The rate of psychiatric disorders among youths in correctional facilities is believed to be significantly higher than the rate among youths in the general population. The prevalence of psychiatric disorders among youths in correctional facilities has been estimated as upward of 5% for psychotic disorders, 29% for major depression, 55% for anxiety disorders, and 86% for substance use disorders (
1–
3). Yet it is estimated that only one-quarter to one-third of incarcerated youths requiring mental health services actually receive them (
4).
There are few population-based and representative data on both needs and service use among incarcerated youths and young adults (
1). Specifically, very little is known about the treatment of incarcerated youths with mental health conditions during and after correctional entry. Estimating use of mental health services in the correctional system is an important measure of the need for services in highly vulnerable incarcerated populations. Measuring whether youths with mental illness receive their first mental health treatment in correctional facilities may be an indicator of poor access to hospital- and community-based health services. Information about prior treatment may be particularly crucial for incarcerated youths with more severe illnesses, including schizophrenia and bipolar disorder (
4,
5); for these youths, correctional involvement may be a sign of missed opportunities to access preventive mental health services and avoid involvement in criminal activity secondary to psychiatric decompensation (
6). A previous study found that 30% of adults who used mental health services while incarcerated had no contact with mental health services in the three years prior to incarceration (
7); however, the extent to which youths and young adults are first-time recipients of mental health care in correctional centers is unknown.
The objectives of this population-based study were to describe the sociodemographic and diagnostic characteristics of young people who used mental health services while in correctional custody and to determine whether the services represented the first time they had received mental health treatment. First use of mental health services while in correctional custody was determined by quantifying contacts with mental health services before correctional custody.
Methods
This population-based study included individuals ages 12–24 who received mental health treatment from a physician while incarcerated in correctional facilities in Ontario, Canada, during the correctional study period (April 1, 2010–March 31, 2012). In Canada, provincial correctional facilities house inmates who are awaiting sentencing and all inmates serving sentences of two years less a day. Our study population included youth offenders as defined by the Canadian Youth Justice Act (ages 12–17) and young adult offenders, whom we define as individuals ages 18–24. Youth offenders may be housed in either youth detention centers or adult correctional centers on the basis of their offense. All provincial youth and adult correctional facilities were included in this study.
Ethics approval was given through the Sunnybrook Health Sciences Centre Research Ethics Board in Toronto, Ontario. Data were analyzed using linked population-based health administrative databases at the Institute for Clinical Evaluative Sciences (ICES). Ontario residents have universal insurance through the Ontario Health Insurance Plan (OHIP) for all medically necessary health services. On the basis of their OHIP number, residents are assigned a unique, encoded ICES identifier that is used to link their health and demographic records across ICES databases at the individual level.
In the absence of access to inmate administrative databases, we used physician claims, which are captured in the OHIP claims database, to define the population of youth and young adult offenders in corrections, assuming that most offenders are assessed by an OHIP-funded physician at least once while incarcerated. From this group, we defined our “primary” study population, individuals who had at least one mental health–specific physician visit during the correctional study period. The assumption that most offenders are assessed by an OHIP-funded physician is likely more accurate for young adult offenders than for youth offenders, who may be more likely to receive mental health services from clinicians who do not bill OHIP. As such, our estimates of the youth offender population and their use of mental health services during the correctional study period are likely low.
Use of mental health services before the earliest OHIP claim during the correctional study period, including hospitalizations and emergency department visits, was obtained from the Discharge Abstract Database of the Canadian Institute for Health Information (CIHI), the Ontario Mental Health Reporting System database, and the CIHI National Ambulatory Care Reporting System (CIHI NACRS) database. Additional demographic information, including age, sex, and urban or rural residence prior to custody, were obtained using data compiled by Statistics Canada and housed at ICES.
To determine whether individuals received their first mental health treatment while incarcerated, we examined mental health service use prior to correctional custody. Individuals in our primary study population were deemed first-time correctional center patients (the “secondary” population) if they had no physician visits in a correctional facility prior to the correctional study period; the date of their earliest OHIP claim during the correctional study period served as a proxy “index” date for the beginning of their correctional episode. [A figure illustrating the procedure for identifying the study population is available in an online supplement to this report.] This highly specific method allowed us to ensure that any use of mental health services before the index date occurred prior to any evidence of an individual’s having been in the correctional system and was therefore our best estimate of mental health services use before the beginning of the correctional episode.
