Out-of-pocket health care expenses are growing for many Americans as a result of increases in patient cost sharing, the prevalence of high-deductible health care plans, the use of high-cost pharmaceutical drugs, and other factors (
1–
5). High out-of-pocket costs have been associated with nonadherence to care and may negatively affect quality of life and various health care outcomes (
6–
14). Out-of-pocket expenses may be particularly problematic for patients with depression, who already face higher costs for multiple chronic conditions compared with patients without depression, as shown in analyses that controlled for mental health utilization, sociodemographic factors, and severity of illness (
15). Despite the Mental Health Parity Act, determination of equivalent coverage is imperfect, and the use of carve-outs for mental health benefits may lead to fragmentation of care, thereby leading to higher costs (
16). In addition, depression is more common among persons with lower incomes. Over 15% of persons with incomes below the federal poverty level have depression, compared with 6.2% of persons with incomes at or above the poverty level (
17). Discussion of costs during psychiatry appointments offers important opportunities to ensure that financial burden does not exacerbate an existing disability.
In previous survey studies, almost two-thirds of patients indicated a desire to discuss out-of-pocket expenses with their physicians, but only approximately 15% reported ever doing so (
18,
19). Physicians regularly cite insufficient time, lack of habit, lack of perceived solution, their own discomfort, and their perceptions of the patient’s discomfort as barriers to discussing out-of-pocket expenses (
20–
22). However, in our previous analysis of physician-patient interactions, we discovered that conversations about health care expenses were more common than previously thought, occurring in 30% to 43% of psychiatry appointments, depending on how cost conversation was defined (
23).
In the study presented here, we explored outpatient psychiatric interactions in more depth, by characterizing the content of health care expense conversations that occurred during visits between psychiatrists and patients with major depressive disorder. We analyzed naturally occurring dialogue from private-practice, community-based psychiatric clinic visits that took place between 2010 and 2014. By exploring the frequency and duration of discussions about health care cost in these encounters, as well as the cost-reducing strategies therein, we are able to provide novel insights about the extent to which psychiatrists and patients discuss efforts to manage out-of-pocket health care costs. By doing so, we hope to help psychiatrists recognize the many ways in which they can help patients reduce out-of-pocket expenses.
Methods
Sample Description
Patient visits were sampled from the Verilogue Point-of-Practice database of audio recorded and transcribed clinical encounters (
www.verilogue.com). Visits took place from May 2010 to January 2014 for medication management in outpatient, private-practice offices across the United States. Details of the sample have been discussed in previous publications (
23,
24). Briefly, Verilogue recruits physicians randomly from available lists of active, board certified physicians and pays them to record patient visits for the purpose of marketing or health services research. No other specific inclusion or exclusion for the physicians exist; the recruitment rate is 1:1,200. Physicians and patients are unaware of the research questions for which their recorded visits will be used. Patients are approached and asked to provide consent to participate prior to initiation of the visit, with approximately 80% of patients agreeing to participate. In the sample, only one visit per patient is included, although multiple visits per provider may exist. The sampled visits can occur at any time within the patient-physician relationship. All protected health information is removed during the transcription process; no other information is censored. This study was approved by the Duke University Institutional Review Board.
Cost-Related Measurements and Analytic Approach
We defined “cost conversation” as any mention of the patient’s out-of-pocket expenses or insurance coverage for a past, present, or potential health care service. The development and validity of this definition has been discussed in detail elsewhere (
23). To mitigate individual coder biases and errors, encounters were analyzed independently by at least two team members. The following cost-related measures were evaluated. First, we determined the presence or absence of a cost conversation. If a cost conversation was present, we then determined which interventions were related to the cost conversation, the duration of the cost conversation, and the discussion of cost-saving strategies. The duration of the cost conversation was calculated by multiplying the total number of cost-related words by the average rate of words spoken, as described elsewhere (
23). A team member experienced in conversation analysis assessed coder agreement on each of the above measures. In cases of agreement, the corresponding decision was assigned as “final.” When there were discrepancies, the final coding decision was decided by group consensus. Team members with clinical experience (WGH and PAU) supervised coder training and discrepancy resolution to ensure proper interpretation of clinical matters. All coding was applied using NVivo software, version 10.
Statistical Analysis
We compared cost discussion code frequencies by using Pearson’s chi-square tests and Fisher’s exact test, and we calculated 95% confidence intervals by using Clopper and Pearson’s exact method (
25). We used nonparametric Kruskal-Wallis and Mann-Whitney U tests to compare duration of cost discussions, because the distribution of these durations was nonnormal. Statistical analyses were conducted using R software (R Core Team, version 3.1;
www.R-project.org). All authors had full access to the data and take responsibility for the data’s integrity.
