated with patients' use of services. Understanding how veterans access services for PTSD is important in order to assess whether care is adequately and uniformly distributed and used; this is especially important as rates of PTSD among veterans treated by the VA increase (
2).
Methods
Data set and model variables
The VHA Medical SAS Outpatient Datasets consist of medical information for all veterans who presented at the VA from October 1, 2007, through September 30, 2008. We initially extracted data about 415,617 patients who presented for outpatient care and were assigned the ICD-9 code for PTSD (309.81).
Using the behavioral model of Andersen and Newman (
14) and Anderson and Bartkus (
15) as a framework, we used as model variables personal characteristics in each of the three dimensions—predisposing, enabling, and need. We included the following variables in our regression model: place of residence (urban, rural, and highly rural), gender, marital status (married or unmarried), race (Caucasian, African American, American Indian, Asian, and Native Hawaiian), combat veteran status, service era (OEF/OIF or prior conflicts), comorbidity, income, and service connection (percentage of disability connected to service history).
Because the patient database does not contain a service era category for OEF/OIF, we used a method formulated by other researchers to create a dichotomous variable that was based on birthday; veterans born after 1973 were coded as OEF/OIF (
2). Comorbidity was measured by a dichotomous indicator of the presence or absence of any comorbidity; it was derived from a numeric field in the patient record indicating the number of
ICD-9 diagnoses.
We categorized patients from an urban, rural, or highly rural area by using the Zip Code Crosswalk, developed by West and colleagues (
37), to match patients' residential zip codes to a rural designation. After merging patient records with the crosswalk, we found 869 patient zip codes—less than 1% of the data, mostly from U.S. territories—that did not match a zip code in the crosswalk. These patients were dropped from the file, yielding a final total of 414,748 unique veterans. We examined the data for missing information about the model covariates. Race values were missing for about 16% of veterans, and these patients (N=64,778) were not included in the regression analysis. Difficulties with the VA's collection of data about race have been previously discussed, and the problem of missing data was not unexpected (
38). Data were not missing for any of the covariates.
The dependent variable for the regression analysis was the total number of patient visits annually. This number was the sum of visits by each patient recorded in the initial visit-level file and represented service use throughout the investigation. To examine outpatient care visits that occurred at specialized PTSD clinics, we merged identifying information from the
2009 Specialized PTSD Programs Directory (
39). Information in this directory allowed us to identify 109 specialized PTSD clinics by matching the station identification number.
Analysis
We used negative binomial regression to examine the main effects and two-way interactions of the nine covariates on veterans' outpatient utilization of PTSD care. Negative binomial regression has been recommended for use with the VA patient databases, in particular, because the number of annual visits has considerable variability among patients (
40). SPSS 17 was used for all analyses. Because of the large number of cases, we defined statistical significance as p≤.001. Incidence rate ratios (IRRs) were also used to help interpret the data.
Study approval
The Colorado Institutional Review Board and the Denver VA Research and Design Committee approved the study. Because the examination was performed on secondary, deidentified data, a waiver of informed patient consent was obtained.