Mental health–related physician visits for the primary study population were defined by using diagnostic, procedure, and physician specialty codes in OHIP records (see
online supplement for details about how physician visits were defined). Our definition of mental health–related primary care has previously been validated by chart review (
8). The primary study population was further categorized by psychiatric diagnosis in order to assess differences in demographic characteristics and use of mental health services among individuals with more versus less severe mental illness. The population was classified by the following hierarchical, mutually exclusive primary diagnostic categories: schizophrenia, mood disorders, substance use disorders, anxiety disorders, and other. These primary diagnostic categories were also used when examining use of mental health services before the beginning of the correctional episode in the secondary population.
Mental health treatment before the beginning of the correctional episode in the secondary population was defined as any mental health–related physician visit, emergency department visit, or hospitalization that occurred one year and five years prior to an individual’s index date during the correctional study period [see online supplement for the diagnostic codes used to identify mental health–related emergency department visits and hospitalizations].
SAS statistical software, version 9.3, was used to generate prevalence estimates for all demographic and diagnostic variables in the primary study population. Prevalence estimates were also generated for use of mental health services before the beginning of the correctional episode, both overall and for each of the diagnostic groups defined above.
Results
A total of 13,919 youths and young adults were identified in the correctional system through OHIP claims during the correctional study period; 42% (N=5,823) had a mental health visit during the correctional study period and comprised our primary study population. Youths and young adults with a physician visit for mental health services during the study period tended to be older and were more likely to be male and from lower-income and urban areas. However, the proportion of youths with a mental health visit during the correctional study period was higher among youths from rural areas (N=755 of 1,318; 57.3%) compared with all 13,919 youths with OHIP claims (N=1,318, 9.5%). [Details about the demographic characteristics of the study population are available in the online supplement.]
In the primary study population, more than 20% of youths and young adults were classified in the most severe diagnostic categories (schizophrenia, N=507, 9%, and mood disorders, N=729, 12%). The largest diagnostic group was the anxiety disorder group (N=2,856, 49%). In all diagnostic groups, the majority of youths were male and belonged to the older age group. However, the substance use disorders group (N=1,225) had a relatively high proportion of females (N=279, 23%). [Details about the demographic characteristics of the primary study population by diagnostic category are available in the online supplement.]
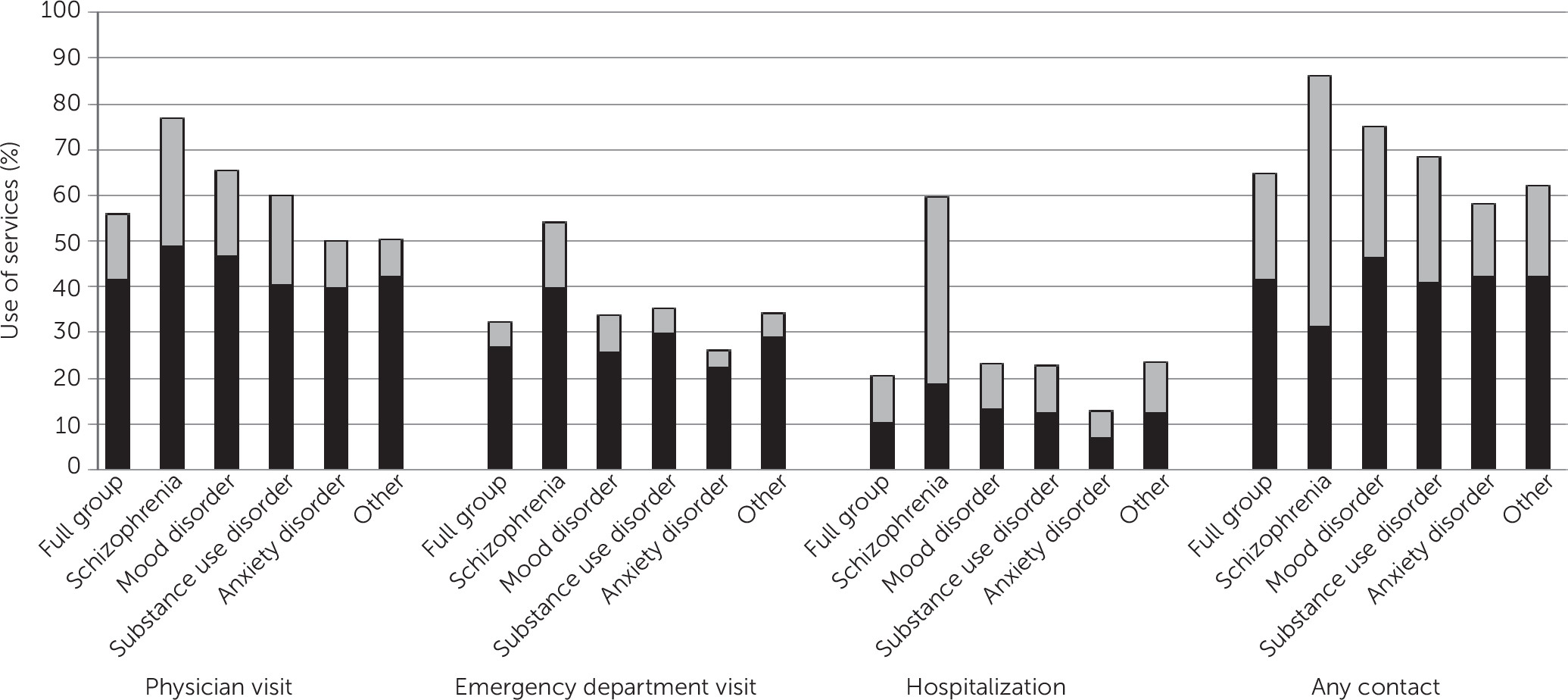
Fifty percent of our primary study population had no prior OHIP health encounters in a correctional center and, therefore, were defined as the first-time correctional center patient cohort, our secondary study population (N=2,913). Of this population, 65% (N=1,883) had mental health treatment in the five years prior to correctional custody, but only 23% (N=668) had mental health treatment in the year prior to custody (
Figure 1). Physician visits were generally the most common type of mental health contact for each diagnostic group. The schizophrenia group (N=207) had the highest rates of mental health treatment before the beginning of the correctional episode, particularly mental health–related hospitalizations; 60% (N=123) and 40% (N=84) of the group was hospitalized in the five years and one year prior to correctional custody, respectively.
Discussion