Results
Study Population
Our final sample included 422 clinic visits. Characteristics of patients and psychiatrists are provided in
Table 1. A total of 422 patients with major depressive disorder were included in our study. They were predominantly female (66%), 35 to 54 years of age (44%), and white (83%). Eight percent of patients were uninsured, which is similar to the national average of 9.8% for patients with depression (
26). A total of 36 psychiatrists were included in this study; they recorded a median of 13 visits each (interquartile range [IQR]=4–17 visits), were all male, and most commonly had 21 to 30 years of experience in practice (44%). Data on physicians’ race were not available. The clinic visits occurred in 20 states: Arizona, Georgia, Hawaii, Illinois, Indiana, Kansas, Kentucky, Massachusetts, Michigan, Minnesota, Mississippi, North Carolina, New Jersey, New York, Ohio, Pennsylvania, South Carolina, Texas, Virginia, and Wisconsin.
Incidence of Cost Conversations
Thirty-eight percent of visits (N=161 of 422) contained a cost conversation (95% confidence interval [CI]=33%–43%). Incidence of cost conversations varied significantly by patients’ insurance status and was highest among uninsured patients (N=21 of 33, 64%), followed by patients enrolled in private insurance plans (for example, Aetna and Blue Cross–Blue Shield) (N=84 of 190, 44%) and then by patients enrolled in public insurance plans (that is, Medicare and Medicaid) (N=50 of 168, 30%) (p<.001 for comparison across groups). Additionally, incidence of cost conversations was higher in visits with white, non-Hispanic patients, compared with visits with nonwhite or Hispanic patients (N=142 of 352, 40% versus N=19 of 70, 27%; p=.05). Finally, cost conversations were more common in visits with middle-aged patients (35 to 54 years old; N=80 of 184, 43%) than with younger patients (19 to 34 years old; N=37 of 96, 39%) or older patients (≥55 years old; N=44 of 142, 31%) (p=.06 for comparison across age groups).
Topics and Initiators of Cost Conversations
Twenty-two percent of cost conversations (N=36 of 161) addressed costs for more than one clinical topic: 16% (N=26 of 161) addressed two different topics, and 6% (N=10 of 161) addressed three different topics. In sum, 208 different cost topics were discussed in our sample. Cost conversations most commonly addressed medications (N=136 of 208, 65% of all cost conversation topics), and more than half dealt with costs for psychotropic drugs (N=107 of 208, 51%). The most frequently discussed classes of psychotropic medications were serotonin norepinephrine reuptake inhibitors (SNRIs; N=22 of 208, 11% of all cost conversation topics) and antipsychotics (N=22 of 208, 11%). Selective serotonin reuptake inhibitors (SSRIs), sleep aids, and stimulants were discussed less frequently, constituting 7% (N=15 of 208), 7% (N=15 of 208), and 5% (N=10 of 208) of cost conversation topics, respectively. The costs of over 50 different medications were discussed in our sample; the most frequently mentioned were duloxetine (Cymbalta), aripiprazole (Abilify), quetiapine (Seroquel), zolpidem (Ambien), bupropion (Wellbutrin, Aplenzin), and escitalopram (Lexapro). Examples of medications among the different classes as well as a single example representative of the seven conversations that discussed cost of medications in general are available as an online supplement to this article.
Nonpharmacologic therapies and services accounted for 35% of cost conversation topics (N=72 of 208) and most commonly addressed costs for psychotherapy (N=19 of 208, 9%), provider visits for medical management (N=19 of 208, 9%), procedures (N=9 of 208, 4%), and medical equipment (N=5 of 208, 2%). Two cost conversations discussed the cost of neuropsychiatric testing. Of the conversations pertaining to procedures, five involved electroconvulsive therapy (ECT) or transcranial magnetic stimulation (TMS) and one discussed a vagus nerve stimulator.