Results
Main effects
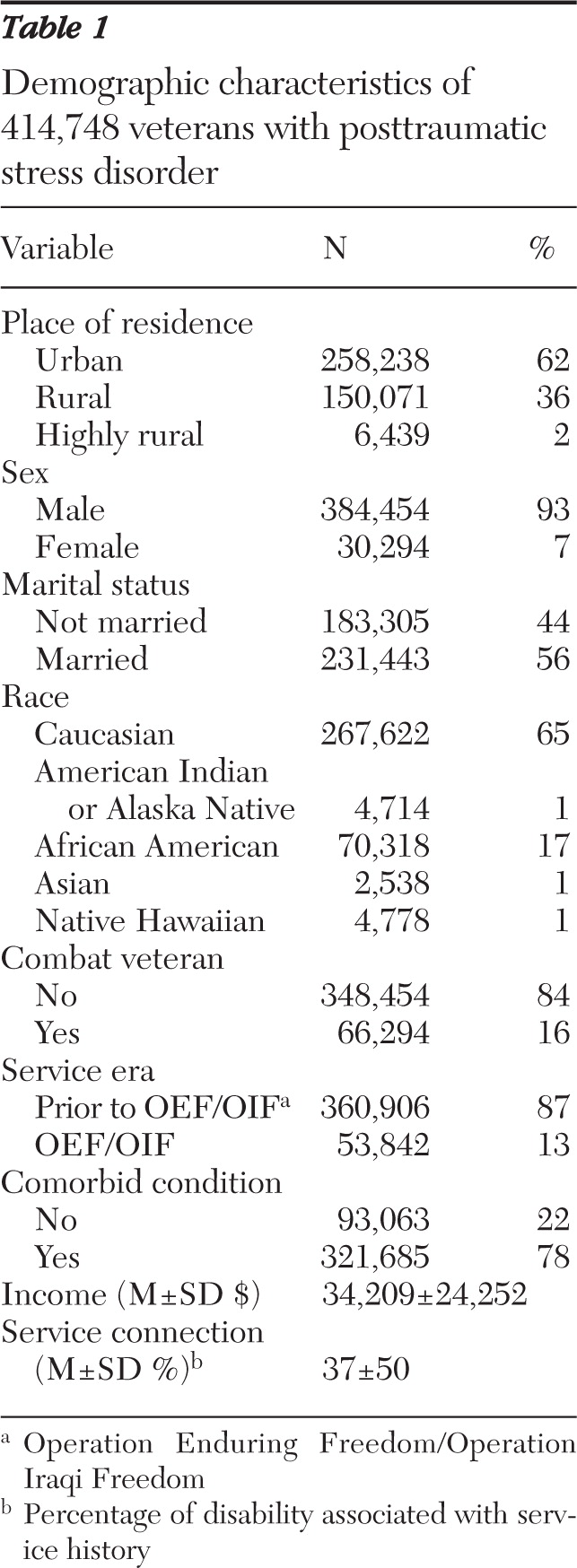
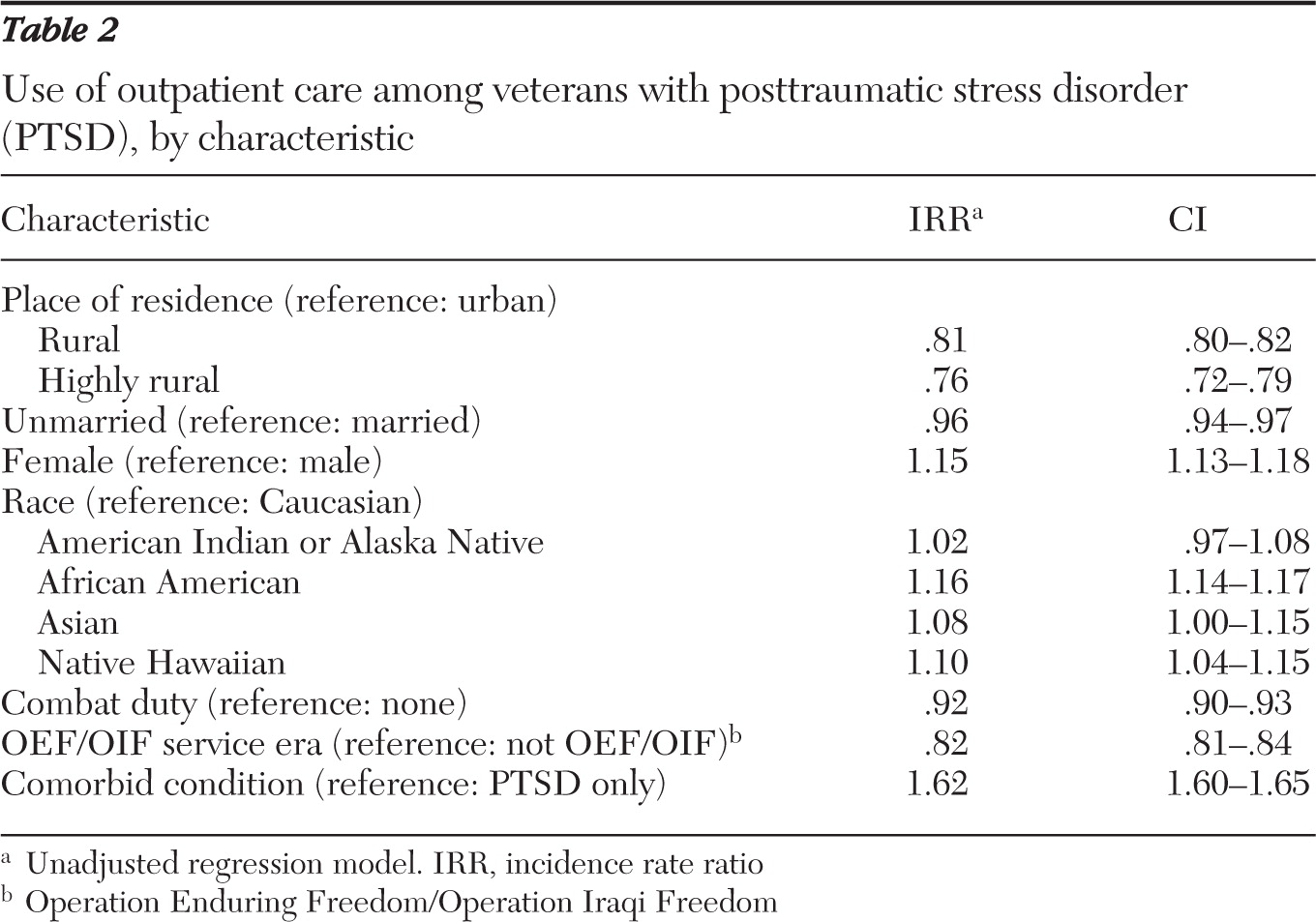
Table 1 shows the demographic characteristics of the sample. The first component of our analysis looked at the main effects of each covariate on veterans' use of all VA-based outpatient care (
Table 2). Three variables—place of residence, service era, and comorbidity—had the most influence on veterans' help-seeking behavior. Specifically, both rural and highly rural patients had fewer visits than urban patients, veterans serving in OEF/OIF utilized fewer services than those who served in prior service eras, and veterans with comorbid conditions utilized more services than veterans with only PTSD.
Adjusted model
Because of the large number of patients, several alphas in the unadjusted model yielded a significance value of ≤.001 but had very little impact on service use. Therefore, to create the adjusted model, we used only the three variables that most affected service utilization—place of residence, service era, and comorbidity.
