One in eight U.S. women will receive a breast cancer diagnosis during her lifetime, and nearly 40,000 U.S. women die from breast cancer annually (
1). Prevention experts have recommended increased mammogram screening, which has been shown to reduce breast cancer mortality by up to 20% (
1–
4). Although breast cancer screening has improved substantially in recent years, underserved women (for example, women from racial-ethnic minority groups and uninsured women) remain less likely to receive guideline-recommended screening (
5,
6).
Disparities in breast cancer screening also extend to women with mental illness (
7). A recent meta-analysis of 24 studies that included a total of 715,705 women concluded that the rate of breast cancer screening among women with any mental illness was significantly lower than the rate among women without mental illness (odds ratio [OR]=.71, 95% confidence interval [CI]=.66–.77) and that women with severe mental illness were even less likely to obtain screening (OR=.54, CI=.45–.65) (
8). Among women with a diagnosis of breast cancer, those with schizophrenia have been shown to have a higher mortality rate compared with the general population (standardized mortality ratio=1.6, CI=1.5–1.7) (
9). A recent systematic literature review highlighted disparities in breast cancer screening among women with mental illness compared with the general population; however, the review found that studies were limited by small samples and the wide array of mental illnesses included (
7).
Although disparities in mammogram screening are well documented, to our knowledge no study has used a socioecological framework—the inclusion of individual, cultural, and systemic factors—to examine rates of breast cancer screening among a diverse population of women with severe mental illness. Socioecological frameworks have been used extensively to add the broader social context into models examining health behaviors (
10,
11), including screening such as mammogram utilization (
12). By using this approach to examine a large cohort of women with severe mental illness, patterns of mammogram utilization can be identified to help guide multilevel interventions. Although previous studies established that women with severe mental illness are less likely than those in the general population to receive breast cancer screening, much less is known about how other psychosocial factors, such as race-ethnicity, area of residence, and other factors related to health care access, are associated with breast cancer screening rates among women with severe mental illness.
Using a unique, large, integrated statewide data set of persons with severe mental illness who were receiving care in the public mental health system, we assessed mammogram screening rates among women receiving specialty mental health services in the state of California. The primary goals of this study were to extend the existing literature documenting mammogram disparities for those with severe mental illness by using a large, diverse data set and to examine the contribution of other psychosocial factors to mammogram utilization among women with severe mental illness. Because we included the social context of women with severe mental illness, our findings can be used to inform targeted efforts to improve breast cancer screening for subgroups of women with severe mental illness. Our primary hypothesis was that our cohort of women with severe mental illness would have lower breast cancer screening rates than women in the U.S. general population. We also hypothesized that within our cohort, rates of screening would be lower for those living in rural areas, those from racial-ethnic minority groups, those with more severe psychiatric illness, those with a comorbid substance use disorder, and those with no evidence of nonpsychiatric health care utilization.
Methods
Design, Databases, and Study Period
The study used a retrospective cohort design. Data were obtained from existing administrative, pharmacy, and billing systems of California Medicaid (Medi-Cal) and the Client and Service Information system, which collects client-level data from California’s county mental health programs. Approval was obtained from the Committee of Human Research of the University of California, San Francisco; the State of California Committee for the Protection of Human Subjects; and the Data and Research Committee of the California Department of Health Care Services (DHCS). The DHCS then combined the existing databases, deidentified the data, and provided us with the combined data set. Data were made available because we were helping the DHCS’s state public partners to examine the efficacy of a separate statewide quality improvement project. Because of the scope of the parent quality improvement project, data were limited to a one-year period from October 1, 2010, to September 30, 2011.
Study Population
The following inclusion criteria were used: Medi-Cal enrollee, female, age 48–67, specialty mental health care utilization during the study period, and a prescription claim for one or more antipsychotic medications during the study period. Although prescription claims for antipsychotic medications were not necessary inclusion criteria for this study, these claims were used to define the cohort for a parent study examining diabetes screening (
13). It is notable that in California and most states, specialty mental health care is reserved for people with severe mental illness. Individuals who were dually eligible for Medicare were excluded from our study cohort because we were unable to obtain Medicare breast cancer screening data.
