Despite more than 50 years of efforts to bolster community mental health treatment, state psychiatric hospitals continue to play a critical role in U.S. mental health services. When outpatient services are unable to help people prevent or manage crises, swift access to inpatient care in community general hospitals can be essential to ensure safety while medications are recalibrated and formal and informal supports are organized. However, general hospital psychiatric units often lack the resources to manage severe symptoms or violent or otherwise disruptive behavior. The results can be costly for health care providers, patients, families, and communities. Responding to a single patient’s violent behavior can require the resources of an entire general hospital ward or emergency room.
The severe shortage of all types of psychiatric beds across the United States (
1–
3) affects not only whether people are admitted for inpatient treatment but also how long they wait for a bed. In a 2012 national survey, 13 state mental health agency directors reported that waitlists for state hospital beds increased as a result of psychiatric bed shortages (
3). Some emergency departments in general hospitals have resorted to boarding people in psychiatric crisis for days while they wait for a bed to become available (
4). In these circumstances, detained individuals can receive treatment only for life-threatening conditions—not for routine psychiatric care.
In contrast to community general hospitals, state psychiatric hospitals are designed and staffed to care for people with severe mental illness, including those who may become violent. Observers now believe that state hospitals will continue to serve patients whom general hospitals and private psychiatric hospitals cannot accommodate (
5). In this respect, state psychiatric hospitals are the ultimate safety net for people with mental illness.
Despite the important safety-net role of state psychiatric hospitals, to our knowledge no previous study has developed a management tool to assist these hospitals in calibrating their capacity and routines so as to increase access to inpatient beds. Simulation models are well suited to address this gap because they quickly provide “what if” results without requiring actual implementation of costly and possibly ineffective interventions. The purpose of this study was to create and test a discrete-event simulation model (
6) to evaluate supply-side interventions for decreasing state hospital wait times. We characterize our approach as “supply side” because we held constant the level of community demand for state psychiatric hospital beds as we explored what the hospital itself could do to reduce wait times.
Methods
Study Setting
The hospital under study is one of three state psychiatric hospitals in North Carolina. At the time of this research, it had 398 beds and served a 25-county region with a 2012 total population of approximately 3.4 million (
7). Its ratio of 11.7 beds per 100,000 population placed it below the national average of 14.1 beds per 100,000 (
2). Most of the study hospital’s adult patients were male and self-pay or uninsured, had a diagnosis of severe mental illness, and were admitted under involuntary commitments (accounts receivable data on file). Community-based crisis services in the region included 494 adult psychiatric beds in 14 general hospitals or private psychiatric hospitals (19.1 beds per 100,000 population) and 66 nonhospital crisis beds in five facilities (2.6 beds per 100,000 population) (
7–
9).
These community-based services are the first tier of response for individuals in psychiatric crisis in the region, but they also serve as a major source of referrals to the state hospital. The study hospital provides a safety net when local inpatient capacity is exceeded and for patients whose illness is too acute or too difficult to manage in community-based settings. During the last six months of 2012, a mean±SD of 520±63 people waited in emergency departments across the state for admission to a state psychiatric hospital (
10). These people waited an average of 3.1±.3 days, although not all patients placed on waitlists were admitted.
At the time of this research, the study hospital’s clinical service units were organized into screening and admissions, medical, child and adolescent, adult acute (short-term), adult community transition (longer-term rehabilitative), and geriatric services. The study reported here focused on patients served in the adult acute and community transition units, because this subpopulation constituted the majority of the monthly waitlist. Each of these units contained male- and female-specific subunits, as well as a high-management subunit for patients requiring more intensive services or increased supervision.
Stakeholder Engagement
We held nine mental health system stakeholder meetings between October 2008 and February 2012 to communicate the study team’s goals and elicit written and unwritten “rules” governing how people flowed through the hospital. The number of attendees ranged from four to 30. The first four meetings were held with stakeholders from the hospital and from two of the hospital’s local community service areas, including representatives from local mental health agencies, psychiatric crisis care and outpatient care providers, community general hospitals, and law enforcement, all of whom were affected by delays in state psychiatric hospital admission. The last five meetings were held with the hospital’s clinical management staff, with three of the last five meetings also including executives from local mental health agencies. These later meetings were conducted to gain specific information about hospital unit capacities and the flow of patients through the hospital, as well as to seek feedback on preliminary findings.