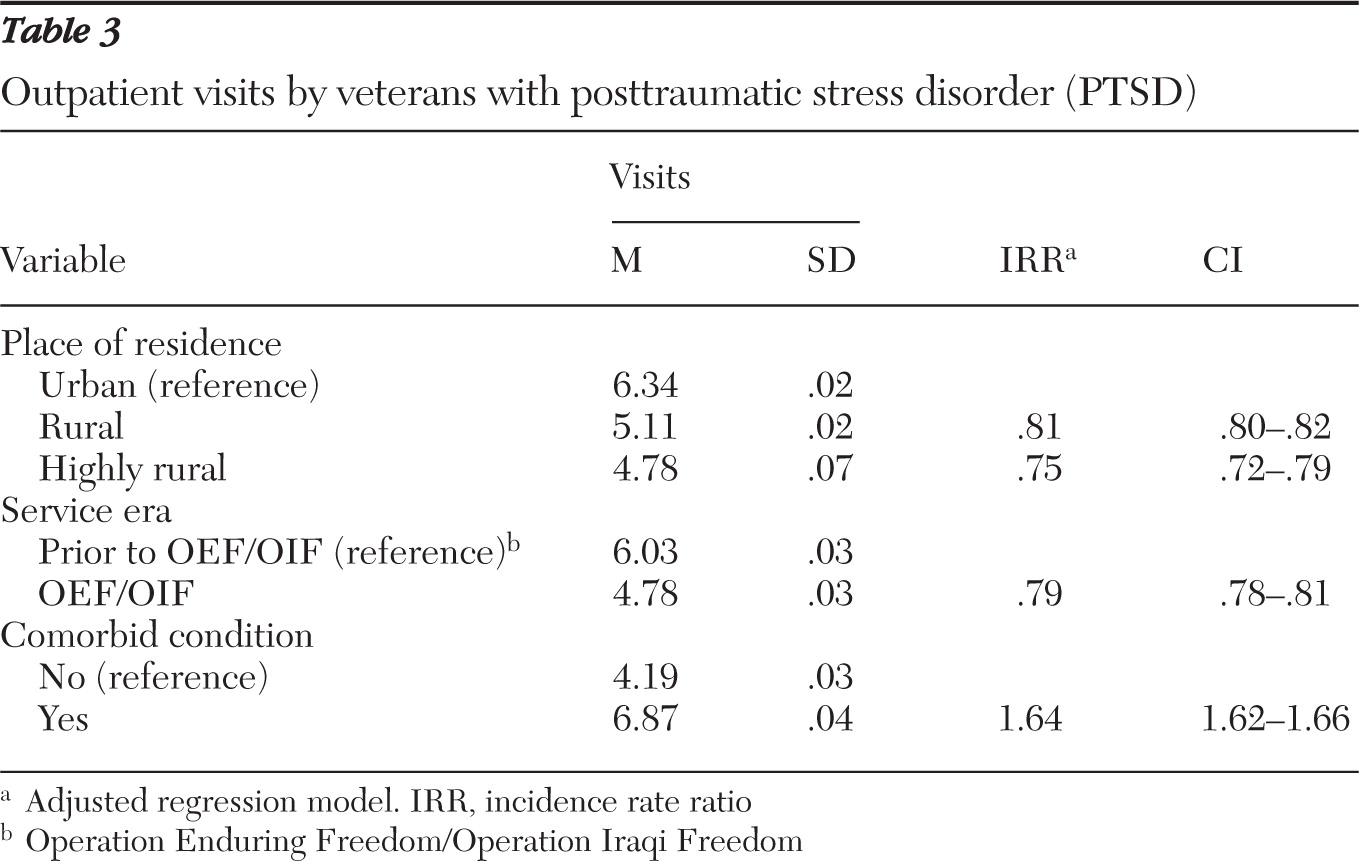
Veterans from rural areas had 19% fewer visits (mean=5.11; IRR=.81, 95% confidence interval [CI]=.80–.82) and veterans from highly rural areas had 25% fewer visits (mean=4.78; IRR=.75, CI=.72–.79) than urban veterans (mean=6.34) (
Table 3). OEF/OIF veterans had about 21% fewer visits than veterans who served in prior eras (mean=4.78 and 6.03, respectively; IRR=.79, CI=.78–.81). Veterans with comorbid conditions had 64% more visits than those with only PTSD (mean=6.87 and 4.19, respectively; IRR=1.64, CI=1.62–1.66).
Effect modifiers
The third component of our analysis examined potential two-way interactions between residence and each category of covariate. This procedure allowed us to better understand the association of geography and service use. The results of this analysis yielded interesting utilization patterns by service era and place of residence (data not shown). Specifically, by using negative binomial regression, we found that service era was linked to help-seeking behavior among urban-dwelling veterans but not among rural-dwelling veterans. Specifically, urban-dwelling veterans who served prior to OEF/OIF had an average of 8.34 annual visits, whereas urban-dwelling OEF/OIF veterans had an average of 6.49 annual visits (IRR=.79, CI=.77–.79). On the other hand, rates of service use among rural veterans were similar regardless of patients' service era. As with our prior regression analysis, we examined both statistical significance and clinical significance in this analysis.