Definition of Outcomes
The primary outcome measure was evidence of breast cancer screening via mammogram (CPT 77051, 77052, 77055, 77056, and 77057 or HCPCS G0202). Potential predictors of breast cancer screening included age; race-ethnicity; county of residence (rural versus urban); psychiatric diagnosis by mental health providers (for example, schizophrenia, bipolar disorder, major depressive disorder, anxiety disorder, or other axis I diagnosis) as defined by
DSM-IV-TR (
14), the criteria standard at the time of the study; a comorbid drug or alcohol use disorder as documented by mental health providers; and health care utilization defined as any nonpsychiatric health care utilization in the prior year (CPT 99201–99205, 99211–99215, and 99241–99245).
Screening Guidelines and Breast Cancer Screening Prevalence
Conflicting guidelines exist for breast cancer screening (
2,
3,
15–
18). However, the guidelines most likely to be used by providers caring for the women in this study population are those endorsed by the United States Preventive Services Task Force (USPSTF). The USPSTF guidelines at the time of the study recommended biennial mammogram screening for women ages 50–74 years (
19). Because our data captured only one year of screening information and the guidelines recommend screening every other year, we used a standard mathematical equation of
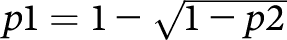
to estimate the annual rate (
p1
) derived from the biennial rate (
p2). Using this equation, we converted the 2010 biennial screening rate of 67% (
20), published by the Centers for Disease Control and Prevention, to an estimated annual screening rate of 43%.
Clustering at the Level of County
Because the State of California delegates mental health care policy and regulations primarily to the county level, analysis was clustered at the level of the county. Counties with few observations were grouped with counties of similar size, region, and demographic characteristics. This approach grouped Alpine with Inyo and Mono, Colusa with Glenn, and Lassen with Modec. All of these are rural counties (
21). San Mateo County was excluded because of much fewer observations in the database than we would have expected.
Data Analysis
We evaluated the associations of each predictor of interest with mammogram screening by using Poisson models with robust standard errors (
22). We used Poisson rather than logistic models because risk ratios are easier to interpret, particularly with relatively common outcomes, where the OR is a badly biased estimator of the risk ratio. For each predictor, we fit two Poisson models, the first unadjusted and the second adjusted for confounders identified by using directed acyclic graph (or causal graph) but excluding any mediators of its effects. [Additional details about these models are included in an
online supplement to this article.] The adjustment variables for each predictor are specified in the footnotes of
Table 1. In additional exploratory analysis, we estimated direct effects of race-ethnicity and rural residence not mediated by health care utilization.
Results
Table 1 summarizes data on demographic and other sociocultural factors (health care utilization and area of residence) for the cohort (N=14,651). The sample had significant racial-ethnic diversity: Asian/Pacific Islander, 17%; black, 19%; Hispanic, 14%; other, 12%; and white, 38%. Seventy percent of women were between the ages of 48 and 57, and the remaining 30% were ages 58 to 67. Only 3% of the sample was considered to be living in a rural area, and the other 97% lived in an urban area. There was a range of psychiatric diagnoses in the sample: schizophrenia spectrum illness, 43%; major depressive disorder, 33%; bipolar disorder, 14%; anxiety disorder, 4%; and other, 5%. Twelve percent of the sample had a documented history of a comorbid substance use disorder. Nearly one-quarter of the cohort (24%) had no evidence of nonpsychiatric health care utilization in the past year.
