Over the past decade, the experimental therapeutics approach has emerged as a key framework for research, sponsored by the National Institute of Mental Health (NIMH) and other federal agencies, on psychosocial interventions. This approach (
1), rooted in experimental medicine, requires a shift from solely quantifying treatment efficacy (i.e., whether outcomes are achieved) to explaining efficacious effects with a focus on the processes of change (i.e., how outcomes are achieved). The literature includes clinical studies that explicitly implement this approach (
2). However, few studies apply this model to nonbiological targets or to interpersonal and/or social mechanisms of action, such as those involved in psychosocial interventions common in mental health and human services research.
Applying an Experimental Therapeutics Approach in Human Services
The experimental therapeutics approach has been articulated by the NIMH for the past decade. In 2010, the National Advisory Mental Health Council (NAMHC) work group developed a report in response to a perceived need to address the lack of advancement in mental health treatment. It is well known that persons with a mental disorder die on average 8.2 years younger than others in the population (
3). Clients who receive mental health services in the public sector have higher age-adjusted death rates and experience decades of life lost compared with those without mental disorders (
4). The NAMHC work group emphasized the need to “discover and develop novel, effective interventions that prevent and cure mental illnesses [and] optimize NIMH’s clinical trials portfolio toward achieving personalized and preemptive interventions” (
5). Developing a personalized intervention, however, requires an understanding of the factors that make outcomes individually determined, and the NAMHC report appears to have elucidated the need to more selectively identify treatment targets. This emphasis on target engagement, borrowed from experimental medicine and later referred to as an experimental therapeutics approach, has been illustrated through mechanisms of dissemination, including clinical trials funding (
6) and blog posts (
7).
Application of the experimental therapeutics approach must satisfy two requirements. First, it must identify the specific targets that are engaged by an intervention—the structures, processes, or phenomena (cognitive, behavioral, affective, social—not just neurobiological) that are purportedly affected by the intervention and toward which the intervention is directed. Whether the target was engaged is foundational; target engagement will dictate whether a study can determine how and through what mechanisms the various intervention-induced effects influence the pathophysiology of the disease (
6,
8). Second, it must promote a deeper understanding of such pathophysiologies of disease by elaborating the action of the intervention (i.e., what happens after the intervention hits the target, the downstream processes that are stimulated, the second- and third-order effects, how these various effects create change in the outcome, and how such a cascade of effects contributes to understanding of pathophysiology and recovery. These targets and mechanisms are likely to differ across and within populations, requiring subgroup analyses to elucidate treatment effects. Furthermore, individual components of multicomponent interventions—typical in the human services—will have differential effects. With such an approach, a better understanding can emerge of how interventions work, through which mechanisms they work, and for which subgroups they might best work, leading to a more refined science of interventions (
6,
9,
10).
Many elements of an experimental therapeutics approach resemble program evaluation. The logic model for program evaluation developed by the Centers for Disease Control and Prevention (CDC) emphasizes the connections between programmatic outputs and anticipated outcomes (i.e., the “what”) (
11). Importantly, mediators affect relationships between outputs and outcomes (
12). Mediators within logic models, articulated within broader mechanisms or theories of change, are analogous to intervention targets. From a program evaluation perspective, therefore, in an experimental therapeutics approach, these mediators are the foci or targets of interventions, and the goal is to determine the extent to which changes in mediators account for changes in outcomes. Manipulation of mediators is central to the experimental therapeutics approach, inviting refinements to the science of interventions. In a 2015 report, a panel from the National Academies of Sciences, Engineering, and Medicine also called for better elucidation of key elements of psychosocial treatment effectiveness (
13). The report distinguishes between “nonspecific” elements—such as a therapeutic alliance, which is common to all psychosocial interventions—and “specific” elements—the intervention’s putative mechanisms of action. These latter elements are the targets of an experimental therapeutics approach. The science of psychosocial interventions can be refined by explicitly naming these targets, creating a tighter link between intervention components and these targets, and elaborating the effects of the intervention after target engagement.
