A series of observational studies has indicated a sharp rise in recent decades in the use of psychotropic drugs in the pediatric population, and gradually health professionals and the public have raised concerns regarding prescription safety in the younger population (
1–
4). This concern is particularly apparent in relation to issues such as developmental effects of psychotropic drugs, concomitant medication, overprescription, and potential abuse. According to a review of epidemiological studies conducted among pediatric outpatients in Canada, Italy, the Netherlands, the United Kingdom, and the United States, the annual prevalence of use of anxiolytics ranges from 2.5 to 6.9 youths per 1,000, and the estimate for stimulant use is as high as 57.3 youths per 1,000 (
1).
Attention-deficit hyperactivity disorder (ADHD), characterized by the core clinical features of overactivity, impulsivity, and inattention, is one of the most common neurodevelopmental disorders emerging in childhood. A recent meta-analysis of 120 studies published between 1978 and 2005 concluded that ADHD has affected 5.3% of the world’s population; the point prevalence estimates for children and adolescents were 7% and 3%, respectively (
5). In the past decade, medication management and behavioral intervention have been recommended for the treatment of ADHD, and the efficacy of these treatments, particularly psychostimulants such as methylphenidate, in diverse populations, including persons with comorbid psychiatric disorders (
5–
9), has been reported. At the same time, stimulants gradually have become one of the medication categories that warrants most attention because of its high potential for abuse and wide availability through the illegal drug trade (
10,
11). Investigators around the world have made an effort to understand the nature and determinants of problems related to use of stimulant medication by young people (
11–
13), yet the evidence has generally focused on individuals’ nonmedical use and drug diversion behaviors up to now, prescribing-related problems and safety issues have been less explored.
In this study, we first determined and characterized the occurrence of prescription overlap of methylphenidate among youngsters who recently received an initial diagnosis of ADHD. Moreover, to disentangle the complex relationship between service providers and treatment-seeking children, we further used multilevel regression analyses to explore whether certain patients’ and physicians’ characteristics may predict the risk of having overlapping prescriptions for stimulants. Prescription overlap is one of several indicators, including doctor shopping and multiple prescribers, that have been developed to detect psychoactive-drug safety problems (
14–
16); these proxy measures may not only reflect nonadherence to prescription fill or refill (
17) but may also indicate potential risk of abuse and misuse, such as drug diversion and overdose (
14,
16). Our goal is to promote safe, effective, and evidence-based pharmacological treatment of children and adolescents.
The primary source of data for this study was the 1999–2002 National Health Insurance Research Database, which was derived from the National Health Insurance Program (NHIP) for research purposes. Administrative data sets have been accepted as important resources for investigating drug safety problems associated with psychoactive medications, given their better validity compared with self-report (
4,
18). To illustrate, a recent study analyzing the methylphenidate prescription data in the French General Health Insurance System identified a subgroup of users with deviant utilization. These users had a higher number of prescriptions and total dispensed quantity as well as an unusually high number of different prescribers or pharmacies (
19). However, prior studies were largely built on cross-sectional designs and did not acknowledge that prescription utilization patterns and associated problems may change as the treatment progresses. Furthermore, although problems of prescribing safety disproportionately affect subgroups of patients with particular sociodemographic backgrounds, medical conditions, or other comorbidity, few studies have recognized that such problematic events may cluster within individuals or even service providers (
20,
21). Failure to take into account the correlation within patients or physicians may lead to biased estimation of determinants.
Methods
Data sources
Launched in 1995, the NHIP provides a universal health program, including treatments, dental service, preventive medicine, and prescription drugs to eligible residents in Taiwan, and the coverage rate is estimated to reach over 98% of the population who are under 19 years old. For each NHIP enrollee, a unique encrypted identification number is created to retrieve data files covering the registries for beneficiaries, contracted medical facilities, and drug prescriptions. This study was reviewed and approved by the institutional review board of the National Health Research Institutes (EC0990804-E).
Measurement
We identified 3,081 persons who were aged 17 or younger, had received no
ICD-9-CM diagnosis of ADHD (314.xx) during the period 1997–1999, received their first diagnosis of ADHD in the calendar year 2000, and received their first methylphenidate prescription within one year of ADHD diagnosis (
22).Through the 1999–2002 study period, short-release methylphenidate was the only stimulant for ADHD treatment reimbursed by the NHIP.