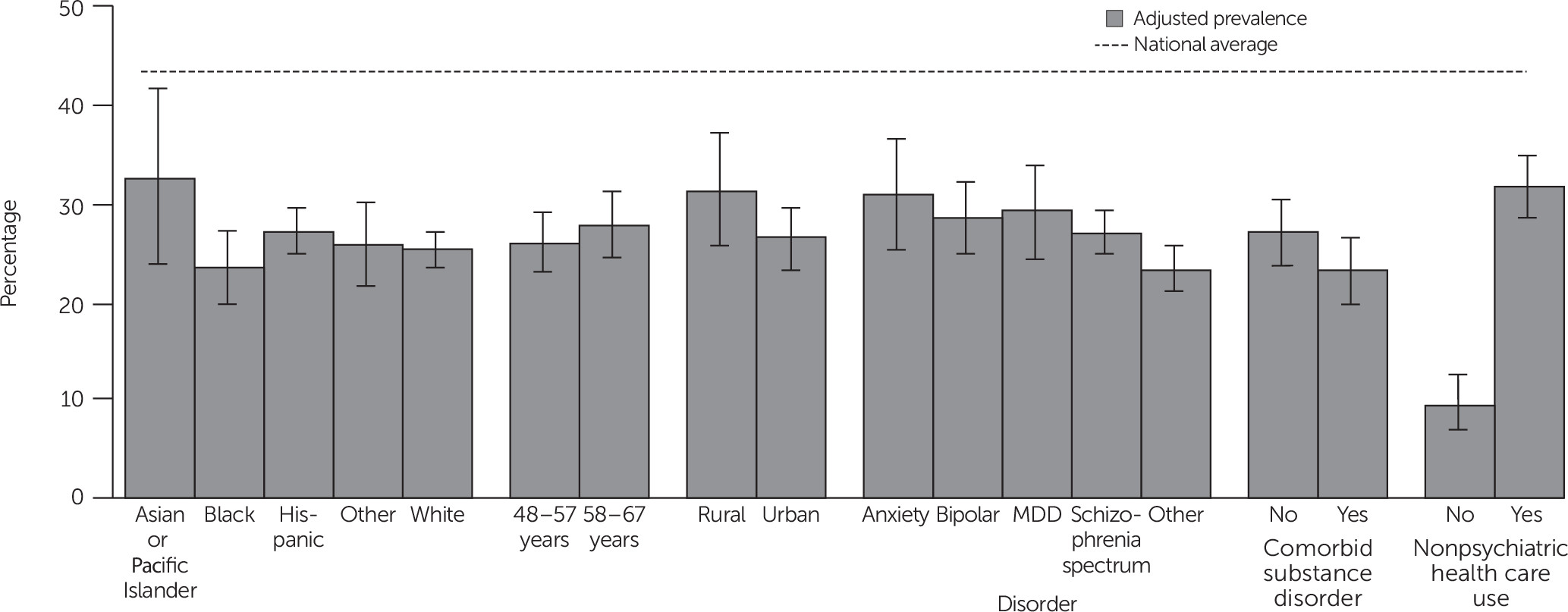
Within this large and diverse cohort of women with severe mental illness, 24.5% (3,589/14,651) received breast cancer screening with a mammogram in the past year, compared with an estimated annual screening rate of 43% among women in the U.S. general population. As shown in
Figure 1, regardless of demographic characteristics, psychiatric diagnosis, comorbid substance use disorder, or utilization of nonpsychiatric health care, the adjusted prevalence of mammogram screening among women in the study cohort fell far below the estimated annual rate in the general population.
Table 2 presents risk ratios for each predictor of interest, first unadjusted and then adjusted for predictor-specific confounders. In the adjusted analysis, the p value for race-ethnicity shows clear evidence for heterogeneity across groups, but there is no clear evidence that any one group differs from whites, who were used as the reference group. Neither age group (48–57 years versus 58–67 years) nor area of residence (rural versus urban) was associated with a difference in mammogram screening. Differences in mammogram screening rates varied by psychiatric diagnosis. Compared with women with schizophrenia spectrum disorder, those with anxiety disorder (ARR=1.33), bipolar disorder (ARR=1.22), major depressive disorder (ARR=1.25), and other diagnoses (ARR=1.16) were all more likely to have been screened in the past year (p<.001). A history of a comorbid alcohol or drug use disorder was associated with a lower likelihood of screening (ARR=.86). Finally, evidence of nonpsychiatric health care use was strongly associated with mammogram screening (ARR=3.30).
Evidence of nonpsychiatric health care use partially mediated the association of screening with Asian/Pacific Islander race-ethnicity. That is, Asian/Pacific Islander race-ethnicity was no longer significantly associated with mammogram screening after adjustment for nonpsychiatric health care use. In contrast, after adjustment for nonpsychiatric health care use, a direct effect of rural residence was noted (direct-effect ARR=1.45, CI=1.17–1.80, p=.007).
Discussion
Our study examining breast cancer screening rates among women with severe mental illness yielded several findings with potential public health and health policy implications. First, across all demographic and diagnostic categories, rates of breast cancer screening in our large sample of women with severe mental illness fell far below the average rate for women in the U.S. general population. This finding validates our original hypothesis and is consistent with other smaller studies in which breast cancer screening was found to be another example of a health care disparity for people with severe mental illness in the United States (
7,
8,
23,
24). Effectively closing this disparity gap will require individual, clinical, and systemic changes, including both increased outreach to women with severe mental illness and increased communication between mental health and primary care providers (
25).