Such a refinement of the science of interventions is particularly important in human services settings. Since Faris and Dunham’s seminal work in 1939 showed that residents of poorer neighborhoods in Chicago had elevated rates of mental disorder (
14), the association of material poverty with both higher risk of developing mental disorders and with poorer outcomes among those with mental disorders has become well established (
15–
17). Service-related variables have a key positive impact on mental health outcomes (
16), and social workers constitute the dominant mental health workforce today (
18). The majority of individuals living with serious mental health conditions receive services within “safety-net” settings in the community, such as child welfare (
19) or corresponding police and mental health programs (
20). Consequently, it is critical to focus on mechanisms of change in these potentially transformative sites that provide service initiation and access to some of our nation’s most vulnerable populations.
In considering an application of experimental therapeutics to human services settings, this article proposes that the core principles do not need to change but that one modification is perhaps necessary. That is, the targets that are engaged will almost never be biological and may not always be cognitive, affective, or even purely behavioral. Instead, the targets are likely to be social or interpersonal. Consider the goal of a housing intervention designed to ensure that participants secure stable housing (
21). Target engagement that will result in that outcome will need to focus on, for example, the ability to negotiate relationships with property owners, superintendents, and neighbors (an interpersonal behavioral target that encompasses independent living skills) (
21). Housing interventionists need to help clients develop the skills needed to prevent them from losing their housing once they have it, such as how to manage friends who want to stay with them, to maintain suitable housekeeping, and to avoid breaking rules, all of which can lead to being deemed undesirable by housing authorities and ultimately result in eviction (
22). In this case, an efficacious intervention is one that engages a behavioral or interpersonal target that may be called “the ability to live with others.” Successful engagement with this target may lead to a proximal outcome of stable housing, which might then lead to the distal outcome of enhanced recovery from mental disorder for precariously housed individuals with such conditions.
Example of an Experimental Therapeutics Approach to an Employment Intervention
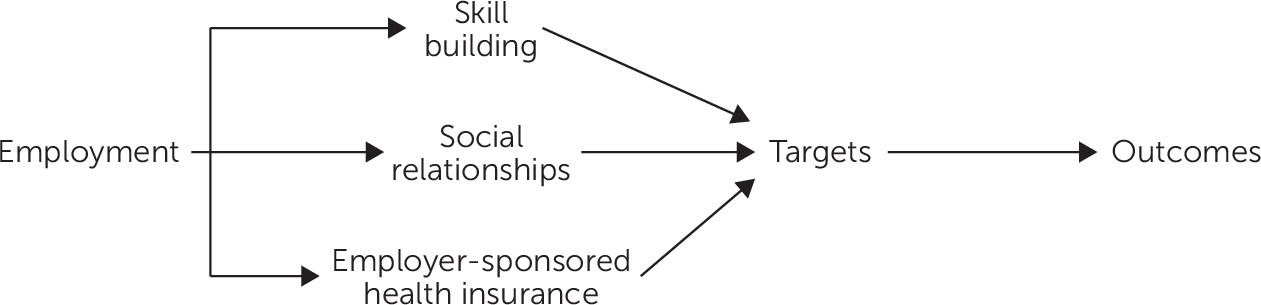
Building on the housing intervention example, we consider first the common components of an employment intervention (
Figure 1). Research on supported employment—in particular individualized placement and support (IPS), vocational rehabilitation, and clubhouse models (
23,
24)—for individuals with mental disorders has been extensive. To date, research has largely focused on the efficacy of the model (
25) and on fidelity development (
26)—not on examining mechanisms of change or on how IPS works (i.e., change in cognitive expectancies, mood, knowledge of the culture of work, or all of the above) (
27). It is important to recognize that duration and intensity of the intervention are not mechanisms of action. They are characteristics of the intervention, or conditions necessary for treatment effectiveness. As such they are normally moderators of effectiveness. These characteristics or conditions are often emphasized in treatment manuals because they are critical to the attainment of desirable outcomes. By themselves, however, they are not targets of an experimental therapeutics approach, forming instead the penumbra of the intervention.