All records of methylphenidate prescriptions within a year of treatment initiation were retrieved for each patient, and the number of overlapping days for any two successive prescriptions (new, renewal, or refill) was measured. Methylphenidate, classified in Taiwan as a schedule III controlled substance since 1999, may be prescribed only by physicians with a registered license from the Food and Drug Administration to prescribe controlled substances; moreover, the prescription should be written on a special form that includes information about the patient, prescriber, pharmacist, and prescription (such as date of issue, patient’s name, practitioner’s name, and quantity prescribed). The patient or whoever picks up the prescription (for example, a family member) must provide a signature before receiving the methylphenidate.
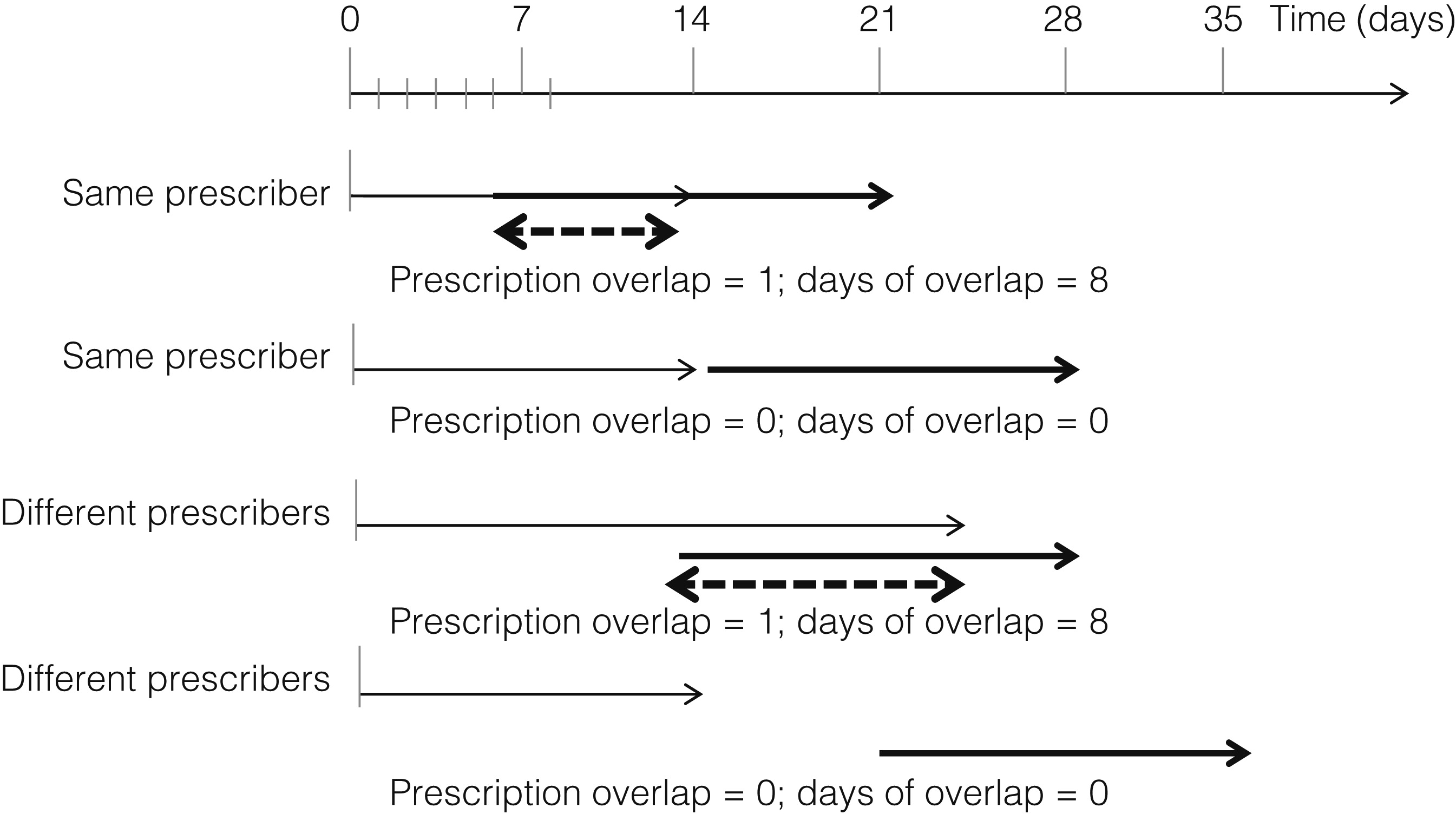
The NHIP regulates that chronic prescriptions cannot be refilled until seven days prior to the end of the last filled prescription, although such regulations are not applied to new and renewal prescriptions. In this study, prescription overlap, defined as an overlap of eight or more days in two successive prescriptions of methylphenidate, was used as a proxy indicator for aberrant prescription utilization.