Because our data source was limited to women with severe mental illness who used mental health services and filled at least one prescription for an antipsychotic medication in the past year, women not meeting these criteria were not included in the cohort. The excluded women may have been even more severely ill (for example, those not accessing services and not filling prescriptions) and may have been less likely to have received preventive services, which would have yielded a finding of an even larger mammogram screening disparity.
As we predicted, women with schizophrenia spectrum disease were less likely to receive screening compared with women with other diagnoses (depression, anxiety, and bipolar disorder). Although other studies have had similar findings (
8,
26), we are unaware of another study with such extensive diagnostic data from mental health providers in a large cohort of publicly insured patients, which allowed for comparisons across diagnostic categories of severe mental illness in a diverse and vulnerable population. Other studies have been more limited; for example, they have compared breast cancer screening rates for women with psychotic illness with rates in the general population, or they have included only women with private insurance, or they have not reported rates for racial-ethnic groups (
8,
25–
28). Our findings replicate previously reported results that women with co-occurring psychotic and substance use disorders may be particularly less likely than those with other psychiatric disorders to get preventive screening and emphasize the importance of targeted outreach to these populations (
26).
Finally, our data suggest that nonpsychiatric health care utilization improved breast cancer screening for women with severe mental illness. To our knowledge, this finding has not been described previously. The impact was so powerful that it mediated racial-ethnic differences in breast cancer screening rates. These findings support the importance of integration of care for this highly vulnerable population (
29). Even though there is a substantial evidence base describing collaborative care to screen and treat depression in primary care (
30), much less has been published regarding collaborative care approaches for people with severe mental illness (
31). Some have suggested that community mental health clinics might better function as the primary care medical home for this patient population (
32). In these models, primary care services are colocated in community mental health clinics to serve patients who are too psychotic or disorganized to access care in traditional primary care clinics (
33). The Primary and Behavioral Health Care Integration grant program, which is funded by the Substance Abuse and Mental Health Services Administration, has provided some initial evidence of effective programs to improve medical care for this population (
34).
A main limitation of our study was that measurements were limited to one year of breast cancer screening data, which necessitated using an estimated value to compare with the U.S. general population screening rates. In addition, the age group categories imposed by our partners at the state level limited our ability to focus exclusively on women exactly age 50 and over, as the USPSTF guidelines recommend. Strengths of our study include a large sample, a racially and ethnically diverse cohort, and the unique availability of health care utilization data (mammogram receipt, psychiatric diagnostic categories, and nonpsychiatric health care utilization in the past year) for women with severe mental illness.
Conclusions
Although our findings demonstrate disparities in breast cancer screening for women with severe mental illness compared with the general population, they also highlight the potential benefits of more integrated care. Decision-making challenges, complexities of navigating care, and disparities between those with mental illness and those without extend beyond screening and into the treatment phase of breast cancer (
35,
36). One study among homeless and marginally housed women in New York City, a group with some similarities to our cohort with severe mental illness, reported that 53% of women who received screening mammograms did not know their results (
23). Specific ideas relevant to the integration of breast cancer screening and follow-up for those with severe mental illness include flagging screening results for additional outreach for women with psychotic illness or a substance use disorder, special screening sessions for women with severe mental illness during which quick communication of results are given, and sending mammogram results to both primary care and mental health providers.
Increased mammogram screening alone does not necessarily result in reduced mortality (
3,
16,
37). Screening is not entirely benign given that the cumulative risk of a false-positive result over ten years of annual breast cancer screening is approximately 61%, and overdiagnosis is estimated to be as high as 19% (
3,
38). Screening and treatment complexities are important to consider for those with severe mental illness, who may find navigating a confusing health care system and unclear decision-making algorithms particularly challenging (
39–
42). These complexities alongside our encouraging findings of improved screening among women with severe mental illness who utilize nonpsychiatric health care, highlight the importance of efforts to integrate care for improving screening disparities in this vulnerable population. Future research should focus on the development, implementation, and evaluation of novel and integrated clinical, systemic, and policy-level approaches to increase breast cancer screening and treatment among women with severe mental illness.
Acknowledgments
Study investigators acknowledge CalMEND staff for their assistance in combining administrative databases without compensation.