These employment programs, however, typically have common components: for example, skill building, social relationships, and examination of prior work experiences (
28). Our conceptualization of an intervention designed to acquire and sustain paid employment consists of three components: skill building, the development of social relationships, and the attainment of employer-sponsored health insurance (
Figure 1). Skill building involves acquiring behavioral and cognitive competencies necessary to secure employment, such as developing a resume and learning to interview. Social relationships involve the development of supportive relationships with an employment specialist and with vocational rehabilitation counselors. Finally, many forms of employment are associated with employer-sponsored health insurance, which safeguards the health of individuals and provides coverage for the management of conditions (such as substance abuse) that can jeopardize continued employment. These components clearly interact with one another but represent three distinct core areas that most supported employment interventions address.
Identification of these components is a necessary but insufficient step to designate targets and mechanisms in accord with the experimental therapeutics approach. Researchers now need to answer, What are the targets that each of these intervention components are designed to engage and how does engagement with each target produce the ultimate outcome of employment acquisition and retention? For brevity, this rest of this article focuses only on social relationships as well as insurance coverage.
Component A: Targets of Social Relationships
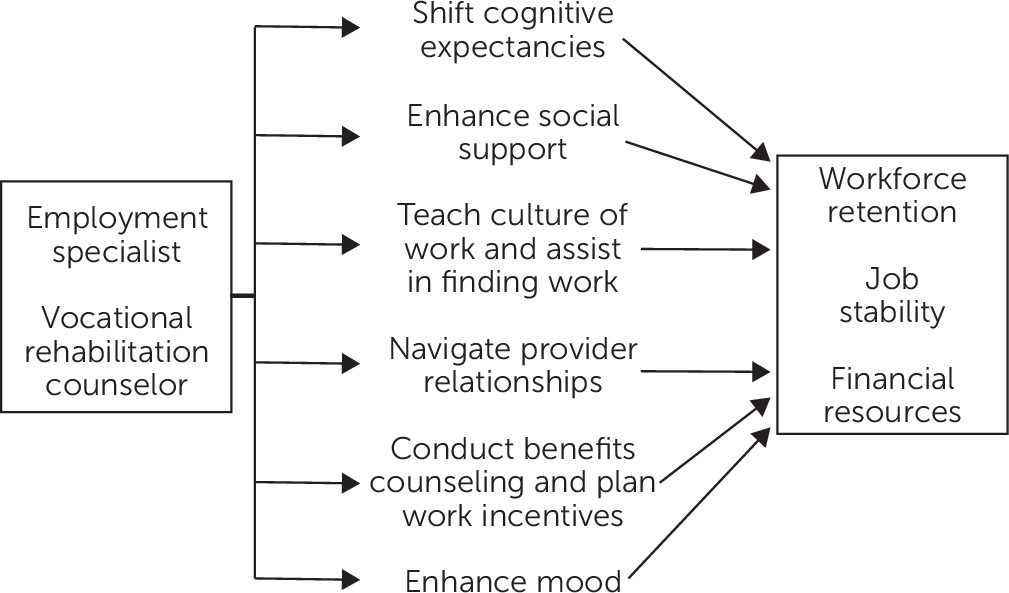
To secure and sustain employment, a person needs to be adept at managing social relationships and attaining “soft skills,” including understanding the culture of work, maintaining strong work ethic, communicating effectively, and conveying a positive (or at least neutral) affect while on the job. Most employment interventions focus on developing these skills through a supportive relationship with an employment specialist or job coach and/or through vocational rehabilitation counseling (
Figure 2).
The experimental therapeutics approach encourages scientists to first conduct formative research to develop systematic knowledge of how each specific component of the employment intervention works. Once the hypothesized targets are identified, scientists can measure each for change and whether any change in those targets leads to change in the ultimate outcome—employment. The approach focuses on uncovering how the supportive relationship component, a relationship with an employment specialist, produces change in the active targets of that component.