Figure 1 illustrates examples of prescription overlap.
Multilevel analyses of methylphenidate prescription overlap were conducted for the subset of 2,176 (70.6%) youths with ADHD who had received at least two methylphenidate prescriptions within a year of treatment initiation. For the visits with methylphenidate prescription, we collected information about prescription-level characteristics, including specialty of the prescriber (psychiatry, pediatrics, or other), hospital accreditation (medical center, regional hospital, or community hospital or clinic), region of the medical institution (southern, northern, or central-eastern Taiwan), daily dose (≤10 mg or >10 mg), length of prescription (weeks), and timing of prescription (while school was in session or during vacations) (
22).
Individual-level attributes included age, gender, enrollee’s category (an index of socioeconomic status), residential region, urbanicity, change in prescribing physician, and history of other mental disorders. Age at ADHD diagnosis was grouped into four categories: <6, 6–8, 9–11, and 12–17 years. Enrollee’s category was primarily defined by the job type of the enrollee’s parents or primary caregivers. Category I mainly covered enrollees whose parents were employed by government, government-run businesses, or public educational institutes. Category II covered enrollees whose parents were employed by private business companies. Category III covered enrollees whose parents worked in private educational institutes, fishing, agriculture, or mining, and category IV covered enrollees whose parents were low-income earners or served in the military. On the basis of the enrollee’s registration information, geographical region was classified into northern, southern, or central-eastern region; residential urbanization was grouped by urban, suburban, or rural region (
23). A code of 1 was assigned if the youth with ADHD ever received methylphenidate prescriptions from two or more physicians within a year of treatment initiation. A history of other psychiatric disorders was defined by
ICD-9-CM codes 290–313 and 315–319 in outpatient care records from January 1, 1997, through the day before ADHD diagnosis.
We collected information about characteristics of the physician who prescribed more than 50% of a youngster’s methylphenidate prescriptions, including information about gender, age (<36, 36–45, or ≥46 years), specialty (psychiatry, pediatrics, or other), accreditation of affiliated hospital (medical center, regional hospital, or community hospital or clinic), and region of affiliated hospital (southern, northern, or central-eastern). In addition, the proportion of patients with ADHD receiving methylphenidate at the first appointment was calculated as a proxy measure of physicians’ prescribing practices. Physicians were classified into quartiles on the basis of the proportion of their patients with ADHD prescribed methylphenidate at the first appointment (quartile [Q]1=1%, Q2=6%, and Q3=10%). For analyses, physicians were categorized into two groups above or below a cutpoint of 10%.
Statistical analysis
Individuals’ sociodemographic and clinical characteristics were stratified by pattern of methylphenidate prescription utilization. Chi square and t tests were used to determine whether the groups differed in relation to prescription overlap status. The intraclass correlation coefficient (ICC) values for methylphenidate prescription overlap at individual and physician levels were .38 and .14, respectively, suggesting the existence of clustering effects by individual or possibly service provider. Next, we turned to the two-level random-intercept multilevel regression analyses to assess the effects of characteristics of individuals and service providers on the occurrence of prescription overlap at the visit and the individual levels.
