Population research has consistently shown increased mortality among persons with severe mental illness (
1–
8). After widespread deinstitutionalization (
9), compulsory supervision outside a hospital has been developed internationally for the treatment of persons with mental illness. Outpatient commitment seeks to provide protection and care via compulsory supervision for people with severe mental illness (
10,
11). This study investigated the relationship between the use of outpatient commitment in Victoria, Australia, which operates by means of community treatment orders (CTOs), and risk of mortality experienced by individuals hospitalized for psychiatric reasons. [A description of CTO use in Victoria is included in an
online supplement to this article.]
In 2000, Victoria closed its last psychiatric hospital and moved to provide integrated health care centered around its general hospitals. In this new era, some have pointed to an increase in the number of CTOs issued as an indication of overreliance on involuntary community treatment (
12,
13). An alternative view is that the increase in CTOs represents clinicians’ assessments that briefer hospitalizations and early release from an inpatient episode place patients at increased risk of adverse outcomes (
14), one of which is increased mortality without the care provided in a psychiatric hospital. In this view, CTOs are the least restrictive alternative to a psychiatric hospitalization. Indeed, supervision provided under CTOs between 1990 and 2000 in Victoria (
15) and elsewhere (
16) has been found to be associated with reduced mortality risk. However, the reasons for this association remain unclear, as do the effects of CTO placement on individuals’ quality of life (
17).
Given the changes in Victoria’s health system, this study addressed the following questions: Did being placed on a CTO between 2000 and 2010 continue to be associated with reduced mortality risk? If so, can reduced mortality risk be attributed to CTO-facilitated access to acute medical care or to the potential of CTOs to reduce involvement in crimes against persons? If CTO placement continued to be associated with reduced mortality risk in 2000–2010 (
15), are the years of life saved associated with a poorer quality of life (
17,
18)?
Methods
Samples
Mental health records from the state of Victoria, Australia, for 2000 to 2010 were obtained from the Victorian Psychiatric Case Register/RAPID (VPCR/RAPID) system for 27,535 patients who experienced psychiatric hospitalization during the period. A total of 11,424 were first placed on a CTO during this period (2000–2010), and 16,161 were hospitalized but never placed on a CTO. The VPCR/RAPID system provides details on all clinical mental health contacts occurring in Victoria. The records were matched with the Australian National Death Index, a compilation of all deaths throughout Australia, during the index study period of July 1, 2000, to February 28, 2012. These combined records were linked to the Victoria Police Law Enforcement Assistance Program (LEAP) data (
19), which document all police contacts in Victoria associated with perpetration of and victimization by major crimes against persons; the Victorian Emergency Minimum Data set, which consists of clinical episode data from emergency departments of Victorian public hospitals; the Victorian Admitted Episodes Data set, which consists of clinical episode data for admitted episodes of care in Victorian general medical hospitals; and the National Outcomes and Casemix Collection, which includes clinical quality-of-life assessments of patients that are conducted with the Health of the Nation Outcome Scales (HoNOS).
Measurement
The structuring of the data for analysis and the content of each of the data sets are reported in a companion article (
14). Briefly, all treatment contacts were organized into inpatient and outpatient episodes of care. Occasions of community service are reported as community treatment days, and intensity of service provision was measured by treatment days per community care episode (
14). Access to acute general medical care was measured by receipt of at least one
ICD-10 or AR-DRG (Australian Refined Diagnosis-Related Groups) diagnosis of a major general medical illness in a hospital or emergency department. Perpetration and victimization were documented by reports of major crimes against persons in the Victoria Police LEAP system reports.
In multivariate modeling, Socio-Economic Indexes for Areas (SEIFA) (
20) postal code ranks for Victoria provided a measure of social disadvantage (lower scores indicate more disadvantage). The individual’s most disadvantaged area of residence was taken into account to control for inherent social inequalities in life expectancy attributable to residence in a poverty area.
The problem of selection associated with comparing cohorts was addressed with preliminary matching on age, sex, and diagnosis in drawing the sample, propensity score control in the study models, and statistical adjustment for potential confounding variables in these models. The propensity score used in the models was based on service, social, and premorbid characteristics that distinguished patients placed on CTOs from other patients in the Victorian mental health system who were not placed on CTOs [see online supplement for additional details].