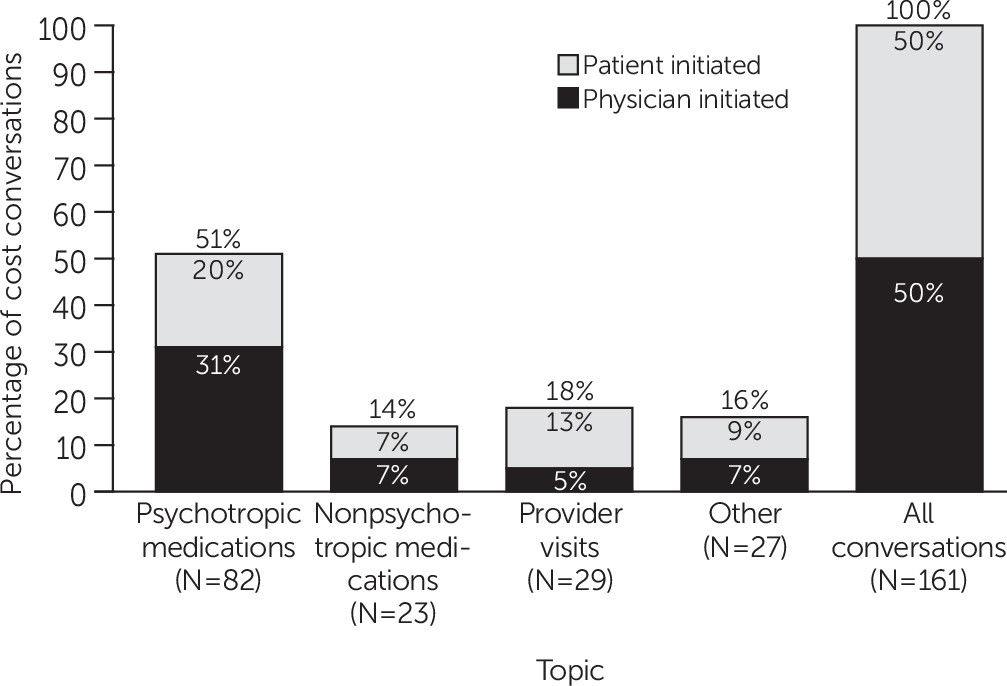
Nearly equal percentages of cost conversations were initiated by physicians and patients (N=81 of 161, 50%; N=78 of 161, 48%; respectively). Rarely, cost conversations were initiated by patients’ caregivers or companions (N=2 of 161, 1%). The breakdown of initial cost topics and who initiated them is presented in
Figure 1. A significantly greater percentage of physician-initiated cost conversations initially addressed costs for psychotropic medications (N=50 of 81, 62%) compared with those cost conversations initiated by patients (N=30 of 78, 38%; p
=.009 for comparison of percentages of physician versus patient initial cost topics which addressed psychotropic medications). By contrast, a significantly greater percentage of patient-initiated cost conversations initially addressed costs for provider visits (N=21 of 78, 27%) compared with physician-initiated cost conversations (N=8 of 81, 10%; p=.008 for comparison of percentages of physician versus patient initial cost topics which addressed provider visits).
Discussion of Cost-Reducing Strategies
Overall, 45% (N=72 of 161) of cost conversations involved at least one cost-reducing strategy (CI=37%–53%). Sixteen percent of cost conversations (N=26 of 161) involved discussion of two or more unique cost-reducing strategies. In sum, physicians and patients discussed cost-reducing strategies for 110 of the 208 total cost topics addressed in our sample (53%).
Cost-reducing strategies most commonly dealt with costs for psychotropic medications (N=86 of 110; 78%) (
Table 2). Specifically, psychiatrists and patients most often mentioned cost-reducing strategies for antipsychotics (N=22 of 110, 20%) and SNRIs (N=22 of 110, 20%, also). Fifteen percent (N=16 of 110) of cost-reducing strategies pertained to nonpharmacologic topics, such as provider visits (N=7 of 110, 6%) and other topics, including procedures, diagnostic testing, and medical equipment (N=9 of 110, 8%).
The majority of cost-reducing strategies (N=75 of 110, 68%) did not require changes to the care plan. Instead, they involved discussions of lowering cost by changing the source or timing of an intervention (N=25 of 110, 23%), providing free samples for the purpose of lowering the patient’s costs (N=25 of 110, 23%), or facilitating use of copay assistance programs (CAPs) or cost-saving coupons (N=22 of 110, 20%). The remaining 32% of cost-reducing strategies (N=35 of 110) required changes to the care plan, such as switching to a lower-cost therapy or diagnostic (N=24 of 110, 22%) and changing the dose or frequency of an intervention (N=11 of 110, 10%).
Frequently, psychiatrists and patients sought to lower costs for psychotropic medications by providing free samples or facilitating use of CAPs or coupons. These often involved a variety of interrelated scenarios in which the doctor offered a medication option because he or she had samples, offered a trial of the medication before writing a prescription, or offered to start the patient on a sample of medication that also is associated with a coupon program (
Table 3). Sometimes psychiatrists discussed coupon programs for nonmedication expenses (for example, a conversation around gender affirmation surgery that utilized a grant program).
