Homeless persons have high rates of illness and fragmented health care utilization (
1–
3). Supported housing programs, which offer permanent, community-based housing with supportive services, improve the health and housing of homeless consumers (
4–
7). Yet many consumers who enroll in supported housing programs disengage prematurely, before receiving permanent housing. We know little about factors associated with such disengagement.
This population is of interest to the U.S. Department of Veterans Affairs (VA), which aims to end homelessness among veterans (
2,
8). Toward this aim, the VA partners with the U.S. Department of Housing and Urban Development (HUD) in the HUD-VA Supported Housing (VASH) program, which provides subsidized housing with supportive services (
2,
9,
10) and has served >60,000 consumers (
11). However, nationwide, 18% of participants never achieve housing after program enrollment (
10), often with negative outcomes (
4).
A review of evidence-based interventions for homeless persons highlighted supported housing’s utility in improving housing tenure and substance use disorders and decreasing hospitalizations (
12). Supported housing builds from the tenets of Housing First, which differs from the “linear” approach to services, by which consumers progress through shelters, transitional housing, residential treatment, and independent housing with longitudinal mental health treatment (
13,
14). A cardinal difference between the linear approach and Housing First is that the latter detaches housing and health care, facilitating permanent housing regardless of health care engagement (
13,
14). Housing First programs offer health care referrals without treatment or sobriety mandates. HUD-VASH is considered a Housing First “variant” (
14). That is, the program provides homeless consumers with permanent housing, without treatment or sobriety mandates (
10,
14). However, between enrollment and housing placement—although consumers can choose to live on the streets or in community-based shelters—many use VA transitional housing, which uses a linear approach (
10,
14).
A multisite, quantitative study identified several factors increasing homeless consumers’ risk of exiting HUD-VASH: days intoxicated in the month before enrollment, lower income, and institutionalization history were associated with shorter program tenure (
10). Several studies have explored differential HUD-VASH housing outcomes for consumers with substance use disorders (
4,
15) and criminal justice histories (
16), yet we are unaware of research studying factors associated with premature disengagement from supported housing programs—before housing placement—in the VA or elsewhere.
This article describes consumer characteristics associated with “negative exits” from supported housing, defined as premature program exits, before housing placement, for reasons other than improved finances or social connections. We characterize housing outcomes for consumers with negative exits. To inform intervention development that improves consumer engagement and housing outcomes, we identify modifiable patient-level factors associated with negative exits.
Methods
Participants
We used the VA Homeless Operations Management and Evaluation System (HOMES)—an administrative data set of VA homeless service utilization—to obtain a roster of VA Greater Los Angeles’ (GLA) supported housing enrollees between 2011 and 2012. We identified consumers with negative exits before the end of 2012 (“exiters,” N=71) and those housed before the end of 2012 (“stayers,” N=1,772).
Rather than identifying demographic characteristics conferring risk of exits, we sought to define malleable factors associated with exits by using demographic characteristics to match exiters with stayers. Because these characteristics are optional HOMES entries (not entered by a subset of case managers), we excluded individuals without known demographic characteristics, leaving 72% of exiters (N=51) and 65% of stayers (N=1,153). Client loads are evenly divided among case managers and account for the complexity of consumers’ psychosocial circumstances and diagnoses. Individuals with demographic data were presumed to comprise a representative sample.
Our final analytic sample (N=102) included all 51 exiters, matched 1:1 on age (±5 years), gender, marital status, and race-ethnicity with stayers. The GLA Institutional Review Board approved the study procedures.