Hospital administrators indicated that the total number of staffed beds was fixed at 398, but overtime and temporary staffing could be used to accommodate fluctuations in patient case-mix severity. Our research team initially considered cost-neutral scenarios that involved shifting beds between treatment units to explore efficiencies. However, preliminary simulation results indicated that most units were already operating at or near full capacity and that substantially decreasing wait times through supply-side interventions would require increasing bed capacity. Increasing staffed-bed capacity was potentially feasible at the study hospital, because 15% of its licensed beds were not in use at the time of this research. Therefore, our hypothetical scenarios focused on how many additional beds would be needed to reduce wait times by targeted amounts.
Data
We built the simulation model using North Carolina’s Healthcare Enterprise Accounts Receivable Tracking System (HEARTS), state psychiatric hospital waitlist data, information shared at mental health system stakeholder meetings, and personal communications with hospital stakeholders. HEARTS is an administrative claims database and billing system maintained for all visits to the state’s psychiatric hospitals. We used admissions data for all adult acute and community transition unit admissions between July 1, 2010, and July 31, 2012, to determine rates of patient arrivals and gain insights about the rules of patient flow through the hospital. We also used state psychiatric hospital waitlist data to confirm that the baseline model results were consistent with available data.
Simulation Model
Discrete-event simulations (
6,
11) model the operation of a system, such as a hospital, as a sequence of separate events in time (for example, patient admissions, treatment unit transfers, and discharges). In this study, these events changed two system states: the number of patients on the waitlist (a whole number) and treatment bed capacity (full or not). The random variables that needed to be characterized to model this system stochastically were patient waitlist arrival times and treatment unit length of stay.
Our baseline discrete-event simulation model captured the flow of patients through the state psychiatric hospital during fiscal year 2012 (July 1, 2011, through June 30, 2012). We began with a simple model based on preliminary conversations with stakeholders, iteratively incorporating additional factors suggested by stakeholders to approximate the true complexity of patient flows. All scenarios started with an empty hospital, using a one-year warm-up period to allow the simulated hospital and waitlist to reach realistic census levels. The model was built using ProModel, version 8.6 (
12). The main components and operationalizations are described below. [Additional technical details of the simulation modeling are included in an
online supplement to this article and can be obtained from the first author.]
Patients
The model included patients ages 18–64 (the only patients eligible for care in the units being studied). These patients were randomly selected, with replacement from a pool of actual patient admissions to the hospital during fiscal year 2012, thus reflecting actual patient population diversity in age, sex, and diagnoses. Several additional attributes were assigned to patients in the model on the basis of HEARTS data, including length of stay (estimated using a Cox proportional hazards model) and eligibility for the high-management and community transition units.
Patient Arrivals and Processing
We modeled patient arrivals to reflect all patients who entered the waitlist, regardless of whether they were ultimately admitted, by increasing observed hospital admission rates by a factor of 1 divided by the mean probability of admission (.38, from waitlist data). In practice, we were told, certain patients may be prioritized for admission from the waitlist for acuity and management concerns. However, stakeholders indicated that these patients could not be identified from the utilization data available to us; thus, in our simulations, hospital admission rates were increased uniformly for all patients.
Hospital clinicians and managers noted that upon referral, if an appropriate adult acute unit bed was available, the patient was admitted to that bed. Otherwise, the patient was placed on the waitlist and retained at the referral source until a bed at the hospital became available. When a regular adult acute unit bed for a male or female became available, a patient was admitted from the male or female waitlist on a first-in, first-out basis. We used person-level waitlist data from one local service area between January 1 and June 30, 2010, to estimate the amount of time people waited before they were admitted to the state hospital, found care elsewhere, or no longer needed inpatient care.