Common targets that are engaged through the employment specialist component include improvement in general mental health, enhanced mood, and reduced stress via social support and coordination of needed mental health services; knowledge of the workplace culture and of typical interactions; and new performance skills on the job (
29). The experimental therapeutics approach requires that the field test these paths to illustrate empirically whether the employment specialist hits those targets of change and, further, whether those mechanisms are the same for different groups of clients. For example, for young adults, the employment specialist component may have its greatest effect through education about the workplace culture and expectations. However, for middle-aged or older adults, the model may have greater impact through follow-along supports. Of late, promising data have emerged supporting models that focus on providing youths with employment specialists, vocational coaches, or both (
30). These models, however, have yet to uncover how the interventions create employment change. Investigating this question using experimental therapeutics is the next step in developing proven treatments for individuals with serious mental illnesses who require stable employment on their journey toward recovery.
Component B: Targets of Health Insurance Coverage
Many types of paid employment come with employer-sponsored health insurance coverage, which is the dominant form of health insurance for Americans today. The health services literature (
31,
32) offers robust findings that the acquisition of health insurance ensures access to services and thereby facilitates positive health outcomes. But how does the presence of insurance produce these effects?
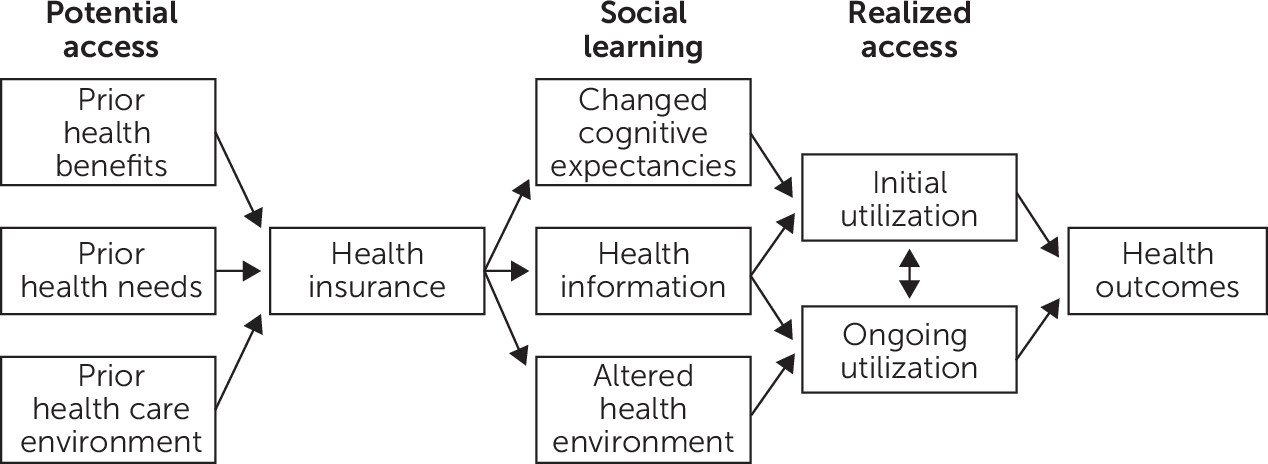
Figure 3 outlines one possible sequence of events. According to this model, individuals gain access to health insurance coverage because of changes in social learning. There are three putative targets of action in this model: changed cognitive expectancies, enhanced health information, and altered health environment.
First, possessing insurance changes expectancies and, thus, behavior (
33). Some of this change in expectancies is negative (e.g., only half of non-Hispanic black patients in one study report trusting their health insurance plan) (
34). Even political discourse about insurance can affect attitudes. For example, between 1988 and 1992, American National Election Studies data suggested increased support for government-funded national insurance. But between 1992 and 1994 (the Clinton administration’s Health Security Act was introduced in the fall of 1993) this support eroded dramatically as support for expanded private insurance coverage increased (
35). But regardless of the valence and antecedents of such changes in attitudes, the possession of insurance changes choice sets (
36), which are cognitive mechanisms that may lead to health service utilization. What does this mean for intervention development? One possible next step could be the development of an intervention that specifically targets such expectancies and attempts to change their valence from negative to positive.