The random-intercept model with logit function was used to analyze the univariate association of prescription overlap at visit level with prescription (level 1) and individual (level 2) characteristics. To take into account temporal sequence, the prescription-level characteristics of the first of two successive visits in which methylphenidate was prescribed were analyzed in relation to the presence of prescription overlap. Next, adjusted odds ratios (AORs) were obtained upon simultaneous statistical control of all prescription-level (level 1) variables (model 1). This step was followed by the introduction into the model of individual-level characteristics (level 2 variables) found by univariate analysis to be significant (p<.05) and simultaneous adjustment for all level 1 variables (model 2). Finally, all variables at the prescription and individual levels were taken into account simultaneously by statistical adjustment (model 3).
Similar analytic strategies were repeated to evaluate the risks of prescription overlap at the individual level by using individual-level (level 1) and physician-level (level 2) characteristics. Confidence intervals were determined with a type I error of 5%. Statistical analyses were performed by SAS 9.01 (
24).
Results
Sociodemographic and clinical characteristics of methylphenidate-treated children and adolescents with newly diagnosed ADHD are summarized in
Table 1. Within a year of methylphenidate treatment initiation, 29% (N=905) received only one prescription and no refill or renewal. Among those who received two or more prescriptions of methylphenidate, 75 (4%) had two successive prescriptions that overlapped for eight or more days. In general, the distribution of sociodemographic characteristics among those with or without overlapping methylphenidate prescriptions did not differ. However, youngsters with prescription overlap were found to be more likely to have other comorbid mental disorders (p<.01) and to have had more prescription visits (p<.001). On average, the number of prescription days was significantly longer for the overlap group (23.6 days; range seven to 30 days) than for the nonoverlap group (20.4 days; range one to 60 days).
The 2,176 youths with recently diagnosed ADHD who had overlapping prescriptions had 11,708 visits with methylphenidate prescription. Multilevel analyses of these visits yielded association estimates for the occurrence of having prescription overlap at the visit level (
Table 2). After taking into account intraindividual correlation, the univariate analyses indicated that several factors, such as having a comorbid mental disorder and receiving a prescription from a regional hospital, had significant effects on having prescription overlap at the visit. After adjustment for all listed individual- and prescription-level characteristics, we found that individuals who lived in a rural area (AOR=2.68) or had ever changed prescribing doctors (AOR=3.04) were more likely to have visits with overlapping prescriptions for methylphenidate (model 3). In addition, receiving a prescription from a regional hospital was associated with 1.65-fold risk of visits with prescription overlap.
Of 248 primary prescribing physicians, 70% were men, 19% were aged 46 years or older, and over one-fifth had prescribed methylphenidate to at least 10% of the patients during a first visit (
Table 3). After simultaneous statistical adjustment for physician- and patient-level characteristics, we found that receiving methylphenidate from doctors aged 46 years or older was significantly associated with increased risk of overlapped prescriptions (AOR=3.62). Youths with a history of other mental disorders were found to have a 1.78-fold risk of having prescription overlap. The risk was elevated to 4.1 for those who changed prescribing physicians within a year of treatment initiation.
Discussion
To the best of our knowledge, this study is one of the first to examine the issue of overlap of prescriptions for methylphenidate among children and adolescents. Our study had several important findings. First, about 3% to 4% of individuals prescribed methylphenidate had prescription overlap within a year of treatment initiation. Second, change in prescribing physicians was a strong predictor of prescription overlap; individuals who changed prescribing physicians had 4.10 greater odds of prescription overlap than individuals who had not changed prescribing physicians. Visits by individuals who changed prescribing physicians were 3.04 more likely than other visits to be associated with prescription overlap. A history of comorbid mental disorders and rural residence were also linked with moderately increased risk of prescription overlap. Youngsters who received methylphenidate from physicians aged 46 years or older were 3.62 times more likely to have prescription overlap.
Several limitations should be considered when interpreting study results. First, because of the small number of individuals (N=75) with prescription overlap, we were unable to obtain converged estimates for the multilevel cross-classified model that took into account the characteristics of all prescribing physicians. To reduce potential misclassification bias associated with limiting data collection about prescribers to the “primary prescribing physician,” post hoc analyses indicated that 86% to 87% of prescription overlap occurred during the visits to primary prescribing physicians. Repeated multilevel analyses of the same subset of data yielded similar results. Also, given the relatively imprecise nature of association estimates, we were not able to use the three-level model to examine the effects of physician, individual, and prescription attributes on the visit in which the prescription overlap occurred. Finally, the study population was limited to young people, so our results may not apply to other age groups. They may also not apply to societies that have health care systems or insurance plan policies different from Taiwan’s.
