European population studies have documented increasing diagnosis and treatment of attention-deficit hyperactivity disorder (ADHD), obsessive-compulsive disorder, and bipolar disorder (
8,
9). Provider surveys that compared U.S. mental health visit rates in 1980s–1990s, 1995–1998, and 2007–2010 indicated increased psychiatric complaints and visits for treatment (
10–
12). A recent representative survey of U.S. households found mental health service use increased for youths ages 6–17 from 9.2% in 1996–1998 to 13.3% in 2010–2013 (
13). Inpatient data have suggested pediatric mental health hospitalizations are increasing (
14,
15) but length of stay is decreasing (
16). However, these studies examined care provided overall, not specific diagnoses or specific patients; results cannot determine whether patient numbers, or number of visits for existing patients, are increasing.
Reported increases may relate to increased population prevalence, ease of diagnosis, or use of mental health care and psychotropic medications related to improved mental health care coverage (
21,
22). Pediatric mental health trends in a population of children with consistent health insurance have not been reported, and previous studies of youth mental health treatment have not included uncommon but severe disorders (
10,
23). Examinations of psychotropic medication use have largely focused on numbers of visits with psychiatric prescriptions; parental report of medication use; children with public insurance at higher mental health–related risk; specific psychotropics, such as antipsychotics; or specific diagnoses, such as autism or ADHD (
10,
13,
20,
24–
27). Studies linking prescription billing data with diagnosed mental health conditions across a large diverse population have not been reported.
Children who are military dependents may be at increased risk of psychiatric disorders. Parental concerns about a child’s psychological health as well as inpatient and outpatient mental health care of children are known to increase during and after a deployment (
28–
31). Children with a military parent have reported higher rates of depression, suicidal ideation, suicide attempts (
32,
33), and hospitalizations; however, data did not account for insurance coverage (
34). Despite having access to high-quality health care, youths with military connections may experience barriers to care related to perceived stigma, confidentiality concerns, and military moves (
35). Although soldiers have reported decreased stigma and increased mental health care use over time (
36), use patterns of military-connected youths have not be reported.
Methods
We performed a retrospective trend study of treated psychiatric diagnoses, treatment, and psychiatric medication prescriptions by using the TRICARE Management Activity Military Health System (MHS) database. This database records care provided to uniformed services members and their dependents at military and civilian health care facilities domestically and abroad. Civilian facilities provide more than half of all care (
28). Our population included all children who were ages 2 to 18 at the beginning of each year from 2003 to 2015 and who were enrolled in the MHS for 11 or more months of that year. Included children were family members of active duty troops, retirees, or National Guard and Reserve troops in active roles; 11 months of required enrollment likely removed many children of National Guard and Reserve troops who received MHS care only during parental active duty service.
Mental health care visits were identified in the outpatient record by ICD-9 diagnostic codes classified by Healthcare Cost and Utilization Project (HCUP) Clinical Classification Software as mental health care. Visits for mental health care were identified by HCUP subcategories for adjustment, anxiety, attention-deficit, conduct, and cognitive disorders; disorders first identified in childhood; impulse control, mood, personality, and psychotic disorders; suicidal ideation; alcohol use and substance use disorders; and miscellaneous mental health conditions (dissociative, eating, and factitious disorders). Mental health subcategories for developmental delay and screening were excluded. Children with one or more diagnoses for a given mental health category were categorized as having that condition and as having a mental health condition within the year. Children could have more than one subcategory of psychiatric diagnosis. All mental health visits were counted for the given year. Means and medians of mental health care visits were calculated, and trends were reported.
Data on psychiatric medication prescriptions were extracted from the outpatient pharmacy record, which includes all outpatient prescription medication data. Prescriptions can be filled at military, civilian, or mail-order pharmacies at low or no cost. Using the American Hospital Formulary System, medications were sorted into the following therapeutic classes: stimulants, nonstimulant ADHD medications, antipsychotics, antidepressants, anxiolytics, and mood stabilizers. Children with one or more psychiatric medication prescription were classified as using that class of medication and using a psychiatric medication within the year.