Second, the act of securing health insurance is an informational phenomenon, where the person in possession of insurance for the first time is forced to learn about it and its uses. In this sense, acquiring insurance produces effects much like those of acquiring any other good; the acquisition of a camera, for instance, may lead its owners to read the manual to understand how to use it. Knowledge about health insurance carries implications that vary according to demographic characteristics. Mothers’ ability to understand printed insurance material, for example, is critical to the dental health of low-income Latino children (
37). Conversely, highly educated and wealthy women are overrepresented in the population seeking in vitro fertilization services in Massachusetts, where these services are covered for all residents (
38). Each of these examples illustrate the final effects of differences in health information, produced either by coverage status (in the case of mothers of low-income Latino children) or a new set of covered benefits (in the case of women in Massachusetts). In fact, the phenomenon of moral hazard after the acquisition of insurance is fundamentally a result of learning (
39), in that individuals with unmet needs recognize that they now have a way to seek services that meet those needs. This is why, for example, patients who are told that their doctor would not accept their insurance spend more time seeking out health information on the Internet (
40); it is probable that at least part of their behavior is motivated by their need to learn about the utility of their new insurance and to overcome its limitations.
This learning also operates in the reverse direction. Residents of villages in rural India eschew health insurance even when it is offered to them at affordable premiums (
41). They report doing so because they have financial means to pay out of pocket for costs incurred and have a fallback option in the free services available to them in government primary health centers, even though the care received within the centers is generally of poor quality. Whatever one may think of the wisdom of their decision, given the catastrophic risks of medical impoverishment in India (
42), the availability of insurance as an option has resulted in an informed decision regarding its role in their care.
Third, the possession of health insurance may alter a newly insured individual’s health environment, channeling use away from emergency departments (presumably the prior pattern of seeking care) into primary care. Such an effect has been demonstrated most recently in evaluations of Oregon’s Medicaid lottery program (
43), as well as in older studies (
44). Children with histories of abuse and neglect acquire Medicaid as a result of categorical eligibility when placed into foster care (
44). This eligibility is one mechanism through which entry into the child welfare system acts as a conduit to needed services (
45). These examples all demonstrate that insurance acquisition changes the environmental boundaries of health service use, introducing new avenues and sources of care denied to those who lack coverage.
These three mechanisms of action need not be the “right” ones—that determination is, after all, the motivation for further research. That they are plausible is sufficient. Clearly, several other intervening factors may play a role; hence,
Figure 3 is illustrative, not exhaustive. It is also not necessary that these intervening factors be independent. The effects of insurance on service use are part of a complex phenomenon involving prior experience, transportation barriers, competing needs, sources of care, client preference, institutionalized racism, and myriad other factors. The point is that the acquisition of insurance produces second-order effects, all of which serve to elucidate possible mechanisms through which coverage might translate into use.
Implications and Challenges of a “Science of Mechanisms”
Shifting to a “science of mechanisms” has several implications and challenges for intervention development and methodological advancement in the health and human services fields.
The primary implication is for the development of target-focused intervention. For example, one decomposition of “the Bridge” peer health navigator intervention involved the navigator providing health education and wellness (i.e., “consumer awareness”) assessments and finding information regarding the insurance and other benefits possessed by the client (
46). Another element of the peer navigator’s role, “scanning environmental resources,” was to find providers and health clinics that could serve the client. As this example illustrates, health services researchers are already performing mechanism-based research that engages targets—they are just not clearly conceptualizing and communicating their research as a science of mechanisms. Consequently, few are empirically testing based on theory whether there is support for these hypothesized mechanisms (i.e., the mediational chains of the effects of an intervention).
A first implication, therefore, may be translational. Conceptualizing the work as a science of mechanisms may lead to further avenues for research. What do empirical data reveal about which of these hypothesized mediating targets are changing? Are all of these intervention components equally effective in securing access to services? If not, are there other program components that a health navigator might deliver or elements that he or she can stop delivering? Refocusing on mechanisms can help address such questions of implementation, deimplementation, and questions about task-shifting. This approach may lead scholars to develop theory with hypothesized a priori mechanisms of action, which are then tested in vivo, in much the same way that physiologists identify a possible pathway relevant to pathophysiology of disease during drug development, and pharmacologists develop and test a drug that affects that pathway.