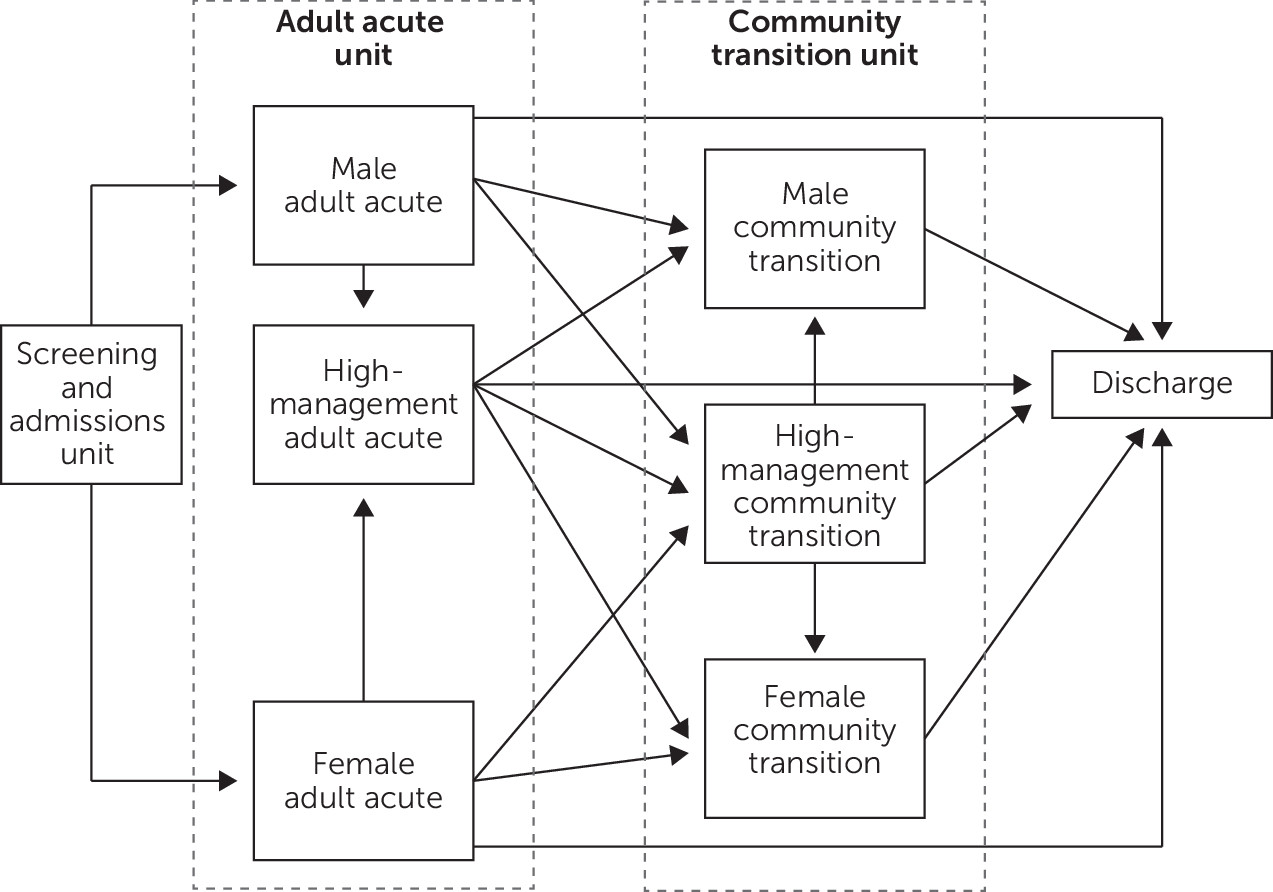
According to clinical managers at the study hospital, admitted patients followed a number of different pathways through the hospital. Specific rules were elicited to describe how and when patients flowed between units. These rules varied by patient sex, eligibility for high-management and community transition units, and availability of beds. The rules were translated into the care pathways outlined in
Figure 1.
