In 2017, New Mexico had the 17th highest drug overdose death rate and 21st highest opioid overdose death rate in the nation—both higher than the respective rates nationwide (
1). To address the opioid use crisis, there has been increasing attention on promoting medication-assisted treatment (MAT) using opioid agonist medications (e.g., buprenorphine) in combination with psychosocial treatments and recovery services (
2). Currently, physicians (medical doctors and doctors of osteopathic medicine) and advanced practice providers (
3) can obtain a waiver and licensure to implement MAT in primary care, thereby helping to expand accessibility to large segments of the population (
4).
Despite evidence supporting the efficacy of MAT, uptake of the treatment in primary care settings has been disappointingly slow (
5). Barriers to the adoption of MAT include lack of provider knowledge, negative attitudes or stigma about prescribing “opioid replacement” medications to patients with opioid use disorders, and policy and financial constraints related to reimbursement (
6,
7). Currently, there is a severe national shortage—especially in rural areas (
8)—of physicians who prescribe buprenorphine. In New Mexico, a predominantly rural state, 629 practitioners held a Drug Addiction Treatment Act (DATA) waiver through 2018; however, only 180 of them had seen at least 10 patients (
9).
The ECHO (Extension for Community Healthcare Outcomes) practice model aims to expand access to MAT in rural primary care settings. This model, developed at the University of New Mexico by Sanjeev Arora, combines didactic and interactive case-based learning through a videoconferencing platform. The ECHO model overcomes communication barriers caused by geographic distance by assembling content experts at a “hub” site to reach participants at remote “spoke” locations. First used to improve patient outcomes in the treatment of hepatitis C in rural New Mexico, this model has been widely lauded as an effective approach to helping providers implement a novel treatment in rural areas that sometimes lack other cost- and time-efficient ways to access training and support (
10,
11). However, important gaps exist in our understanding of the implementation dynamics associated with Project ECHO (
12). This brief report describes findings from a study of barriers and facilitators to participation in ECHO sessions among rural primary care providers.
Methods
This ongoing study featured the delivery of 12-session training cycles through Project ECHO aimed at providing training and support for rural primary care providers to expand MAT for opioid use disorder. Eligible sites must have had at least one potential prescriber for buprenorphine (e.g., physician or advanced practice provider) who did not have more than 30 patients prescribed buprenorphine during the preceding 6 months. Data collection was conducted from December 2017 to December 2018. All participants involved in this study provided informed consent, and research activities were approved by the University of New Mexico Institutional Review Board.
Recruitment efforts were extensive and multipronged, using a variety of statewide sources, including the New Mexico Primary Care Association, other state opioid treatment initiatives, and email LISTSERVs through the state Behavioral Health Services Division and Department of Health. In addition, the research team identified primary care clinics in New Mexico counties with the highest rates of opioid use disorder. Research team staff also directly contacted clinic leadership, including medical directors, managers, and other available staff, to introduce the study and request an email address to send recruitment materials. The last phase of recruitment efforts involved sending recruitment materials to all clinics via fax.
The research team developed a 12-session curriculum designed to provide education, support, and consultation to help start, expand, and sustain MAT for opioid use disorder in rural primary care. Specifically, session content covered key components of implementation in primary care practice, such as DATA waiver training, prescribing considerations, psychosocial supportive models, counseling techniques, and selection and use of opioid screening instruments. These sessions were presented on a one-hour-weekly basis (from noon to 1 p.m.) for 12 consecutive weeks. On the basis of the ECHO model, participants were encouraged to present deidentified patient cases to enhance skill building and self-efficacy in the use of MAT.
Data collection efforts were designed to assess primary features associated with participation and to identify provider perspectives on potential barriers and facilitators to MAT implementation using this model. At each session, the research team documented attendance and the number of participants who presented patient cases. Each participant was contacted on a monthly basis during the 12-week cycle to confirm session attendance and catalog reasons for absences. After the completion of the cycle, all participants were invited to a qualitative interview, conducted either in person or by phone. The interview guide featured questions about participants’ overall attendance, challenges in participation, scheduling issues (e.g., length of sessions, time of day), and perspectives on barriers to implementing MAT. Participants received either continuing medical education or continuing education units, as requested, as well as a $40 merchandise card for their participation in the session attendance survey and qualitative interview.