Quality of life was measured with profiles of the 12 HoNOS items (
21): aggression, nonaccidental self-injury, drug or alcohol problems, cognitive problems, general medical illness or disability, hallucinations or delusions, depressed mood, other mental or behavioral problems, relationships, activities of daily living, living conditions, and occupation and activities (
14). HoNOS items were independently scored (
22) at various stages in a person’s involvement with mental health services; scoring was by clinicians not associated with the patient’s care. The average of all HoNOS assessments made for each patient during the periods associated with years of life saved for men and women separately was taken as the measure of each patient’s quality of life.
Analyses
All analyses were completed with SPSS version 23 (
23) and Excel 2016 spreadsheet software (
24). Excel was used for computing standardized mortality ratios (SMRs), years of life lost (YLL), and relative risk (RR) statistics (
25). SMR comparisons were based on deaths in the Victorian population and reported by age and gender (
26). RR and YLL statistics among patients in the CTO and non-CTO cohorts were computed by using life table analyses. The analyses compared the expected age- and gender-adjusted mortality of those in the CTO cohort with their expected mortality, assuming that the CTO group had the same age and gender distribution as the non-CTO patients; SMRs and YLL were used to compare life expectancy at birth of the average-age sample member at midstudy. The YLL was computed separately for men and women. The index year was 1971, when a man’s life expectancy in Victoria was 68.7 years and a woman’s was 75.2 years.
The contributions of CTOs to mortality risk and the role of access to general medical care and of crime and victimization involvement in interaction with CTO exposure were assessed with logistic regressions. Significant interactions were evaluated on the basis of the model statistics. The logistic models analyzed the contribution of a CTO to non–injury-related mortality risk and death from injury (that is,
ICD-10 codes including accidents, homicide, suicide, and other unexplained causes of death [
27]). The models were adjusted for treatment days per community care episode (that is, how much supervision was actually provided); gender; age; age at entry into the mental health system; diagnoses (schizophrenia, major affective disorders, paranoia and other psychoses, and dementia); total number of inpatient days (a control for the protective character of hospitalization in a patient’s treatment); time in the study (risk period); potential stereotype and communication effects (non-English speaker and Aboriginal or Torres Strait Islander status); propensity to be selected into the CTO cohort; the patient’s psychosocial profile reflected in his or her 12 HoNOS scores at both inpatient admission and release; and, given findings of an association between community context and death (
28), the lowest SEIFA postal code rank of a neighborhood in which the individual resided (
20).
Implications for patient quality of life were determined by using analysis of variance to evaluate differences in the mean scores on the 12 HoNOS items over the periods of life saved, according to YLL statistics for males and females separately.
Ethics
Ethics committees of the Department of Health and Human Services of Victoria, the Australian Institute of Health and Welfare, the Australian National Death Index, the National Coronal Registry, the Victoria Police, and the Human Subjects Committee of the University of California, Berkeley, approved the human subjects procedures for the project. The project was compliant with data regulations set by all approving agencies and their ethics committees; no data breaches or other adverse events occurred during the study.
Results
Sample Characteristics
The mean±SD age of the overall sample of hospitalized patients (N=27,585) was 34.0±16.7 years at the study outset. In the overall sample, 15,480 (56%) were men and 12,103 (44%) were women, and two were of unknown gender. Compared with the non-CTO cohort, the CTO cohort had proportionally more men (58%, N=6,646, versus 55%, N=8,834) and was approximately three years younger (32.4±15.3 versus 35.4±17.5). The diagnostic, social, and service characteristics of the samples are reported in the companion article (
14).
Mortality
The crude cumulative death rate per 1,000 for Victoria’s population over the 11.8-year period (July 1, 2000, to February 28, 2012) was 77.85. For the overall sample of hospitalized patients, it was 98.93—90.16 for the CTO cohort and 105.10 for the non-CTO cohort (
Table 1). During the study period, the death rate in the CTO cohort was 1.27 times the rate in the general population, and the death rate in the non-CTO cohort was 1.35 times the general population rate. For the CTO cohort, the risk of death was lower than for the non-CTO cohort (RR=.86). On the basis of the age- and gender-specific death rates for the state of Victoria, the SMRs were 1.17 for patients in the CTO cohort (1.14 for men and 1.22 for women) and 1.36 for patients in the non-CTO cohort (1.36 for men and 1.37 for women).