Treatment Units
Figure 1 depicts the two main treatment locations included in the model: the adult acute unit and the community transition unit. To account for fluctuations in staffed beds, we used HEARTS data to determine the daily average number of beds in use in each unit during the year. In the adult acute unit, we modeled 86 beds designated for men, 44 beds for women, and ten high-management beds for use by either men or women. Similarly, in the community transition unit, we modeled 44 beds for men, 22 for women, and ten high-management beds.
Base Case and Hypothetical Scenarios
We took several steps to verify that the model behaved as intended. For example, we examined the model’s behavior with only one patient arriving and varied the patient attributes to confirm that the patient’s pathway through the hospital was consistent with the pathways depicted in
Figure 1 and with the associated rules. Similarly, we varied length-of-stay estimates and probabilities of high-management and community transition unit eligibility to ensure that the model reacted as expected. The first two authors independently reviewed the model’s code and conducted independent scenario analyses. Finally, technical consultants from ProModel verified our simulation model and improved its computational efficiency.
After verifying the model’s structure, we compared baseline simulated patient flow to fiscal year 2012 HEARTS data. We adjusted rules of patient flow so that the simulated outcomes better reflected actual patterns of hospital use (for example, matching the annual expected number of community transition unit discharges). Model results related to patient queuing and unit utilization were also compared with waitlist data and stakeholder input. We used four hypothetical scenarios to simulate alternative capacity expansion targets. In the first expansion scenario, we added 24 beds, distributed equally across the four regular treatment units. In each of the other three scenarios, we repeatedly added a bed to the treatment unit with the highest utilization rate (that is, the bottleneck unit) until a wait time threshold (three, two, or one days) was reached.
The study was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill.
Discussion
Results of supply-side simulations at our study hospital indicated that a large number of additional state hospital beds would be needed to make any substantial impact on the average wait time to admission of people in crisis. Furthermore, reducing average wait time below one day would require nearly a 165% increase in bed capacity at the study hospital. Although recent legislative proposals in North Carolina have called for the construction of a fourth state psychiatric hospital to increase systemwide capacity (
15,
16), authorizing legislation has yet to be enacted.
All the expansion scenarios considered in this research were based on steady-state assumptions that kept constant both the level of community demand for inpatient psychiatric treatment and the supply of alternative psychiatric beds in community general hospitals and freestanding crisis facilities in the region served by our study hospital. However, bed capacity increases could be made in these community facilities instead of, or as well as, in the state hospital. Expanding community-based intensive outpatient services, such as assertive community treatment, would also help to reduce the need for state psychiatric hospitalizations (
17). In other words, a more comprehensive resource optimization model could be constructed to consider demand-side as well as supply-side interventions.
To a limited extent, North Carolina has already increased the availability of general hospital psychiatric inpatient beds for uninsured patients through its three-way contract beds initiative, which provides short-term psychiatric crisis services and detoxification in community hospitals (
18). To the extent that such inpatient resources are able to serve patients who otherwise would have been cared for in a state psychiatric hospital, increases in community treatment capacity could achieve reductions in wait time similar to those described in our study hospital expansion scenarios. However, many community facilities are not currently staffed to care for the most acutely ill psychiatric patients and those who become violent. Thus, although buying community hospital beds may initially be less costly than adding state hospital beds, making community beds the sole solution would change community hospital staffing requirements, possibly increasing total costs for North Carolina.
Some other study limitations should be noted. For example, the scenarios we examined were limited to our study hospital, and we may have applied unrealistic assumptions or simulation parameters. However, we sought to ensure accurate model input by relying on utilization data to the extent possible and by involving system stakeholders throughout the model-building process. Also, the simulation model could be adapted to other state psychiatric hospitals in North Carolina and elsewhere in the United States.
Under current policy and financing arrangements, state psychiatric hospitals remain a vital component of the U.S. mental health system, offering treatment for people whose illness severity or violence exceeds the capacity of community providers. Demand for psychiatric hospital beds is increasing (
19). At the same time, financially pressed states continue to reduce state hospital capacity (
20), in part because of federal regulations precluding Medicaid reimbursement for nongeriatric adults in institutions for mental disease (
21). This study highlights an example of the national disconnect between increasing demand for psychiatric inpatient care and decreasing supply.