Specialized PTSD services
The fourth component of our analysis compared visits to PTSD specialty clinics by veterans from urban, rural, or highly rural areas while controlling for total number of visits. Again, we found that veterans in rural and highly rural locations had less service use than veterans in urban areas. Specifically, veterans from rural areas had 22% fewer visits (mean=2.17; IRR=.88, CI=.87–.89) and veterans from highly rural veterans had 33% fewer visits (mean=1.66; IRR=.67, CI=.64–.71) than urban veterans (mean=2.46).
Post hoc examination of service era
As a result of our analysis, we wanted to understand the association between period of service and other demographic characteristics in our database. We conducted several post hoc tests by using chi square (Cramér's V) and analysis of variance (eta squared) statistical tests to examine the effect size for each comparison. We found that a higher percentage of OEF/OIF veterans lived in urban versus rural areas (37% and 30%, respectively, χ2=1,025.13, df=2, p<.001), although this effect size was small (V=.05). The mean rating for service connection was lower among veterans of OEF/OIF than among veterans of prior service eras (23% versus 53%; F=15,596.96, df=1 and 414,746, p<.001), but, again, the effect size was small (R2=.04). Approximately 78% of OEF/OIF and non-OEF-OIF veterans were diagnosed with more than one health condition.
Discussion
The VA, like most health organizations, locates primary care facilities in more populous areas to serve the largest numbers of patients. The unequal distribution of facilities has an impact on care-seeking behavior. Past research shows that rates of utilization of VA-based care are among the highest for veterans with PTSD compared with veterans with other disorders (
41). Yet this investigation showed that service use was highly contingent on veterans' proximity to care. It is clear that veterans in rural areas had less access to outpatient care in general and to specialty PTSD services in particular. We worry, therefore, that veterans living outside metropolitan communities receive less optimal care of PTSD symptomology. Recent treatment guidelines issued jointly by the VA and the U.S. Department of Defense recommend a variety of tools to help veterans cope with PTSD but do not specify how many annual visits are required for sufficient care (
42). On the basis of that omission, it is unclear whether making 19% to 25% fewer visits might hinder treatment of veterans from rural areas.
From the systems perspective, increasing veterans' use of services might have profound consequences on the need for additional service options. In one year alone, over 156,000 veterans in rural and highly rural areas presented to the VA for PTSD care. Using the mean number of visits from our adjusted model, we found that an additional 194,000 visits would have occurred had veterans of rural and highly rural areas and urban-dwelling veterans sought care at equal rates. Projecting out five years, that's nearly a million visits. Research suggests that currently many veterans do not utilize VA services because of the long wait required for appointments (
23). If veterans in rural areas utilize additional care for PTSD, the VA will need to respond with more treatment opportunities.
One way to supplement service options in rural areas is through the use of alternative delivery mechanisms. Increasingly, rural areas turn to telemental health as a bridge when access to health care is of concern. As of 2006, the VA offered telemental health services at 290 sites, over half of which were community-based outpatient clinics (
43). Research demonstrates that telemental health is useful for addressing the problems associated with a lack of services in rural areas (
31); therefore, the VA should consider adding telemental health services. A special effort to establish telehealth, particularly specialized PTSD clinics, at existing facilities should also be considered.
The results of this study revealed that other factors besides geography influenced care-seeking behavior for PTSD. Urban-dwelling veterans who served during the current service era were less likely than veterans of prior conflicts to seek care. Although research indicates that younger people are more likely to seek care for mental health problems, this pattern does not appear to be true for veterans with PTSD (
19,
22,
44). This finding is somewhat concerning, given the VA's increased attention to PTSD services and multiple efforts to screen for the disorder.