During the 11.8-year study period, there were 2,727 deaths (10% of the overall sample). The CTO cohort accounted for 38% of these deaths (N=1,030), and the non-CTO cohort accounted for 62% (N=1,697, or N=1,695 where information on the gender of the decedent was available). The expected number of deaths in the CTO cohort was 879, indicating an excess of 151 deaths—or 12.8 excess deaths per year. In the CTO cohort, the number of excess deaths over the 11.8-year period was 72 among men and 79 among women. In the non-CTO cohort, the expected number of deaths was 1,243, indicating an excess of 452, or 38.3 excess deaths per year. In the non-CTO cohort, the number of excess deaths was 249 for men and 203 for women.
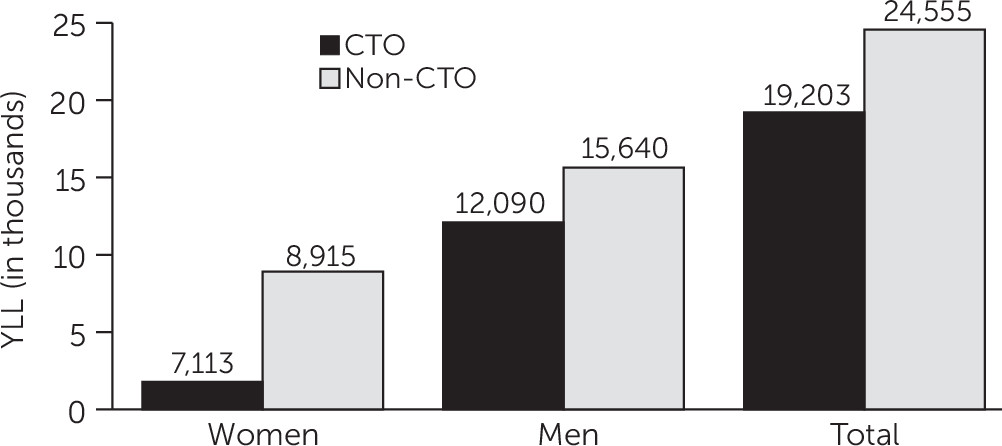
Figure 1 shows YLL for men and women in both cohorts. The non-CTO cohort lost 5,352 more years of expected life, compared with the CTO cohort. The 938 men who died in the non-CTO cohort lost 3,550 more years of life than the 590 men who died in the CTO cohort—or, on average, 3.8 more YLL per individual in the non-CTO cohort. The 757 women in the non-CTO cohort who died lost 1,802 more years of life than the 440 women who died in the CTO cohort—or, on average, 2.4 more YLL per individual in the non-CTO cohort.
CTO Exposure and Mortality Risk
The logistic regression models, which included the control factors noted above, were all significant (p<.001) (
Table 2). Results indicated that the CTO cohort experienced a 9% reduction in overall mortality risk, compared with the non-CTO cohort. Overall risk has two components: one for external causes and one for other causes. The 9% is the net effect of the 17% (Exp(b)=.83) reduced mortality risk in deaths by other causes (that is, exclusive of the external causes attributable to assault, self-harm, and undetermined intent) and an elevated risk of 26% (Exp(b)=1.26) associated with external causes, assault, self-harm, and undetermined intent. Furthermore, the elevated risk associated with external causes in the CTO cohort seemed to be primarily explained by a 32% (Exp(b)=1.32) increased risk of death from self-harm.
The models were rerun to assess the impact of greater access to general medical care facilitated by CTO oversight and of crime and victimization prevention resulting from CTO involvement (data not shown). When death exclusive of assault, self-harm, and undetermined intent was the criterion variable, access to medical care had a significant interaction with CTO status. The model was significant (χ2=5,049.24, df=46 and 27,129, p<.001; correct classification=93.3%). The interaction term indicated that among patients on CTOs, which facilitated access to medical care, the risk of death (exclusive of assault, self-harm, and undetermined intent) was 20% less (Exp(b)= .80, 95% confidence interval=.68–.95). These results remained the same when the analysis took into account all the potential confounding factors listed above [see online supplement].