Second, translation may be a reasonable recommendation when the targets of an intervention are well known and are already being studied. In many cases, however, services researchers may not know how their psychosocial interventions are efficacious and may lack knowledge about intervention targets. In such instances, theory may guide them to develop and evaluate interventions. In “the Bridge” example cited above, treatment targets are inherent within interventions, and theory can be used a posteriori to refine the intervention’s mechanism of action. The earlier discussion of targets of health insurance presents a similar situation. However, in other cases, there may be no targets available. In such instances, theory may need to be used a priori to identify putative mechanisms of action that can then be tested. Thankfully, the field of services research is well acquainted with theory, and many services researchers come from theory-laden disciplines, such as economics and sociology. But an explicit extension of disciplinary frameworks to the theory of services research—as has been done, for example, in theories of access (
47), quality (
48), and policy (
49)—is necessary to further the science of psychosocial interventions.
Third, how can theory lead to empirical studies when understanding of targets is inchoate? It is possible (indeed, even likely) that researchers do not know how many programs and interventions in the human services space actually work. In these cases, qualitative methods are essential to conduct formative research aimed at uncovering processes of interventions that have yet to be identified and to develop initial hypotheses of how new and innovative interventions might work. Qualitative research in this context is necessary and can be designed to uncover putative targets for interventions. For example, researchers may conduct interviews with service users about their perspectives on how the intervention assisted them in their lives and with providers about their observations of how the intervention served those living with mental illness. Such formative work can then yield to measurement studies that develop indices of potential mechanisms of change (e.g., hope). Once mechanisms are understood, services researchers will need to conduct psychometric studies to develop valid and reliable measures of these targets. The identification and measurement of targets is critical to psychosocial intervention development. Training of services investigators in such methods will be necessary to enhance the rigor of services research studies.
Fourth, a science of mechanisms can also lead to the repurposing of existing interventions toward novel outcomes. Among the strongest effects of “the Bridge” program (effect size of 0.91) in a randomized control evaluation was a reduction in bodily pain and consequent limitations in functioning between the experimental and control groups (
50). However, none of the program components appear to be uniquely focused on pain management. If the effects are replicated, key components of the program might be worth deploying for patients with pain conditions. Such a reconceptualization followed by repurposing has the potential to strengthen pain interventions and enhance understanding of therapeutic commonalities that may engage novel targets. This thinking is central to the research domain criteria framework (
51) but has been insufficiently applied to services research. Just as there are symptoms and neurobiological processes that are “transdiagnostic,” there are perhaps components within services interventions that are “transoutcomes.” Identifying and elaborating such program components are outcomes of a science of mechanisms.
Fifth, an important need of a science of mechanisms in services research is to further analyses of observational studies. Thus far, much of the focus of an experimental therapeutics approach has been on research design, such as sequential multiple assignment randomized trial (SMART) designs (
52). But many services researchers conduct observational studies, where such design innovations cannot be deployed. Hence, advances in analytic approaches, such as causal mediation analysis (
53,
54), are necessary to help enhance the rigor of a science of mechanisms in the health and human services fields. Other services researchers conduct experimental studies using smaller sample sizes. In these instances, careful attention to power is needed to strengthen causal inference. Some methodologists suggest that small-N studies are enough to make causal inferences, advancing strategies such as nominal comparison, ordinal comparison, and within-case analysis (
55). This thinking may not be fully aligned with orthodox causal inference theory based on a potential outcomes framework, but the larger point is clear: services scholars should deploy methods that enhance causal inference given the constraints of their science.
Sixth, a deeper understanding of targets and their effects may enhance the science of treatment evaluation. Intervention targets lie on the pathways between treatment (or programmatic outputs) and outcomes (i.e., they are mediators). Currently, there is no requirement that logic models specify moderators or mediators, and scholars have called for greater inclusion of these factors within evaluation research and practice (
56). Adoption of an experimental therapeutics framework will require evaluators, logic model developers, and program theorists to further elaborate on exactly how program outputs translate into outcomes and how outputs can be manipulated to further strengthen outcomes.