Chi-square analyses compared groups on the prevalence of treated psychiatric disorders overall and mental health subtypes. The Cochran-Armitage test was used to identify significant trends in psychiatric diagnoses overall and by mental health subtype, outpatient mental health visits, and psychiatric medication use overall and by class. The Poisson regression was used to calculate prevalence rate ratios (RRs) and 95% confidence intervals (CIs) to analyze trends over the study period. Adjusted models accounted for child gender and parental rank. When clearly not linear, trend analyses were completed on smaller time segments. Analyses were conducted by using Stata Intercooled, version 13; p<0.05 was considered statistically significant. The study was reviewed and approved by the responsible institutional review boards.
Results
An average of 1,798,530 children ages 2–18 received health care each year in the MHS from 2003 to 2015, ranging from 1,738,856 (2015) to 1,873,549 (2010) children. On average, 8.9% of included children had a parent of junior-enlisted rank (military rank of E-4 or below), ranging from 8.0% in 2006 to 10.4% in 2010. A slightly higher percentage of children were boys; the largest age group was children ages 6–13. Of children with diagnosed mental health conditions, 57%–60% were male, and an average of 8% had a parent of junior-enlisted rank (
Table 1).
Psychiatric Diagnoses
In 2003, 9.2% of included children had a diagnosed mental health condition; this percentage increased to 15.2% of children in 2015. Over the 13-year period, the prevalence of treated mental health conditions significantly increased by 4% per year (RR=1.04, 95% CI=1.04–1.05, p<0.001;
Table 2) in unadjusted analysis. ADHD and conduct disorder diagnoses were the most common diagnosis, affecting 5.1%–8.1% of children, followed by mood, adjustment, and anxiety disorders. The treated prevalence of diagnoses in each subcategory of mental health care increased from 2003 to 2015, with the exception of alcohol-related disorders. Prevalence of identified suicidal ideation increased the most, from 0.01% in 2003 to 0.53% in 2015, a 20% increase (
Table 2). Trends were fairly consistent across gender, parental military rank, and age.
Mood, depressive, personality, psychotic, alcohol use, substance use, and suicidal ideation diagnoses were more than twice as common in children ages 14–18 compared with children younger than age 13 (p<0.001 for all diagnostic categories in 2003 and 2015; results not shown). Children ages 6–13 had the highest treated prevalence of ADHD or conduct disorder diagnoses (p<0.001). Most psychiatric diagnoses increased at a slightly higher rate for children ages 14–18 (p<0.001), with the exception of suicidal ideation, which increased at a slightly higher rate for children ages 6–13 (RR=1.24, 95% CI=1.18–1.30, p<0.001).
The percentage of children with a diagnosed mental health condition was higher among boys than girls in 2003 (10.9% vs. 7.9%, p<0.001) and 2015 (17.1% vs. 13.2%, p<0.001). In both 2003 and 2015, boys were significantly more likely to have disorders diagnosed in childhood (p<0.001), ADHD (p<0.001), or impulse control disorders (p<0.001). Girls were significantly more likely to have diagnosed mood and depressive disorders (p<0.001) and suicidal ideation (p<0.001).
Mental Health Care
The total number of mental health care visits rose from 1,055,100 in 2003 to 2,148,451 in 2015. The number of mental health care visits per child per year was not normally distributed. The mean number of visits per child with a psychiatric diagnosis increased from 6.3 in 2003 to 8.0 visits per year in 2015, a 2% (p<0.001) increase per year in unadjusted and adjusted analysis (
Table 2); the median remained consistent at three visits per year.