The model assessing the impact of CTO involvement on risk of death from prevention of crime and victimization was also significant (χ2=306.88, df=46 and 27,129, p<.001; correct classification=98.3%), although the interaction term testing this hypothesis was not.
Quality-of-Life Outcomes
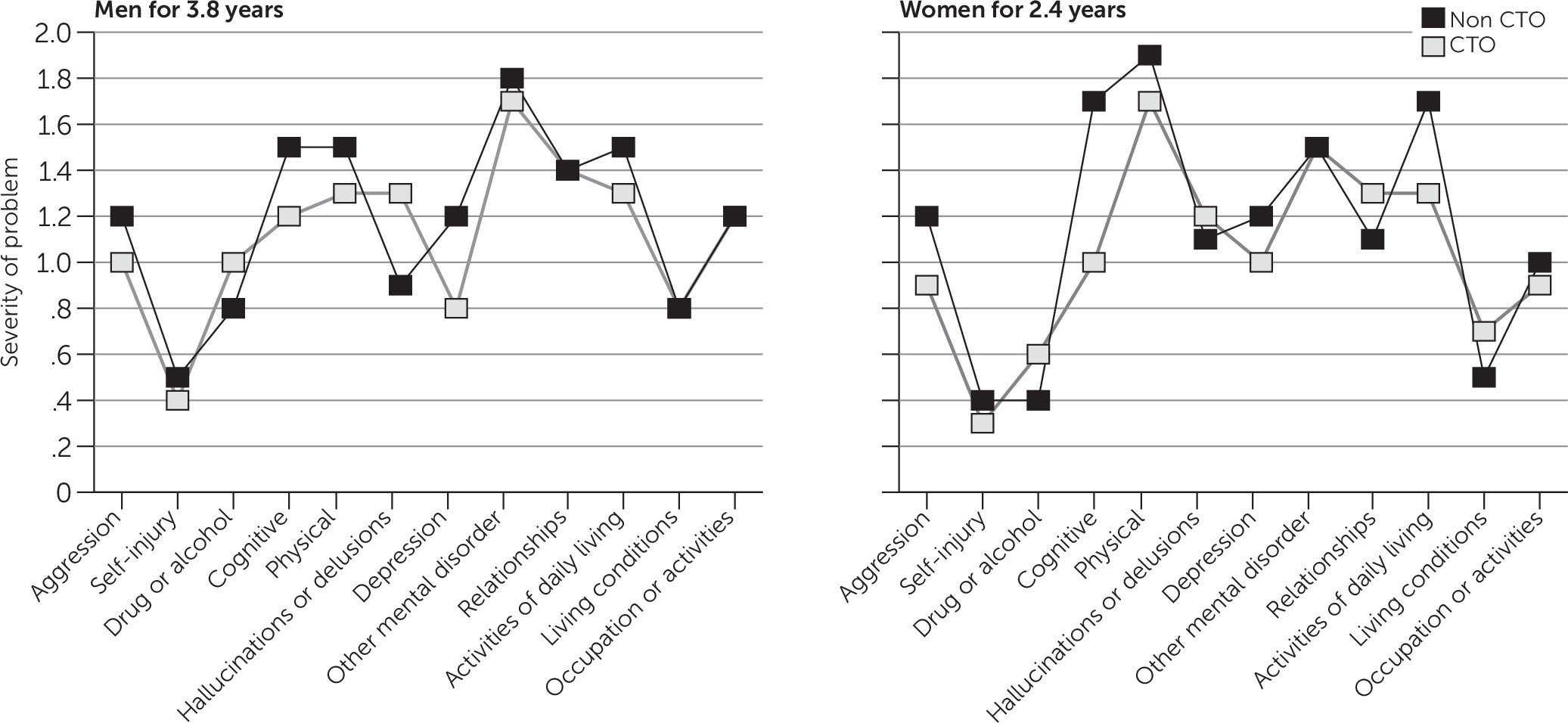
As noted above, CTO placement appeared to lead to a gain of 3.8 years of life among men and 2.4 years among women.