Attendance logs were created in an Excel spreadsheet to record session participation and reasons for absences. Descriptive summaries were then generated to examine attendance patterns. The qualitative interviews were transcribed and analyzed using NVivo, a qualitative data analysis software program. Two members of the research team reviewed the transcripts, developed a coding template, and ran queries to further assess implementation issues associated with participation or with participants’ impressions of the ECHO sessions.
Results
A total of 24 participants from 13 primary care clinics were enrolled. Of the represented clinics, 11 were part of federally qualified health center systems, one was a private practice, and one was a hospital-based primary care clinic. Of the 24 participants, 13 were prescribers, and 11 were practice staff. A majority (63%, N=15) were female, and race-ethnicity composition was reported as follows: 54% (N=13) non-Hispanic white, 25% (N=6) Hispanic, 8% (N=2) black, 4% (N=1) American Indian, and 8% (N=2) “other.”
The pattern of participation and attendance in ECHO sessions was widely variable.
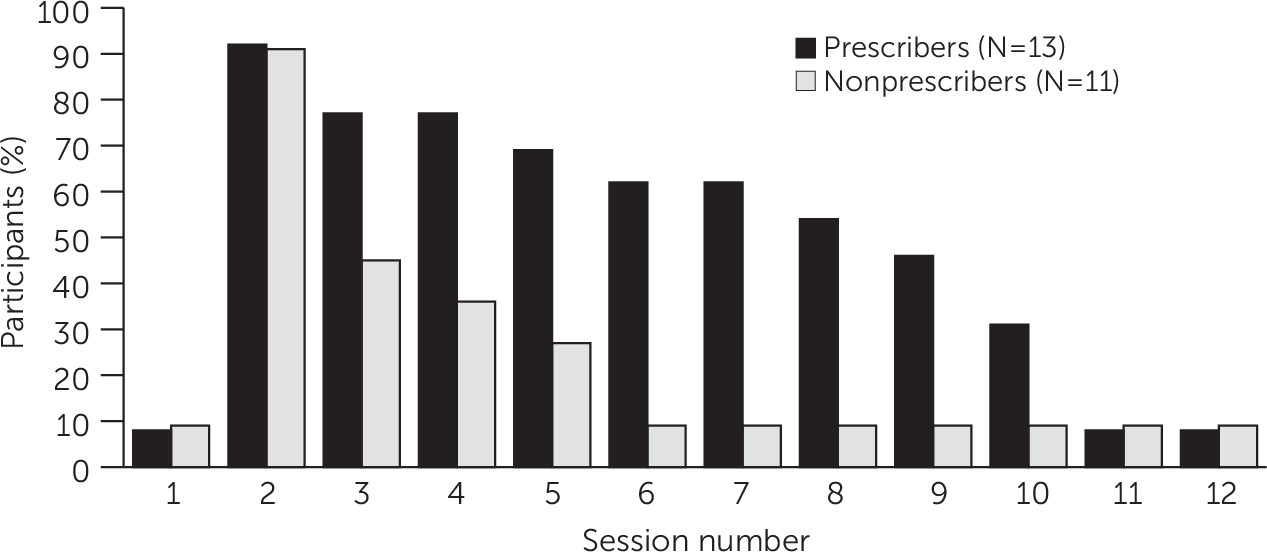
Figure 1 depicts attendance in each of the 12 ECHO sessions by participant type. Overall, the mean±SD rate of attendance was 4.4±3.7 participants per session with a range from zero to 11. Prescribers attended 5.9±3.6 sessions, and nonprescribers attended 2.6±3.1 sessions. Participants presented eight patient cases throughout the cycle, out of a possible 48 sessions. In the absence of a participant-led case, expert panel members presented impromptu cases derived from their clinical experience to ensure interactive discussion and case-based learning.
In the qualitative interview data, providers and staff reported positive impressions of the ECHO sessions. Specifically, participants indicated three aspects of the ECHO model that led to this favorable review. First, almost all interviewees highlighted the ease of access to the ECHO sessions. Participants could access the sessions from a chosen location in the clinic (or elsewhere) and found the interface to be convenient. As one provider stated, “I like it online because there’s no travel involved. . . . I can easily jump out and jump back in as issues come up around the clinic.” Second, providers and staff expressed support for the opportunity to engage with content experts through the didactic and interactive case presentations. Last, participants emphasized the value-added effects of participating in the ECHO sessions. That is, in clinics where both providers and staff routinely attended sessions, participants reported that this involvement served as a catalyst to advance dialogue and reflection about MAT integration in the practice setting.