Conceptual Framework
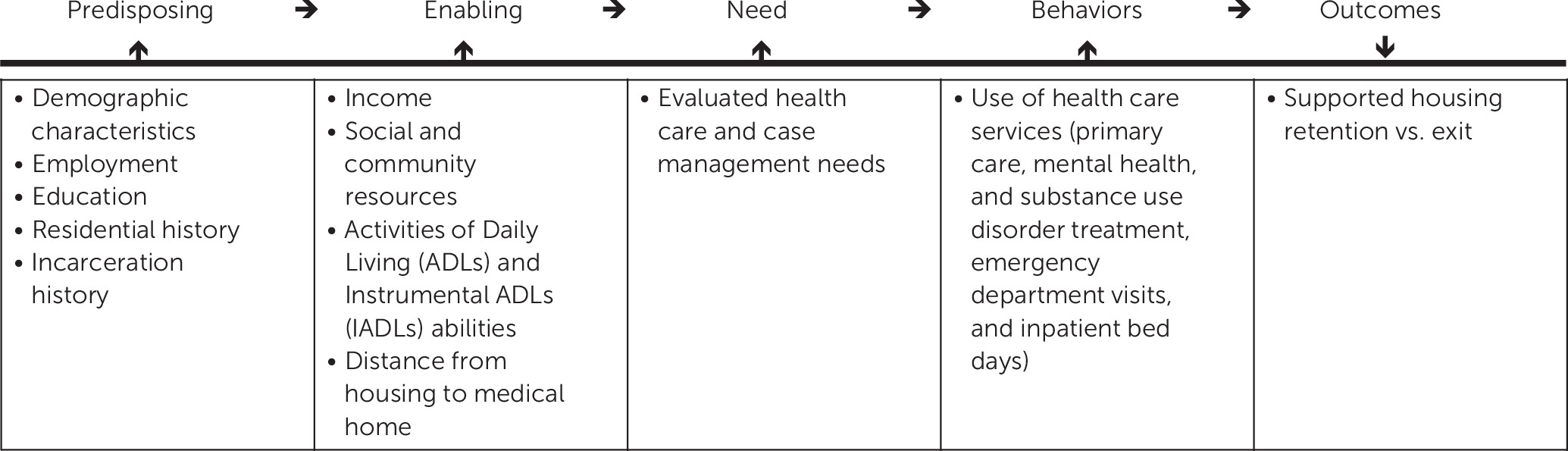
We used the Gelberg-Andersen behavioral model for vulnerable populations (
17), an adaptation of the Andersen model (
18–
20) that includes domains aligned with homeless consumers. This framework identifies factors predisposing individuals to access services (demographic characteristics and employment), which interact with enabling factors (personal, organizational, and community resources) and needs (perceived by patients and providers) to influence behaviors (service use) and outcomes (
17).
Figure 1 depicts our framework, modified to the outcome of supported housing retention versus exit.
Procedure
A group of GLA-supported housing clinicians identified factors that—in their experiences—influenced consumers’ case management “acuity.” These factors comprise a ten-variable instrument with associated Likert scales, described below and known as the Acuity Scale. We conducted a retrospective chart review of all participants, adapting the Acuity Scale to include additional variables from the Gelberg-Andersen model (
17) and entering data into a Web-based template. Because HOMES is restricted to VA homeless program data—and lacks the breadth of variables from our conceptual framework, such as diagnoses—we abstracted data from local medical records, using HOMES solely to generate the program roster. [All variables reviewed are listed in an
online data supplement, which notes variables derived from the Acuity Scale.] One author established the abstraction protocol and trained other reviewers in usage. All reviewers abstracted five consumers’ charts to establish reliability. No major discrepancies were revealed, and minor discrepancies were resolved iteratively.
Measures
Predisposing and enabling factors.
We obtained demographic characteristics (age, gender, marital status, and race-ethnicity) from the program roster.
Vocational activities, residential history, and criminal justice involvement were captured with the Acuity Scale. At program enrollment, case managers complete an “admission note” template with data needed to code these variables. This template includes consumers’ self-reports of competitive employment, irregular employment, vocational rehabilitation, or schooling. It indicates individuals who are identified by case management staff as chronically homeless (
21), defined at enrollment as continuously homeless for one year or more or having four or more episodes of homelessness within the past three years. Incarceration history is also listed, stratified into active probation or parole, history of justice involvement without active probation or parole, and no justice involvement.
Most enabling variables were also in the Acuity Scale. GLA clinicians associated income ranges with levels of ease of living in Los Angeles–based supported housing. Consumer-reported income is documented in the admission note template, and we used this information to categorize consumers: >$1,800 per month, $1,400–1,800 per month, $750–$1,359 per month, $301–$749 per month, and ≤$300 per month. All consumers met HUD-specified subsidized housing income limits (
22).
The presence or absence of consumer-endorsed social support was abstracted from the admission template. We also used this record to note whether consumers reported independence in activities of daily living (ADLs) and instrumental ADLs (IADLs) or whether they required assistance. We noted the distance from the individual’s residence (often a street corner or transitional housing) at program enrollment to his or her assigned medical home (or nearest VA facility for consumers lacking medical homes). The admission template identifies this residence, and the chart notes medical home assignments.