Psychiatric Medications
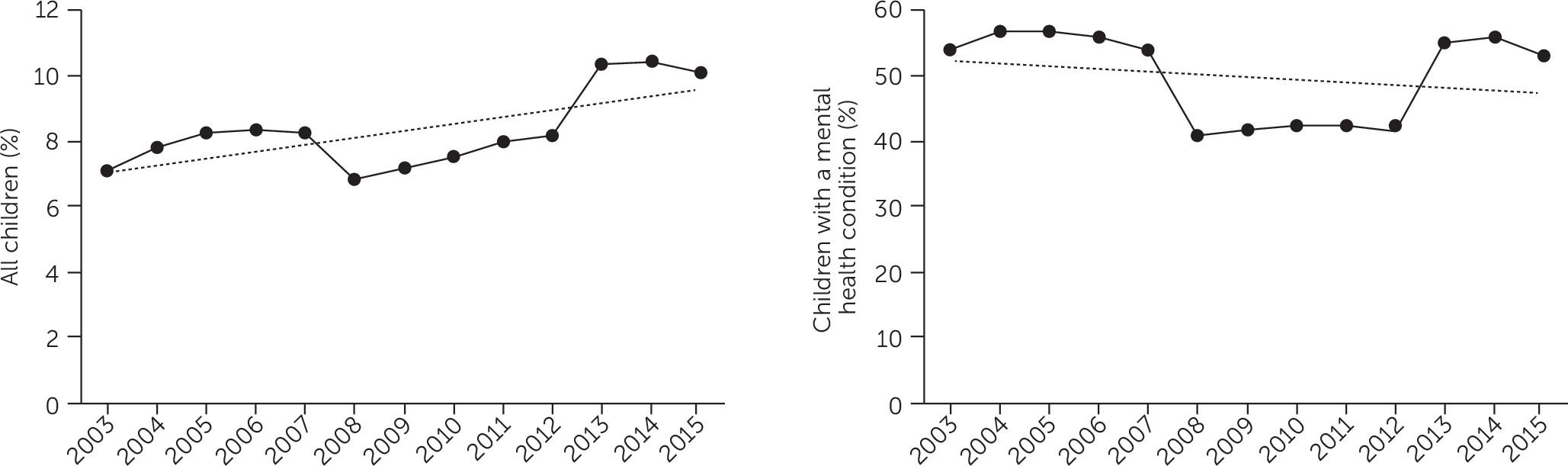
The percentage of all children who received a psychiatric medication prescription increased significantly from 7.1% in 2003 to 10.4% in 2015, a yearly increase of 3.0% (RR=1.03, p<0.001;
Figure 1); the RR became nonsignificant after adjustment for demographic characteristics. In unadjusted analysis, prescriptions for nonstimulant ADHD medications, antipsychotics, antidepressants, and anxiolytics, all significantly increased for the population of children over the course of the study (
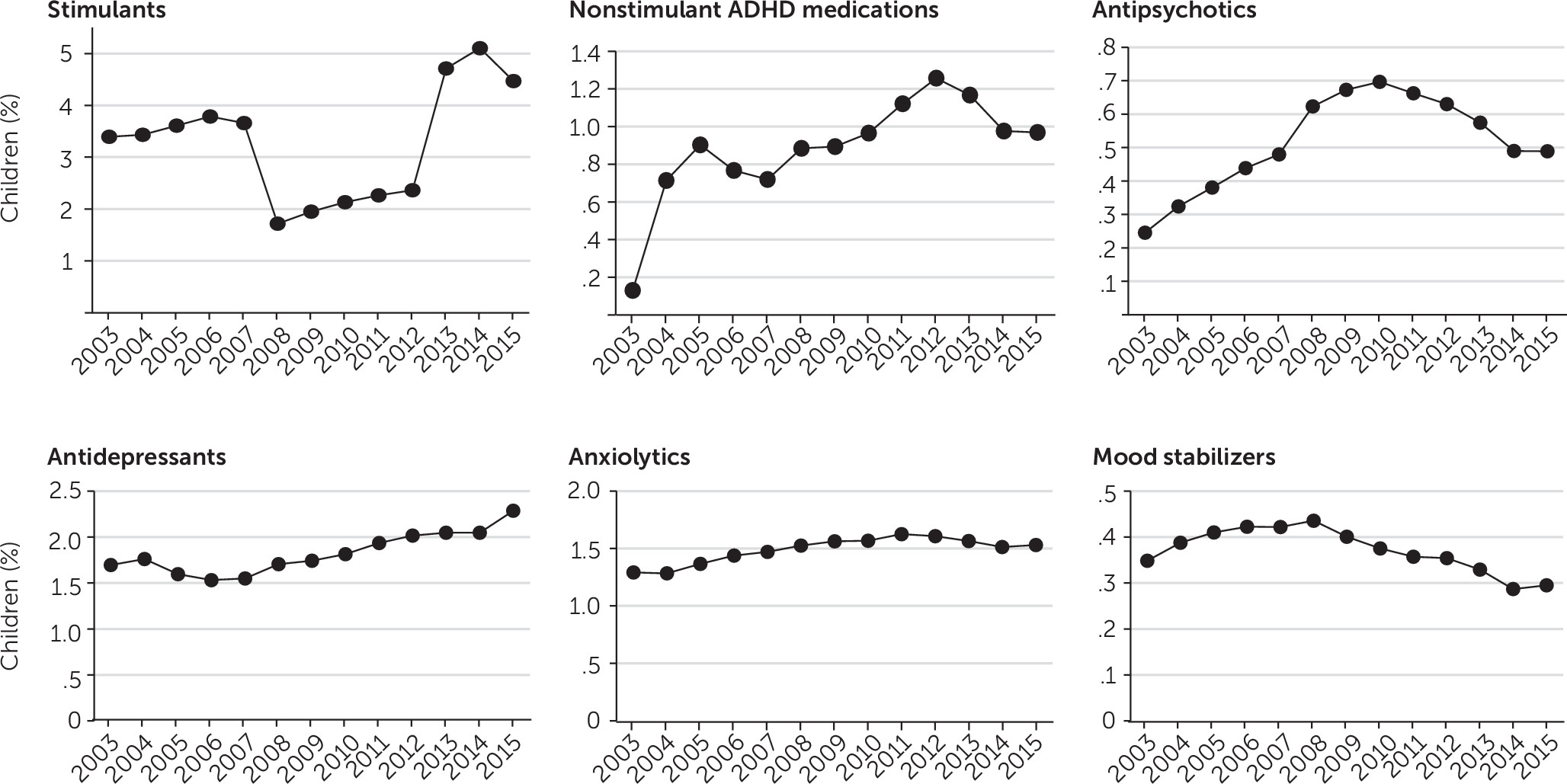
Figure 2). Prescriptions for mood stabilizers decreased, and stimulant prescriptions did not change significantly.
After the analysis was adjusted for demographic characteristics, it was shown that prescriptions of anxiolytics increased significantly and prescriptions of antidepressants and mood stabilizers decreased significantly. Stimulant prescriptions did not follow a linear trend (
Figure 2); they increased from 2003 to 2007 (RR=1.02, 95% CI=1.01–1.04, p=0.001) and from 2008 to 2011 (RR=1.09, 95% CI=1.08–1.11, p<0.001), but they did not significantly increase from 2012 to 2015 (RR=1.18, 95% CI=0.95–1.45, p=0.13). Stimulants were the most commonly prescribed class of medication, with 2% to 5% of children having a prescription each year. Stimulants, antipsychotics, antidepressants, and anxiolytics all increased the most for children ages 14–18 (p<0.001). Nonstimulant ADHD medications increased for children ages 2–5 and ages 14–18 (p<0.001). Antipsychotics and antidepressants increased for children ages 6–13 (p<0.001). Stimulant medication prescriptions increased for children with junior-enlisted parents but not for children with parents who had senior military rank (p<0.001). All medication prescription trends were consistent across gender.
For children with psychiatric diagnoses, psychiatric medication prescriptions did not increase (53.8% of children in 2003 vs. 52.6% of children in 2015: RR=0.99, 95% CI=0.97–1.01, p=0.29; adjusted RR [ARR]=0.98, 95% CI=0.96–1.00, p=0.42;
Figure 1). Prescription data were not linear; two time periods showed a small statistically significant increase in prescriptions (2008–2011: RR=1.01, 95% CI=1.01–1.01, p<0.001; 2012–2015: RR=1.01, 95% CI=1.01–1.01, p<0.001). The period from 2003 to 2007 did not show any significant changing trend.