The most notable engagement challenge reported by participants, not surprisingly, was the burden of competing demands on time and availability. While virtually all providers and staff indicated that the one-hour ECHO session is an appropriate duration, they consistently cited the need to prioritize patient care over other activities. The other primary barrier participants reported pertains to the degree to which clinic leadership supported devoting resources to starting or expanding MAT, including time for attending the ECHO sessions. Providers consistently noted that there must be willingness from leadership to approve time spent participating in the ECHO sessions and to integrate MAT in the clinic. As one provider stated in reference to meeting the training and prescription requirements for MAT, “You can give somebody a license, but if you don’t have the support to do what it is you need to do, it makes it difficult.” Finally, as indicated in
Figure 1, nonprescribers averaged lower attendance than prescribers, which was attributable primarily to the relatively greater focus on MAT training elements geared to prescribers.
Participants also discussed potential strategies to promote attendance in the ECHO sessions. Several providers and staff requested that the ECHO sessions be recorded in order to facilitate asynchronous access. Participants expressed limited confidence that changing the time the sessions convened would increase regular attendance. However, the consensus among respondents was that the most important facilitators for session attendance relate to organizational drivers, such as support from leadership and a shared desire to build a learning community whereby providers learn from each other regarding different models of MAT delivery.
Discussion
We systematically documented the attendance and engagement of primary care providers in a series of Project ECHO telementoring sessions aimed at providing training and support for implementation of MAT. Despite the prevalence and burden of opioid use disorder in New Mexico, we faced significant challenges recruiting and retaining participants throughout the 12-week training cycles. Provider attendance was irregular, and the majority participated in fewer than half the sessions. Interestingly, the qualitative findings indicate that providers valued the didactic and interactive nature of the sessions but identified system-level constraints that limited engagement.
We anticipated that common competing demands—volume of patient care, challenge of identifying a consistent time to participate in training, and lack of time—would limit enrollment. Providers who ultimately enrolled in the study identified a clear interest and desire to either begin delivering MAT to patients with opioid use disorders or to add more patients by enhancing their skills. However, several of the participants with lower attendance noted the challenge of insufficient practice-level support from leadership to take on MAT. This lack of support appeared to be the most prominent “upstream” determinant, because providers in clinics where MAT is a priority were able to more easily justify time spent attending sessions and to perceive that attendance was valuable.
ECHO implementation may also be hindered by the difficulty of identifying a single window of time during the week that is suitable for all attendees to convene. Several participants suggested recording the sessions and allowing for asynchronous review. Although archiving sessions would likely enhance opportunities to view the didactic presentations when convenient, the conundrum is that robust ECHO sessions depend on interactions whereby participants present cases and learn from each other during discussion.
Conclusions
Use of ECHO interventions to address critical primary care training challenges has the potential to overcome barriers such as geographic distance between trainers and care providers and shortages of content experts in order to extend evidence-based practices such as MAT. Prior research has broadly characterized implementation barriers to changes in primary care practice (
13). However, there has been little documentation of evaluation efforts aimed at understanding barriers to participation that may influence more distal outcomes of concern, such as achieving a higher number of rural primary care providers prescribing MAT and patient adherence to treatment. Strategies to enhance engagement in models such as ECHO may require more “upstream” policy-level approaches. For example, in spring 2019, legislation was introduced to the U.S. Senate aimed at increasing access to health care services in rural areas by expanding the use of technology-based collaborative learning and capacity-building models such as ECHO. Such legislation holds potential to provide outcomes-related reimbursement in order to promote best practices and participation in ECHO (
14).
This brief report identifies key practice system challenges that may directly affect engagement in ECHO. As researchers use this important infrastructure, it will be important to assess engagement during formative assessments, drawing from implementation science frameworks to maximize benefits.
Acknowledgments
The authors acknowledge Rana S. Al Khafaji for her contributions to the study.