Research has revealed pervasive and persistent negative attitudes among Americans toward persons with mental illness. A study that compared 1999 and 2006 data from the General Social Survey (GSS) indicated surprisingly little change over time in high rates of stigma—in particular, the desire for social distance and perceptions about the dangerousness of persons with serious mental illness (
1). Less information is available on public attitudes toward persons with drug addiction, and available data are dated. These data suggest that public views about individuals with drug addiction are more negative than those about persons with mental illnesses (
2).
In the current environment, widespread efforts are aimed at integrating services for treating addiction and policies supporting such treatment into the mainstream of what we now refer to as “behavioral health.” From a clinical and delivery system perspective, this approach makes sense given the sizable share of individuals with mental illness who have a co-occurring substance use disorder (
3). It is unclear, however, whether this push toward integration reflects how the general public conceptualizes these conditions. We know little about how public attitudes about drug addiction differ from attitudes about mental illness. We conducted a Web-based national public opinion study (N=709) to compare public attitudes in four domains: stigma, discrimination, treatment effectiveness, and policy support.
Methods
Between October 30 and December 2, 2013, we designed and fielded a Web-based national public opinion survey of 709 adults aged 18 and over by using the survey research firm GfK Knowledge Networks (GfK). GfK has recruited a probability-based online panel of 50,000 adult members, including persons living in cell phone–only households, using equal probability sampling with a sample frame of residential addresses covering 97% of U.S. households. The GfK panel recruitment rate was 16.6%. To minimize concerns about priming, the order of the survey items was randomized. The survey completion rate, defined as the proportion of GfK panel members randomly selected for this study who completed the survey, was 70%.
Respondents were asked about their attitudes toward either drug addiction or mental illness. We used a split-sample approach so that about half of the 709 respondents (N=347) were randomly assigned to answer each survey question with reference to drug addiction and about half (N=362) with reference to mental illness. We compared their sociodemographic characteristics and confirmed that there were no significant differences between the two groups. [A table presenting unweighted and weighted data on sociodemographic characteristics of the sample and of the U.S. population with rates from the 2013 Current Population Survey is available in an online
data supplement to this report.] Consistent with national rates, in the weighted sample, 51% (N=359) were female, 34% were nonwhite (N=189), and the mean age was 47±.75.
First, we asked two stigma questions measuring desire for social distance from persons with drug addiction or mental illness. Respondents randomly assigned to the mental illness version of the questions were asked: “Would you be willing to have a person with mental illness marry into your family?” and “Would you be willing to have a person with mental illness start working closely with you on a job?” For respondents randomly assigned to the drug addiction variants of these items, the words “mental illness” were replaced by “drug addiction.” The wording for these items was adapted from the 2006 GSS (
1).
Second, to measure attitudes about the acceptability of discrimination, we included three survey items (with separate mental illness and drug addiction variants): “Discrimination against people with drug addiction/mental illness is a serious problem.” “Employers should be allowed to deny employment to a person with drug addiction/mental illness.” “Landlords should be able to deny housing to a person with drug addiction/mental illness.” Third, two items measured respondents’ attitudes about the effectiveness of treatment: “The treatment options for persons with drug addiction/mental illness are effective at controlling symptoms.” “Most people with drug addiction/mental illness can, with treatment, get well and return to productive lives.” The latter item has been used in the GSS as a measure of recovery (
1).
Finally, we gauged respondents’ support for four different policy items: insurance parity and government spending on treatment, housing, and job support. These items were worded as follows: “Do you favor or oppose requiring insurance companies to offer benefits for the treatment of drug addiction/mental illness that are equivalent to benefits for other medical services?” “Do you favor or oppose increasing government spending on the treatment of drug addiction/mental illness?” “Do you favor or oppose increasing government spending on programs to subsidize housing costs for people with drug addiction/mental illness?” “Do you favor or oppose increasing government spending on programs that help people with drug addiction/mental illness find jobs and provide on-the-job support as needed?” All responses were measured with 7-point Likert scales. Each of the 7-point Likert scales was collapsed to a dichotomous measure for presentation below.
We used Pearson chi square tests to assess whether public attitudes differed by whether respondents viewed the drug addiction or mental illness version of the item. In addition, we ran logistic regression models to examine associations between respondents’ attitudes and their sociodemographic characteristics, including age, gender, race-ethnicity, education, and self-identified political affiliation (Republican, Independent, or Democrat). All analyses incorporated survey weights to produce nationally representative estimates by accounting for panel selection deviations, panel nonresponse and attrition, and survey-specific nonresponse.