We examined several demographic factors to see if they might explain the difference in use of services by OEF/OIF veterans and veterans of prior service eras. We hypothesized that older veterans were more likely to seek care because they had worse symptomology and more disability. We also speculated that geographical differences influenced care seeking. Compared with younger veterans, older veterans had more service connection, which might explain their greater use of services, but did not differ in comorbidity status. A greater proportion of older veterans than of younger veterans lived in rural areas; this finding was opposite of what would be expected if place of residence affected help seeking by service era.
Other factors that might explain the difference in service use among OEF/OIF veterans and veterans of prior conflicts could not be tested in this data set. They include the possibilities that younger veterans are more likely to believe they do not need care; are prevented from seeking care by more work or family obligations or other circumstances; or are more likely to seek treatment elsewhere, perhaps under a significant other's health care plan.
Patients with more than one health diagnosis made 64% more outpatient visits to the VA than those with only a diagnosis of PTSD. Poor health has long been cited as a factor influencing help-seeking behavior (
19,
45–
47). Some research shows that need factors, such as poor health, are most predictive of service use; such findings suggest that patients who really need care will seek it despite other obstacles. Our study results supported that conclusion.
This study, while informative, was prone to several limitations. Although the outpatient data sets provide a wealth of information about a large number of individuals, the original databases were created and maintained primarily as a clinical and administrative tool. Our lack of direct control limits the type and complexity of information that we can examine and, to some extent, the conclusions we can draw. Further, patient records are entered by multiple providers, resulting in inconsistent data collection and diagnostic evaluation methods. In addition, the information contained in this database included only veterans enrolled in the VA system. A major limitation was the inability to understand factors influencing veterans who have chosen not to use VA-based services.
Because we could not get specific patient addresses, we relied on the Zip Code Crosswalk to assign urban, rural, and highly rural category labels. A potential problem with this method is that some zip codes represent a mix of urban, rural, or highly rural locations. Despite this shortcoming, the Crosswalk has been found to be highly reliable and is accepted by the VA as the gold standard for classification of residence (
48). Given that OEF/OIF is not yet coded as a categorical option in the medical databases, we created a proxy variable that was based on a variable used by other researchers. Because of the inaccuracy of this method, we urge the VA to quickly include OEF/OIF as a service era coding option.
Our findings indicated that geography influenced the number of visits annually, but they did not tell us whether that association had implications for overall health and interpersonal relationships, such as marital or relationship discord. Given that veterans living in rural and highly rural areas sought fewer outpatient visits for PTSD than those living in urban areas, we might conclude that their illness was more severe. That conclusion is supported by research that provides some evidence that veterans living in rural areas have worse health-related quality-of-life scores than those in urban areas (
31,
49).
Conclusions
This study yielded valuable information about service patterns for veterans with PTSD. By investigating veterans' service use over one year, we were able to examine a “snapshot in time” but could not determine long-term patterns. We recommend additional research examining multiyear use of VA services in order to understand patterns of care seeking to inform long-term resource planning.
We also did not explore system-level factors that affect help seeking for PTSD, an area of study suggested by other researchers (
50). There are 21 Veterans Integrated Service Networks (VISNs), each of which is responsible for overseeing, organizing, and directing the facilities in their catchment area. Because of the inherent differences in operations, there is ample opportunity for discrepancies among VISNs in care and utilization. For example, one VISN may be better at providing outreach to rural veterans or offer more transportation opportunities, whereas another VISN might provide more rurally based health care facilities. Future research should explore the impact of system-level variables on patients' health service utilization and give particular focus to services provided by specialized PTSD clinics, which vary considerably.
Acknowledgments and disclosures
This study was funded by the field office of the U.S. Department of Veterans Affairs (VA) Rural Health Resource Center-Western Region in Salt Lake City, Utah. The opinions expressed by the authors do not necessarily reflect those of the VA.
The authors report no competing interests.