To our knowledge, this was the first population-based study to utilize routinely collected health administrative data to assess use of mental health services in a population of younger offenders both during and prior to correctional custody. We found that a high proportion of the young correctional population of Ontario had used physician-based mental health services while in custody. Notably, schizophrenia prevalence in the young correctional population as a whole, according to service use patterns, was notably high (4%), compared with estimates of schizophrenia prevalence in the general population (<1%) (
9). Service use is very likely an underestimate of true mental illness prevalence and need in correctional facilities, given that many incarcerated young people with severe mental illnesses may not seek mental health care. Rates of severe mental disorders may indeed be higher in the young correctional population.
Thirty-five percent of youths and young adults with mental health treatment during the correctional study period had no mental health contact during the five years prior to entering the correctional system. This estimate is similar to the results of a previous study that estimated use of mental health services before incarceration among adults who used mental health services in correctional facilities (
7). Although some psychiatric symptoms may arise after incarceration, studies assessing mental health or addiction issues at correctional facility intake have reported high levels of preexisting mental health conditions (
10,
11). If the same holds true for our population, the incarcerated youths with no prior mental health service use either did not seek or had difficulties gaining access to physicians who could provide mental health services and support prior to correctional involvement.
The youths and young adults who used mental health services before the beginning of the correctional episode tended to have more severe conditions, particularly schizophrenia. The notably high proportion of individuals with schizophrenia who were hospitalized in the year prior to entering the correctional system (40%) could be indicative of poor continuity of care after discharge from the hospital, when this population may be at risk of encounters with the criminal justice system (
5).
This study had a number of limitations. Given that we could not access correctional administrative data, we assumed that the majority of inmates had at least one physician visit while in the correctional system and used OHIP claims to create a denominator population of incarcerated young people. However, it is possible that this method biased the study population by excluding individuals who had shorter incarceration periods and, therefore, less time or opportunity to seek medical services. We also could not capture individuals who received nonphysician mental health services, which may have further underestimated prevalence, particularly for the youth offender group. Because we did not have access to correctional entry and exit dates, we used physician claims to make assumptions about the timing of mental health treatment before the beginning of the correctional episode. However, in the absence of other data, this was the best way to approximate first mental health contact in the correctional population. In summary, our limitations likely underestimated mental health service utilization among the youth offender population in Ontario.
Conclusions
This study demonstrated the high mental health needs of youths and young adults in correctional custody. Examination of use of mental health services prior to correctional custody indicated that a significant proportion of young people with mental health issues may be accessing treatment for the first time while in custody, whereas those with schizophrenia or other severe mental illness may end up in the correctional system despite high rates of prior ambulatory and hospital-based care. Nevertheless, gaps in the justice system and the health care system, of which there are many, can also be seen as opportunities to coordinate services and assessments in order to provide rehabilitative options for young people in custody with both moderate and severe mental illnesses.