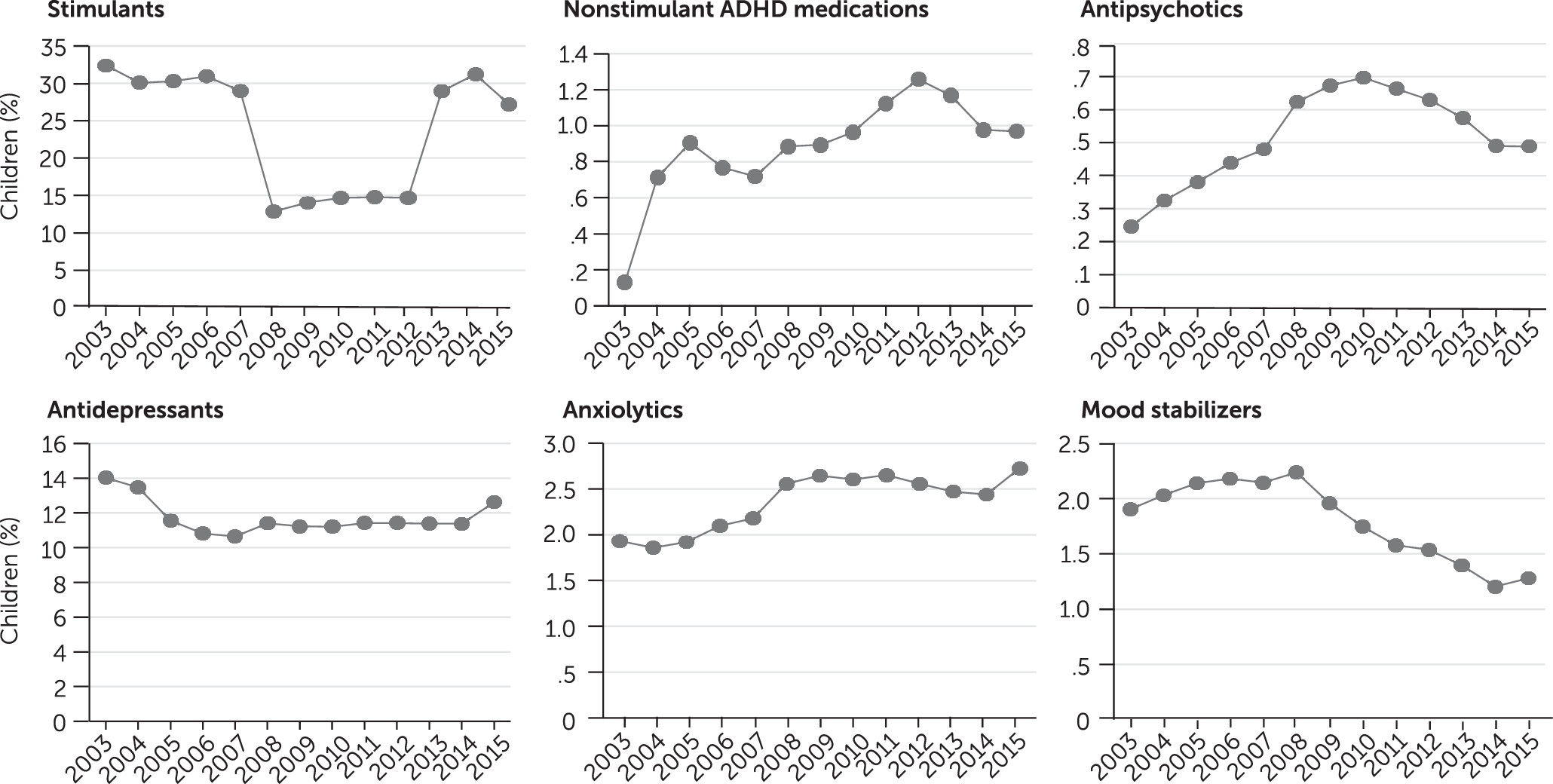
For children with psychiatric diagnoses, in unadjusted analysis, anxiolytic prescriptions significantly increased, and mood stabilizer prescriptions significantly decreased (
Figure 3). After adjustment, prescriptions for antipsychotics (ARR=1.07, p<0.001) and anxiolytics (ARR=1.04, p<0.001) increased significantly, and stimulants decreased (ARR=0.98, 95% CI=0.96–1.00, p<0.05); however, stimulant prescriptions did not follow a linear trend. For children with diagnosed mental health conditions, stimulant prescriptions increased for children with junior-enlisted parents but not for children with parents who had senior military rank. Antidepressant prescriptions decreased for children ages 2–5 but not for older children. Anxiolytics increased for children ages 6–18 (p<0.001) but not for younger children.