Needs and behaviors.
The presence or absence of common chronic medical conditions, psychiatric disorders, and substance use disorders were used to capture evaluated need. Medical conditions were identified from a list of common outpatient diagnoses from the National Ambulatory Medical Care Survey (
23), supplemented by common conditions among homeless men (
24,
25). These conditions included cancer, coronary artery disease, congestive heart failure, chronic pain (generalized, or localized to the back or a joint), chronic obstructive pulmonary disease (COPD), diabetes, dyslipidemia, hepatitis C virus (HCV), HIV/AIDS, hypertension, and stroke. Psychiatric disorders encompassed a breadth of
DSM-IV axis I conditions, including depression, bipolar disorder, other mood disorders, posttraumatic stress disorder (PTSD), other anxiety disorders, and psychotic disorders. Substance use disorders (regardless of whether active or in remission) were stratified into alcohol use and drug use disorders. Diagnoses were obtained from the medical record “problem list” (a list of diagnoses, by patient) and notes from inpatient admissions and discharges, the emergency department, primary care, and subspecialty consultations from January 1, 2011, to December 31, 2012. Because these diagnoses reflect chronic conditions, we reviewed this time frame regardless of consumers’ supported housing admission dates. We also noted whether the admission template documented consumers’ self-report of substance use disorders as active or in remission.
The main behavior variable was the frequency of VA health care utilization, which captured the number of emergency department, inpatient admissions (medical-surgical and mental health), primary care visits, and mental health visits (with psychiatrists or psychologists) from one year before each consumer’s supported housing admission (ranging from January 1, 2010, to December 31, 2011) to one year later. Length of stay was recorded for admissions. Adherence to outpatient medical-surgical visits and mental health care over this time was calculated by comparing the number of “missed appointment” notations (excluding cancelled appointments) with the total number of appointments. This ratio was translated to a Likert Scale, ranging from 0, attends all appointments, to 4, no adherence. We captured each consumer’s number of supported housing social worker contacts between admission and housing (stayers) or discharge (exiter) dates. We noted (at the time of admission to supported housing) whether consumers were enrolled in outpatient substance use disorder treatment or assertive community treatment (ACT)—which offers intensive, interdisciplinary, field-based case management (
26).
Outcomes.
The program roster classified consumers as exiters versus stayers. We noted time lapsed between program enrollment and disengagement (exiters) versus housing (stayers). For exiters, we used the first informative note after program discharge (dated a median of 11.5 days after program discharge) to identify their next known living situation.
Analyses
We used the chi square test and analysis of variance to determine how predisposing, enabling, need, and behavior variables varied between exiters and stayers. For Likert scale data, we collapsed successive categories with total frequency ≤5% and used logistic regression to identify between-group differences. Analyses were performed in Stata/SE 12.1 (
27).
Next, we used recursive partitioning to identify which combination of predictor variables and corresponding values best differentiated exiters from stayers. Recursive partitioning is a data-mining technique that uses decision trees to predict outcomes from predictor variables (
28–
30). In particular, this methodology facilitates exploration of complex and potentially overlapping predictor variables and is better suited than regression analyses for studies with large numbers of predictors versus sample size (
28,
29). Here, analysis began by independently evaluating each variable on our outcome (exiter versus stayer). The variable and its corresponding cut-point (or value) that best split data by this outcome was selected as the first predictor, or the first two “branches” of the decision tree (
28–
30).
Subsequently, this process was repeated on each of the two newly created subsamples, again identifying the variable and its value that best predicted the most homogenous subsamples within each previously formed branch. Branching continued until there was no further improvement in correct differentiation of participants by outcome, a process that aimed to simplify a complex set of potential predictor variables into a few simple “if-then” rules that predicted outcomes (
28–
30). Given our large number of predictor variables versus sample size, we used a ten-fold cross-validation approach (
31,
32), splitting our sample into ten random groups of approximately equal size to approximate the analysis of a different sample drawn from the consumers of this supported housing program (
28). Cross-validation aimed to determine which predictors were likely generalizable to any other sample from this population (versus due to overfitting). These analyses were performed with the recursive partitioning algorithm in the rpart package version 3.1–33 for the R language and environment (
33).