Sometimes psychiatrists recommended reducing expenses by switching to a different formulation of the same medication. This was particularly true with bupropion (example in
Table 3). Other times, psychiatrists lowered patients’ expenses by prescribing generic medications that were not the equivalent of the brand-name medications that patients had taken previously (
Table 3).
Sometimes psychiatrists lowered patients’ expenses by changing the source or timing of medications (for example, discussing an alternative location for obtaining the medication, such as using a different pharmacy to obtain a lower price). Other times, psychiatrists lowered patients’ medication expenses by prescribing a different quantity of medications (for example, a 90-day versus 30-day prescription).
Psychiatrists also reduced patients’ expenses by addressing the source or timing around nonmedication expenses (for example, by having a patient come to another office location that would accept the new insurance plan, or by spacing out the intervention, such as the appointment follow-up time). Psychiatrists also suggested logistical changes to reduce therapy expenses (for example, by recommending that patients seek counselors through churches) (
Table 3). Discussions around ECT and TMS often focused on obtaining insurance approval.
Duration of Cost Conversations
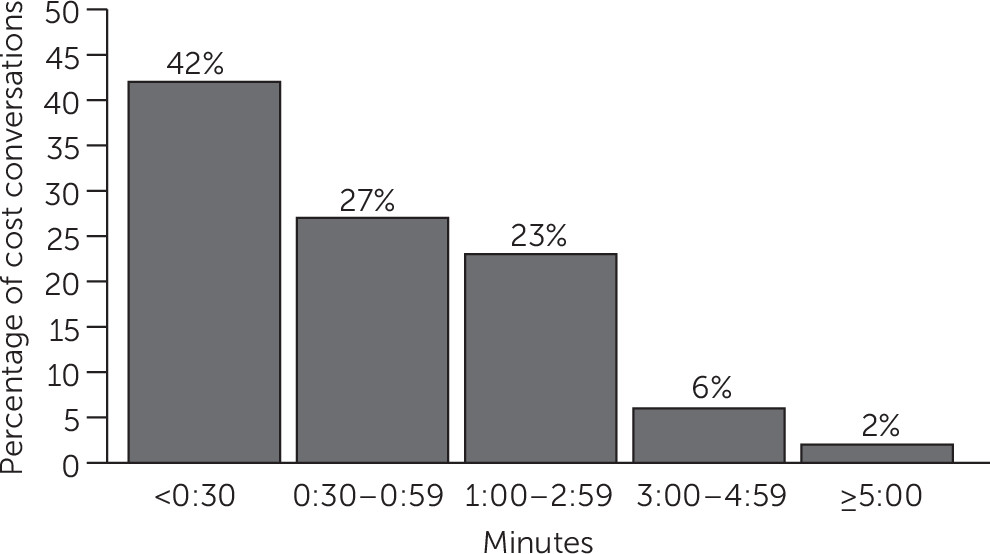
The median visit duration in our sample was 12 minutes and 15 seconds (IQR=9 minutes and 13 seconds to 18 minutes and 36 seconds). In visits containing cost conversations, the median time spent discussing patients’ health care costs was 36 seconds (IQR=16–81 seconds). The majority of cost conversations lasted less than one minute (69%), and 8% lasted three minutes or longer (
Figure 2). There was no significant difference in the duration of cost conversations initiated by physicians versus patients. However, cost conversations containing discussion of cost-reducing strategies lasted significantly longer than those without such discussion (median=71 seconds and 22 seconds, respectively, p
<.001).
Discussion
We analyzed the content of outpatient encounters between patients being treated for depression and their psychiatrists and discovered that discussion of health care costs was common, typically brief, and frequently focused on ways of reducing patients’ out-of-pocket expenses. Cost conversations occurred in more than one in three visits and focused mainly on costs for psychotropic medications. Notably, psychiatrists and patients differed with respect to the cost topics they initiated. Psychiatrists were more likely to bring up costs for psychotropic medications, whereas patients were more likely to bring up costs for provider visits.