Discussion
We found that between 2003 and 2015, the percentage of military-connected children with a diagnosed psychiatric diagnosis increased significantly (9.2% vs. 15.2%), as did mean health care visits per year (6.3 vs. 8.0) and the percentage of children prescribed a psychiatric medication (7.1% vs. 10.0%). However, psychiatric medication prescriptions did not increase in children with diagnosed mental health conditions. Medication increases were largely in older children.
This research indicates an increasing trend in children’s psychiatric diagnoses over 13 years. The treated prevalence in our population is lower than reported estimates of 13% to 20% of U.S. children for 2005–2011 (
3,
7,
13). This percentage of children with psychiatric diagnoses may be lower than national estimates because of study methods requiring a psychiatric diagnosis, inclusion of children as young as age 2, the fact that military pediatrics skew toward younger children (
38), and possible military-related stigma surrounding seeking care (
35). Results mirror previously reported trends of increased psychiatric diagnoses in children (
10,
13) with consistent health insurance coverage.
This study period fell entirely during the wars in Afghanistan and Iraq; increased mental health care and psychiatric medication use of military-connected children is consistent with research linking parental wartime deployment and child mental health care needs (
28,
29). However, mirroring nationally reported trends (
10,
13), diagnosed mental health conditions increased consistently without marked upsurges in periods of high-intensity combat deployments in 2007–2008 and 2010–2012 (
39,
40).
Consistent increases in mental health care and psychiatric medication prescriptions, without marked upsurges at times of increased military deployment, suggest that parental deployment did not drive increased psychiatric diagnoses and care or that effects of deployment and military life significantly affected ongoing mental health risk. Findings may also be related to the enactment of the 2011 mental health care provision in military schools (
41), although the late initiation date and the fact that 80% of military children attend public schools (
42) suggests that school programs do not fully explain the results. National efforts to support primary care providers through telemedicine and links to specialty providers may also contribute to outcomes, given that primary care providers’ comfort with diagnoses and treatment of children’s mental health conditions may have increased during the study period.
Of all subcategories of psychiatric diagnoses, suicidal ideation increased the most: a 20% per year increase over the time period, a 40% increase in adjusted analysis, and a 24% increase for children ages 6 to 13. This study did not identify deaths by suicide, yet findings of increases in diagnosed suicidal ideation in this study are consistent with increasing rates of suicide among children and youths reported elsewhere (
43). Consistent with research on the prevalence of suicidal ideation among young people in clinical settings, we found that the identified prevalence of suicidal ideation was almost twice as common among girls as among boys (
44). Increased use of HEADSS (Home & Environment, Education & Employment, Activities, Drugs, Sexuality, Suicide/Depression) interviewing, stronger U.S. preventive task force recommendations, use of the Patient Health Questionnaire–9 (Adolescent), and increased militarywide attention to depression and suicide may suggest that the increases are related to identification.