Results
Predisposing and Enabling Factors
Table 1 displays sample demographic characteristics and baseline characteristics. Exiters and stayers were matched 1:1 on demographic characteristics. Participants’ average age was 53±10 years; most (96%) were male. Many (47%) were divorced, 29% never married, and 8% were married or partnered. Most (55%) participants were African American, with fewer Caucasians (24%) and Hispanics/Latinos (22%).
There were no significant between-group differences in rates of chronic versus acute homelessness. More than twice as many exiters as stayers were on probation or parole at enrollment (29% versus 14%). More exiters than stayers (40% versus 24%) indicated having active substance use disorders. Most consumers (65% of total) lacked vocational activities.
Although both groups had similar distances between their residence at program enrollment and their medical home, all consumers in transitional housing facilities on VA grounds at program enrollment were exiters (29% of exiters). There were no significant between-group differences in income, presence versus absence of social support, or ADL/IADL independence.
Needs and Behaviors
Rates of cancer, coronary artery disease, diabetes, congestive heart failure, COPD, diabetes mellitus, dyslipidemia, HIV/AIDS, hypertension, and stroke were similar between groups. Two diagnoses were significantly higher (p<.05) among exiters versus stayers: chronic pain (exiters, N=28, 55%; stayers, N=17, 33%) and HCV (exiters, N=20, 39%; stayers, N=11, 22%). Bipolar disorder, cognitive disorders, depression, PTSD, other anxiety disorders, and psychotic disorders were similar between groups. Alcohol and drug use disorders were significantly associated (p<.05) with exiting: 71% of exiters had an alcohol use disorder and 79% had a substance use disorder, versus 49% and 61%, respectively, of stayers.
Table 2 displays health care utilization data. Compared with stayers, exiters used more primary care over two years (9.3 visits versus 6.6 visits), although the difference was not significant. Exiters were more likely to have one or more inpatient medical-surgical admissions (26% versus 8%) and used more emergency department services (75% versus 45% with one or more visits). Rates of mental health care utilization were similar between groups, as was the number of supported housing social worker contacts during program enrollment (13.5 for exiters versus 16.9 for stayers). However, stayers had significantly better adherence to outpatient medical and mental health care. Only one consumer was enrolled in ACT, and there were no significant between-group differences in substance use disorder treatment rates among consumers with this diagnosis.
Outcomes
There were no significant between-group differences in duration of program engagement (stayers averaged 212.9 days between enrollment and housing, whereas exiters averaged 190.3 days between enrollment and discharge). National VA data show a median of 185 days between enrollment and housing in this program (
10).
Table 3 shows exiters’ housing outcomes. Immediately after disengagement, about one-third of exiters (31%) became homeless on the streets. Nearly one-quarter (24%) became incarcerated, and 22% entered residential rehabilitation. Only 12% secured temporary housing with friends or family.
Recursive Partitioning
In recursive partitioning, the 42 aforementioned predisposing, enabling, need, and behavior variables were used as potential predictors of exiting versus staying. [The best possible model for these data is shown in the online supplement and highlights two variables—transitional housing on VA grounds during program enrollment and adherence to outpatient medical-surgical care—that were sufficient to capture information from all predictors to classify participants as exiters versus stayers.] Consumers living on VA grounds at program enrollment were predicted to exit. Among those living elsewhere, individuals with “excellent” adherence (attended all appointments) to medical-surgical care were predicted to become stayers.
This decision tree correctly classified 55% (28 of 51) of exiters and 92% (47 of 51) of stayers (74% correct classifications overall). It misclassified 45% (23 of 51) of exiters and 8% (four of 51) of stayers (26% misclassifications overall); this performance represents a 48% reduction of the misclassification rate compared with a coin flip (50% misclassification). Using cross-validation to check for overfitting, we expected a misclassification rate of 33% in any other sample selected from the population of consumers in this supported housing program (34% reduction versus coin flip). If we consider this decision tree as a diagnostic test for exiting supported housing, it had a sensitivity estimate of .87 (95% confidence interval [CI]=.70–.95) and a specificity estimate of .67 (CI=.55–.77).