Why are psychiatrist-initiated conversations disproportionately focused on medication costs? The combined cost-reducing strategies around free samples and the use of CAPs or coupons accounted for over 40% of the cost-reducing strategies discussed. Previous survey data have indicated that physicians will change prescribing habits, deviating from their preferred drug, if samples are present (
27). The availability of samples and coupon programs in the clinics is unknown, although familiarity with these strategies may explain the high rates of discussion. A prior study indicated that physicians with high perceived knowledge of medication costs are more likely to discuss costs (
28). Physicians may be more likely to initiate cost discussions on the topics in which they perceive greater knowledge and comfort. Patients, conversely, may have greater motivation to initiate conversations with greater immediate out-of-pocket expenses, such as high copays, coinsurance, or deductibles.
Our study also highlights that out-of-pocket expenses can be reduced without necessarily changing the course of clinical care. Although a variety of cost-reducing strategies were used, the majority of strategies did not alter the plan of care. However, the long-term effects of these cost-reducing strategies on clinical care are unclear. Although providing free samples or facilitating the use of CAPs or coupons can provide patients with significant short-term cost savings (
29,
30), the long-term effect on patients’ out-of-pocket expenses is possibly detrimental (
31,
32). After the sample or program runs out, patients may be faced with copays for brand-name drugs or even the full out-of-pocket cost of the drugs. In some cost conversations, for example, patients complained about the cost of medications, pointing out that even with coupons and other assistance programs, their out-of-pocket expenses remained high.
Our study also suggests demographic variation in the kind of patients likely to discuss health care costs with their psychiatrists. For example, the rate of discussions among patients older than 55 years was lower than the rate among younger populations. Further studies are needed to better assess the relationship among race, age, and insurance status with regard to cost discussions. Still, not surprisingly, the highest incidence of cost discussions was among uninsured patients. Knowing the patient was uninsured may have made psychiatrists more cognizant of discussing costs. It is not known whether the uninsured patients chose not to use their insurance in order to avoid insurer or employer awareness of the receipt of mental health treatment. Another point of emphasis concerning demographic characteristics is that all physicians in the study were men, although the majority of psychiatrists in the nation are women. Although there is high likelihood of bias in the sample from having only male physicians, the overall impact is not known.
Almost one-half of the cost conversations in this study included discussion of a cost-reducing strategy. One often-cited barrier to communication around costs is the perception of insufficient time (
20,
33). Yet psychiatrists commonly engaged in cost conversations with their patients. This concern over insufficient time has not been borne out in our study. These conversations are and can be succinct. Almost 70% of the cost conversations lasted less than one minute, and a plurality of cost conversations lasted less than 30 seconds, meaning that the vast majority of cost conversations took less than 10% of the visit.
Our study showed that cost conversations occur more often than survey data previously described and that cost-reducing strategies are included in these discussions. However, the study did not establish the effect that these discussions have on out-of-pocket expenses nor did it establish that the cost conversations are as effective as they could be. Discussions about cost-reducing strategies do not necessarily lead to lowered expenses for the patient (for example, substitution of Pristiq for Effexor in one encounter). Further research is required to characterize strategies that improve the efficiency, quality, and patient-centeredness of cost discussions. This would include evaluation of strategies that can reliably lead to changes in out-of-pocket expenses. In some encounters, neither psychiatrists nor patients were able to assign costs to specific interventions accurately. Indeed, frustration around the complexities in health care reimbursement was a common theme, with psychiatrists and patients at times aligning against such perceived barriers. Greater price transparency could help alleviate some of the difficulties in determining out-of-pocket expenses and facilitate the discussion around cost-reducing strategies (
20,
34).
There are some additional limitations to the study. Generalizability of the findings may be further limited, given that the sample did not include academic settings, hospital-based clinics, or community mental health clinics. However, the relatively large sample size, geographic diversity, and variety of insurance coverage makes this study more broadly generalizable than previous ones. Because we had access to only one visit per patient, we could not determine whether cost conversations occurred during preceding encounters—thus limiting the need for discussion in the sampled visit. Furthermore, other psychiatric conditions may have different rates of cost conversations.
Conclusions
In clinic visits for depression management, we found that patients and psychiatrists discuss costs regularly, in more than one in three visits. Interestingly, patients and psychiatrists initiated cost conversations with nearly equal frequencies, although they differed with respect to the costs they brought up more often: psychiatrists tended to bring up costs for psychotropic medications and patients tended to bring up costs for provider visits. Importantly, almost half of cost conversations mentioned a cost-reducing strategy, which most often pertained to the use of free samples or facilitation of CAPs or coupons. Cost conversations were usually brief, with the majority lasting less than one minute. This study provides novel insights into the topics and cost-reducing strategies discussed in outpatient psychiatrist-patient visits for management of major depressive disorder.