This study had several strengths. First, the design was based on a retrospective, longitudinal study with a large, nationally representative population of over 3,000 young people who had recently received the diagnosis of ADHD. The study design allowed the data to fully inform potential treatment problems within a year of diagnosis. Also, the robust and unique nature of the NHIP data on pharmacoservice utilization provides a valuable opportunity to investigate probable problematic prescribing behaviors or medication utilization in the health care system; such data would be more difficult to obtain and would be less likely to be accurate if they were from self-reports by children and adolescents. Finally, a major strength of this study is the disentangling through a multilevel statistical approach of physician-, individual-, and prescription-level effects on prescription overlap, which takes intraprovider and intrapatient clustering effects into account and adjusts for a rather comprehensive list of factors simultaneously. In view of this analysis, the association estimates, in essence, are likely to yield the most reliable and valid results of any analyses of relatively large groups.
In the context of a universal health care system that requires that prescriptions for chronic disorders be refilled no sooner than seven days prior to the end of the last filled prescription, our descriptive analyses indicated that prescription overlap occurs disproportionally among persons who had other comorbid mental disorders, had a longer period of methylphenidate prescription, or changed prescribing physicians. Considering that children and adolescents are vulnerable to the adverse effects of stimulant medication and associated problems (
9–
13,
25), it is recommended that medication treatment be planned with close monitoring and coordination among service providers, such as physicians and pharmacists (
26,
27). Also, persons with other mental disorders may be a subgroup that should be targeted when devising interventions to reduce prescription overlap or associated problems (
7,
9,
28,
29).
An interesting finding is that individual sociodemographic characteristics—such as age, gender, and socioeconomic status—were not associated with prescription overlap. Our restriction in age range (<18 years) may have increased the homogeneity of our sample; in addition, differences associated with socioeconomic status may be fewer among those who seek mental health care and receive medication treatment (
30,
31). In terms of rural residence, prior studies have shown that children with special needs living in rural areas were more likely than those living in other areas to face marked difficulties in obtaining comprehensive mental health services (
32–
34). Further post hoc analyses found that the youngsters with rural residence were more likely than their peers with urban residence to change prescribing physicians and receive methylphenidate prescriptions from clinics or community hospitals. Because physician visits by young people, particularly children, usually require parents or primary caregivers to adjust their schedules, parents may visit the prescribing physician on weekend earlier than scheduled weekdays to avoid losing further time at work. In some cases parents might change prescribing physicians or even obtain stimulant medications from multiple doctors. Our results may indicate that in order to provide safe and effective medication treatment for ADHD, access to a continuum of pharmacological services, such as service providers with a registered license to prescribe controlled substances, and coordinated referral for children with mental health problems, especially those in rural areas, must be provided.
The findings of this study, similar to those of prior studies (
26,
35,
36), indicate that treatment of and prescribing practice for ADHD may depend on the physician’s age. Our rigorous analyses suggested that older age may be one of the most important factors governing prescribing habits. Continuing medical education should address guidelines and regulations concerning use of scheduled prescription drugs in order to promote physicians’ adherence to prescription guidelines and to increase awareness of prior or concomitant use of scheduled medications by children and adolescent populations, particularly at patients’ first visits.
Conclusions
This study found that prescription overlap occurred disproportionately among youngsters with rural residence, comorbid mental disorders, a change in prescribing physician, and receipt of prescription from a physician aged 46 years or older. Our findings have several implications for clinical practice and future policy initiatives. Physicians should take note of a patient’s history of use of controlled prescriptions at first visit and be alert to requests for unscheduled refills. In an effort to reduce safety problems associated with use of controlled prescriptions in a younger population, programs should be devised to monitor indicators at the level of both service provider and patient (
36).
Acknowledgments and disclosures
Funding for this study was provided by the National Health Research Institutes (NHRI) (99A1-PHPP45) and a grant from the Taiwan Ministry of Education’s Aim for the Top University Plan. The authors thank the individuals who manage the National Health Insurance Research Database in NHRI’s Department of Research Resources. NHRI had no further role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
The authors report no competing interests.