Results
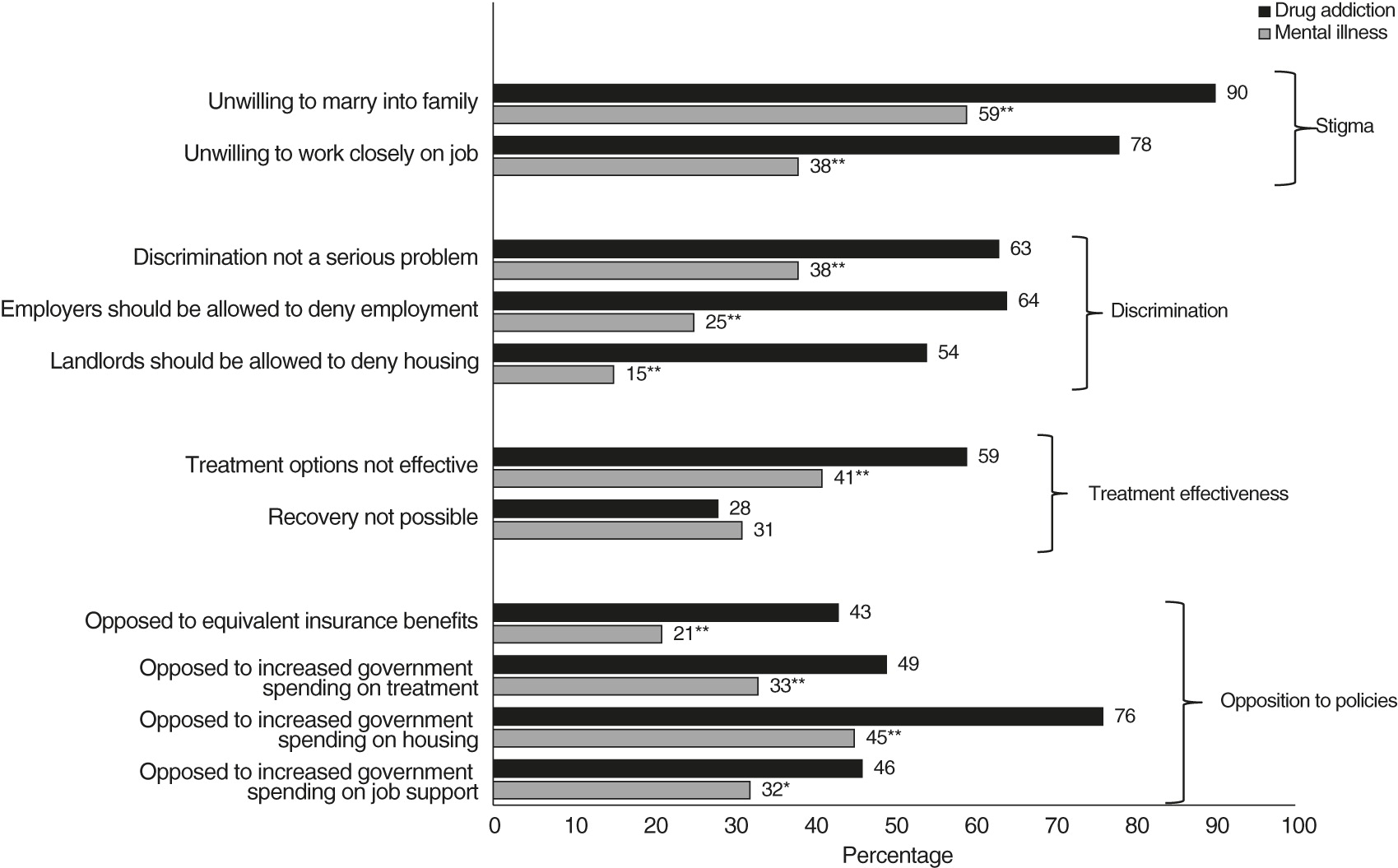
As
Figure 1 indicates, Americans hold significantly more negative attitudes toward persons with drug addiction than toward those with mental illness. We identified very high levels of desire for social distance in both groups; however, a far larger proportion of respondents were unwilling to have a person with drug addiction marry into their family (90% versus 59%, p<.001) or work closely with them on a job (78% versus 38%, p<.001).
Respondents were also more likely to view discrimination against persons with drug addiction as “not a serious problem,” compared with discrimination against persons with mental illness (63% versus 38%, p<.001). Sixty-four percent of respondents thought employers should be allowed to deny employment to persons with drug addiction, compared with 25% who held a similar view about persons with mental illness (p<.001). Similarly, 54% thought landlords should be allowed to deny housing to a person with drug addiction, compared with only 15% who had a similar view about persons with mental illness (p<.001).