Figure 2 presents mean scores on the 12 HoNOS items during the final 3.8 years of life for all men who died and the final 2.4 years for all women who died. Men in the CTO cohort who died and for whom HoNOS assessments were available for the final 3.8 years of life (N=343) had significantly higher scores than their non-CTO counterparts (N=344) on drug or alcohol problems (p=.025) and hallucinations or delusions (p<.001). In the non-CTO cohort, however, these men had higher scores on problems associated with self-injury (p=.042), cognitive functioning (p<.001), physical health (p<.001), depression (p<.001), and activities of daily living (p=.011). The two groups of men did not differ significantly on assessments of aggression, other mental disorders, relationships, living conditions, and occupation or activities.
Women in the CTO cohort who died and for whom HoNOS assessments were available for the final 2.4 years (N=207) had significantly higher scores than their non-CTO counterparts (N=258) on drug or alcohol problems (p=.004), relationships (p=.003), and living conditions (p=.010). Women in the non-CTO cohort scored higher on problems associated with aggression (p=.003), cognitive functioning (p<.001), physical health (p=.043), depression (p=.002), and activities of daily living (p<.001). The two groups of women did not differ significantly differ on problems associated with self-injury, hallucinations or delusions, other mental disorders, and occupation or activities.
Discussion
The analyses examined mortality among patients in Victoria, Australia, with mental disorders severe enough to require psychiatric hospitalization. As a group, these individuals were at increased risk of mortality compared with the population of Victoria. Protective supervision, such as that afforded by CTOs, seems to be of particular importance in Victoria and in other jurisdictions in which a reduced commitment to providing community-based services is evident (
14). The protective supervision offered to patients on CTOs, compared with patients not on CTOs, was found to be associated with reductions in excess deaths, with SMRs 14% lower in the CTO cohort. After the analysis controlled for multiple factors, the results indicated that the supervision afforded by CTOs contributed to a 9% reduction in overall risk of death and 17% reduction in risk of death exclusive of assault, self-harm, and undetermined intent. The reduction in overall risk occurred despite the CTO cohort’s 32% increased risk of death due to self-harm. These findings replicate mortality risk reduction outcomes associated with CTO supervision that were found in a similar analysis of data from the previous decade in Victoria (
15).
Findings demonstrated an association between CTO placement and facilitation of access to acute general medical care, which may partly explain how the mortality risk was reduced. Patients under CTO supervision, which facilitated access to acute medical care, were 20% less likely to experience a non–injury-related death (that is, exclusive of assault, self-harm, and undetermined intent).
Authors of some studies have concluded that CTOs are overused (
9,
12,
17). Persons who want to restrict the use of CTOs have raised two philosophical concerns about the type of findings reported here. First, although death rates are elevated among psychiatric patients, these persons question whether the rates are elevated enough to justify involuntary supervision. During the study period, patients in the CTO cohort died at a rate 1.27 times that of the general population. Comparative rates in the United States indicate that among individuals with severe mental illness who die, SMRs range from 1.2 to 4.9 times higher than in the general population (
29). Other studies have reported decreased death rates associated with CTO placement (
15,
16), and there also appears to be an association between reduced homicide rates and use of an outpatient commitment law with criteria similar to the law in Victoria (
30). These results and the results of this study suggest that a possible reason for the lower comparative death rate for persons with severe mental illness in Victoria is the availability of the CTO mechanism.
The second concern raised by those who want to restrict CTO use is that CTOs are an assault on quality of life (
17). However, our analysis of HoNOS quality-of-life ratings associated with years of life saved appeared to modestly favor the CTO cohort. Men in the CTO cohort scored significantly better than their non-CTO counterparts on five of the HoNOS dimensions, did not differ on five dimensions, and scored worse on two. Women in the CTO cohort also scored better than their non-CTO counterparts on five HoNOS dimensions, did not differ on four, and scored worse on three. It would seem that the years of life saved associated with CTO placement are not negatively affected by CTO placement.
The study had some limits. It was based on administrative data. Results did not reach the level of certainty of causal inference associated with randomized controlled trials. However, with the exception of one trial focused on victimization outcomes (
31), no trials have been completed that have a criterion focused on the need for treatment to protect health and safety. In today’s deinstitutionalized environment, the misplaced focus on reduction in hospitalization days may constitute a denial of needed treatment. Also, quality-of-life assessments were based on clinicians’ perspectives, although patients’ perspectives obtained via surveys evaluating the impact of outpatient commitment on quality of life have been mixed (
32).