Discussion
We identified factors significantly associated with premature disengagement from a supported housing program before housing placement: residing in transitional housing on hospital grounds during program enrollment, poor adherence to outpatient care, substance use disorders, HCV, chronic pain, justice involvement, frequent emergency department utilization, and medical-surgical admissions. Moreover, we found that exiters had poor housing outcomes: >50% were street homeless or incarcerated shortly after disengagement.
We question whether these findings stem from challenges in implementing supported housing programs with strong fidelity to Housing First. Although Housing First is rooted in case management with rehabilitation (
10,
34), with an aim to facilitate rapid housing placement without treatment mandates, research indicates that VA supported housing case managers often initially focus on housing placement (versus rehabilitation, such as for substance use disorders) (
10). With time, case management activities shift to “monitoring” and “supportive care”—again, versus rehabilitation (
4). That is, although this program has fidelity to some components of Housing First (housing placement without treatment or sobriety mandates), there is less fidelity to rehabilitation services that could address factors associated with negative exits.
In this matched sample, all consumers in transitional housing on hospital grounds during program enrollment were exiters. These transitional housing services mandate sobriety while offering short-term shelter (with or without mental health care), but they have eligibility criteria equivalent to those in the supported housing program. Future studies could explore consumer preferences for hospital- versus community-based transitional housing and characterize the experience of hospital-based transitional housing with a focus on rehabilitation services (and unmet rehabilitative needs). Such work could inform the implementation of services, adapted to this setting, to address factors associated with negative exits.
Beyond these factors, specific diagnoses were associated with exiters. The association between substance use disorders and exits builds on literature describing a dearth of Housing First outcome data for consumers with severe substance use disorders (
14). Injection drug use is the strongest predictor of HCV (
35), and substance use disorders are highly prevalent among homeless consumers with chronic pain (
36). Associations between these diagnoses and exiters may reflect an underlying association with substance use disorders.
Specific health care utilization patterns were also associated with exiters. Interestingly, although homeless persons typically underuse primary care (
17,
37), exiters used more primary care than stayers. Because exiters also had more emergency department use, more medical-surgical admissions, and worse adherence to outpatient care, future research could explore whether different primary care modalities—like a homeless-focused primary care clinic (
8)—might influence supported housing engagement (versus visit frequency).
This study had limitations. We studied consumers at one urban VA (with a large homeless population) (
38). This supported housing program had fewer exiters (4%) compared with those reflected in national figures (18%), so these data may face barriers to external validity in other communities (inside or outside the VA). We lacked data about this program’s fidelity to Housing First during the study period. We reviewed medical records, which are subject to documentation variations. Records were largely derived from self-report or clinician diagnoses, without confirmation from other sources, such as laboratory values. Future work would benefit from use of validated assessments, such as for symptoms, diagnostic confirmation with laboratory tests, inclusion of national VA data (because consumers may receive care across facilities), and review of non-VA records. Last, although recursive partitioning facilitates exploration of complex and potentially overlapping predictors–and although cross-validation enhances generalizability–results of these analyses were based on this sample. We were limited by the representativeness of our sample to the larger population and the extent to which variables measured represented the underlying constructs of our conceptual framework. We also note that the wide CI of our sensitivity and specificity estimates suggests the benefits of replicating these methods with a larger sample.
Conclusions
Diverse social factors, diagnoses, and health care utilization patterns were associated with premature disengagement from supported housing. In future studies, these findings could be enhanced with qualitative data; consumer narratives may enrich our understanding about the nature of linkages between factors identified here as associated with exits from supported housing. Future work could also implement and test rehabilitative services—aligned with Housing First and adapted to supported housing—that address identified factors and have potential to improve outcomes for homeless consumers.
Acknowledgments
This material is based on work supported by a VA Mental Health Quality Enhancement Research Initiative (QUERI) Recovery Workgroup Locally Initiated Project. The authors thank Pamela Harris, R.N.-B.C., B.S.N., Melody Jazeb, L.C.S.W., Au Sam Ha, L.C.S.W., Ronald M. Andersen, Ph.D., Lillian Gelberg, M.D., M.S.P.H., Adrian Alexandrino, Jr., B.A., and David A. Smelson, Psy.D., for their contributions to the manuscript. The contents of this article are those of the authors and do not represent the views of the U.S. Department of Veterans Affairs or the U.S. government.