With regard to beliefs about treatment effectiveness and recovery, respondents were significantly more likely to view treatment options for persons with drug addiction as ineffective in controlling symptoms, compared with treatment options for persons with mental illness (59% versus 41%, p<.001). However, a roughly equal share rejected the concept that persons with these conditions could get well with treatment and return to productive lives (28% for drug addiction versus 31% for mental illness).
Respondents reported higher levels of opposition to public policies directed at helping people with drug addiction, compared with persons with mental illness. Respondents were significantly more likely to oppose insurance parity for drug addiction than for mental illness (43% versus 21%, p<.001), to oppose increased government spending on drug addiction treatment than treatment for mental illness (49% versus 33%, p<.001), to oppose increased government spending on programs to subsidize housing costs for people with drug addiction than for those with mental illness (76% versus 45%, p<.001), and to oppose increased government spending on job support programs for people with drug addiction than for those with mental illness (46% versus 32%, p<.01).
Finally, we found that political party affiliation was in almost all cases significantly associated with support for the four policies in both the drug addiction sample and the mental illness sample, when the analysis controlled for respondents’ demographic characteristics. In both the drug addiction and mental illness arms, respondents who self-identified as Democrats were significantly less likely than Republicans and Independents to oppose equivalent insurance benefits or to oppose increased government spending on treatment, housing, and job support (results not shown and available from authors upon request).
Discussion
These findings indicate that the American public holds significantly more negative attitudes toward persons with drug addiction than toward those with mental illness, and these attitudes translate into lower support for policies to improve equity in insurance coverage or to increase government funding in support of better treatment rates and housing and job support options. Less sympathetic views may result at least in part from societal ambivalence about whether to regard substance abuse problems as medical conditions to be treated (similar to other chronic health conditions, such as diabetes or heart disease) or personal failings to be overcome. More so than mental illness, addiction is often viewed as a moral shortcoming (
1), and the illegality of drug use reinforces this perspective. It is likely that socially unacceptable behavior accompanying drug addiction (for example, impaired driving and crime) heightens society’s condemnation.
The only dimension in which attitudes did not differ was the belief in the potential for recovery. However, the belief in recovery may be driven by a pull-yourself-up-by-your-bootstraps attitude in the context of drug addiction rather than by the philosophy that has driven the recovery movement in the context of persons with lived experience of mental illness.
One potential limitation of our approach is that when asked about mental illness, some respondents may have embedded their views on drug addiction in their responses, which would have the practical effect of masking even greater differences in attitudes. Another limitation is that we were not able to distinguish between specific conditions within mental illness and drug addiction. We would expect that the desire for social distance from persons with schizophrenia and from those with an anxiety disorder might differ and that public perceptions about the acceptability of discrimination might depend on whether a person had developed an addiction to prescription pain medication after a back injury or was addicted to heroin. Likewise, we did not compare public attitudes toward persons with alcohol abuse. Understanding public attitudes about alcohol is critical because the prevalence of dependence on alcohol is much higher than for any other drug (
4).
Conclusions
Although the behavioral health field is increasingly emphasizing integration, our results suggest that it may be necessary for advocates to adopt differing approaches for advancing stigma reduction and policy goals given underlying differences in public beliefs and attitudes about drug addiction and mental illness. One approach to stigma reduction holds promise. Research on HIV supports the notion that increasing public recognition of treatability can reduce stigma and discrimination toward affected persons (
5,
6). It would be worthwhile to better understand how portraying addiction or mental illness as treatable might lower stigma among the general public, which has grown accustomed to seeing media portrayals of untreated individuals with mental illness or drug addiction as disheveled, often homeless, and potentially dangerous.
Acknowledgments and disclosures
Dr. Barry and Dr. McGinty acknowledge funding from a research grant from AIG Inc. (principal investigator, Dr. Barry). Dr. Barry acknowledges funding from grant R01 DA026414 from the National Institute on Drug Abuse (principal investigator, Dr. Barry). Dr. Barry, Dr. McGinty, and Dr. Goldman acknowledge funding from grant 1R01MH093414-01A1 from the National Institute of Mental Health (principal investigator, Dr. Barry). Data for this study were collected through Time-Sharing Experiments for the Social Sciences, National Science Foundation (grant 0818839). Dr. Pescosolido acknowledges support from an infrastructure grant from the College of Arts and Sciences, Indiana University.
The authors report no competing interests.