Mean mental health care visits rose 2% per year in unadjusted and adjusted analyses from 6.3 to 8.0 visits per child per year. The median number of visits did not increase. Results suggest that increases in outpatient care are driven by severe cases; trends toward decreased inpatient child mental health care may support this finding (
16). Although this study did not examine the care provision site, a known dearth of military mental health providers (
45) suggests that a substantial portion of care was provided outside the military, indicating that civilian providers need to be aware of issues surrounding military life.
In our population of nearly 2 million children a year, we found that the percentage of all children prescribed psychiatric medications rose from 7% to 10% and stayed at about 50% for children with diagnosed mental health conditions. Previous studies reporting increased psychiatric medication use by U.S. children have not controlled for confounders and have not examined rates among children with and without psychiatric diagnoses (
10,
11,
23). Our findings are at odds with one U.S. study indicating that use of psychiatric medications by children who were publicly insured did not increase from 2004 to 2014 (
20). However, our findings mirror population-level research in Europe indicating increased psychiatric medication prescriptions overall and consistent psychiatric medication use rates in children with psychiatric diagnoses (
17–
19).
The results of this study are consistent with U.S. provider survey research indicating that an increased number of pediatric visits include psychiatric medication prescriptions (
10,
11,
23); the findings are also consistent with parent surveys showing an increasing percentage of children using psychiatric medications (
13). The results suggest that reported increases are related to increased diagnosis of mental health conditions, not an increased medication burden in children with preexisting diagnoses. Psychiatric medication prescriptions for all children and for children with psychiatric diagnoses decreased from 2008 to 2012. This decline is likely due to the black box warnings on ADHD medications in 2007 and on antidepressants in 2004 (
46,
47).
Anxiolytic prescriptions increased, and those for mood stabilizers decreased, for all children and for children with psychiatric diagnoses. Antipsychotic prescriptions increased for all children, and for those with psychiatric diagnoses. Nonstimulant ADHD medications and antidepressants prescriptions increased for the full population but not for children with diagnosed conditions. Increases may be related to the rise in polypharmacy in the treatment of mental health conditions (
48,
49). Decreases in mood stabilizer prescriptions may relate to the movement toward using anticonvulsants (which were not included in this analysis) to treat mood disorders (
50). Psychiatric medications increased the most in older children with all classes of medication—with the exception of mood stabilizers and nonstimulant ADHD medications—increasing more for youth ages 14–18 than for younger children.
In the full population of children, only use of nonstimulant ADHD medications increased in the youngest age group, and use of antipsychotics and antidepressants increased in school-age children. Increased medication use mirrors the increasing diagnosis of mental health conditions in older children. Stimulant ADHD medications increased significantly in children of junior-enlisted parents; increases were evident in those with and without mental health conditions. Finding are inconsistent with research indicating decreased medication for children with ADHD during parental deployment and decreased medication use for children of junior-enlisted parents (
51); however, the results are consistent with studies indicating increased stress burden in junior-enlisted service members (
52,
53), given that child and parental mental health have been linked (
54).
This study had several limitations. It was limited by reliance on ICD-9 coding, which is dependent on providers correctly coding visits. Use of ICD-9 codes also made it impossible to assess the severity of mental health conditions, although the use of codes in claims data ensured that care needs rose to clinical significance. We were also unable to identify providers who made diagnoses and prescribed medications. The large number of included children and nature of a trend study did not allow for identification of risk factors associated with increasing psychiatric diagnoses, including the impact of parental deployment. However, the fact that percentages of psychiatric diagnoses in our population mirrored national estimates suggests parental deployment does not fully explain the increasing treated prevalence of psychiatric diagnoses.
Strengths of this study include a long 13-year time period and a large population of children who received consistent, high-quality medical and mental health care as well as free or no cost prescription medications, which decreased ascertainment and sampling biases. Previous studies of U.S. children have relied on compiling adjacent years to overcome small sample sizes. Our large population allowed us to look at numbers year by year, permitting a closer examination of visit and medication trends. Because prescription data were linked with individual children, we were able to explore medication trends in the total population and in children with diagnosed mental health conditions.