Recent global efforts to reduce the treatment gap for persons with mental, neurological, and substance use disorders in low- and middle-income countries (LMICs) have focused on supply-side factors, i.e., increasing availability of primary care providers trained in mental health care (
1,
2). However, even when availability of services has increased, there is often low utilization of mental health services because of demand-side factors, i.e., factors that determine the level of uptake of care. These factors include cost of services, social and cultural norms, and knowledge of available services (
3–
6).
Gaps in help seeking in LMICs are similar to those in high-resource settings. For example, in both the United States and LMICs, there is low help seeking for mental health conditions among members of racial and ethnic minority groups (
7), members of the military and veterans (
8,
9), rural populations (
10), and the general public (
11,
12). To bridge the access gap and increase mental health treatment coverage, supply-side efforts will need to be combined with strategies that increase help seeking and demand for care (
13). Initiatives that have demonstrated success in LMICs may set the stage for comparable strategies in high-resource settings.
Use of the Community Informant Detection Tool (CIDT) is an innovative strategy to increase help seeking. The CIDT was developed for use in a district-based mental health care service in Nepal (
14), which was part of a program to evaluate the integration of mental health into primary health care in five LMICs (
15), including Nepal. The CIDT is intended for use by people who are respected and trusted in the community (
16). Prior to using the CIDT, these trusted individuals receive 2 days of training in community engagement and implementation of the tool. Persons trained in CIDT use the tool in their daily work or interactions, through a process of prototype recognition of people in their surroundings. The method has two strengths: it facilitates efforts to reach the most vulnerable and most isolated people in a community, and it provides a low-cost alternative to universal screening in primary health care. Several risks are associated with universal screening for mental, neurological, and substance use disorders in primary care, including the extra time and related costs associated with screening by primary care providers, the diverse range of screening tools required, and the risks associated with false positives, including the possibility that services would be flooded with clients.
Methods
Setting
This study was implemented in Chitwan, a district in southern Nepal, as part of the multiyear Program for Improving Mental Health Care (PRIME). The program aimed to implement and evaluate a district-level mental health care plan (MHCP), including integration of the World Health Organization’s (WHO) mental health Gap Action Program Intervention Guide (mhGAP-IG) in primary health care (
14,
15). PRIME includes supply-side improvements, specifically the training of health care workers in all primary care facilities to deliver mental health services using the mhGAP-IG (
14).
Proactive Case Finding Strategy: The CIDT
The CIDT is a method of proactive case detection that enables lay people in the community to assist in the identification of people with potential depression, psychosis, alcohol use disorder, and epilepsy (see Figure S1 in online supplement). The CIDT consists of context-sensitive vignettes describing prototypes of depression, psychosis, alcohol use disorder, and epilepsy, combined with pictures that are easy to understand by low-literacy populations; a question that asks the community informant to gauge the extent to which a member of the community matches a prototype; and two additional questions about impaired daily functioning and perceived need for support for an identified individual.
If there is significant prototype matching and a positive response to at least one of the two additional questions, the community informant encourages the person to seek help in the health facility where mental health services are being offered (
18). Asking the two additional questions (about impairment and perceived need for support) and discussing care seeking with the individual or family member take approximately 10 to 15 minutes.
A previous study has demonstrated that when lay community members use the CIDT for depression, the accuracy of detection is good (positive predictive value of 0.64) (
18), and the psychometric properties are stronger than those of the Patient Health Questionnaire–9 (PHQ-9) (
19). A subsequent study demonstrated that among those detected with the CIDT, two-thirds (67%) accessed services because of that detection (
20). These encouraging results prompted us to compare help seeking between primary care settings in regions that were randomly assigned to standard treatment engagement or to use of the CIDT.
The CIDT was developed within the context of the PRIME mental health care package in Nepal to increase help seeking and was implemented by female community health volunteers. Female community health volunteers are an existing cadre within Nepal’s health care system and are present within each village; these women are often the first point of contact for people needing health services (
21). They are residents of the village where they work, and they deliver family planning and maternal and child health services. Within the mental health care package, community health volunteers were also responsible for conducting home-based care for people receiving mental health care, a feature that is intended to promote treatment adherence.
Study Design
We conducted an RCT comparing utilization of mental health services at primary health care facilities where the CIDT was introduced and facilities that used standard practices (control condition). Female community health volunteers in both arms received training of equal duration in awareness-raising activities. This 2-day curriculum included basic information about mental health, stigma, availability of mental health services in primary care, and self-referral. In the CIDT arm, the community health volunteers were taught how to make proactive community referrals (see Table S1 in the online supplement for standard curricula and modifications for the CIDT arm). During the training on using the CIDT, time was spent addressing the potential risks associated with using this approach (e.g., stigmatizing of identified individuals, issues of confidentiality). In this regard, it is important to mention that the community health volunteers are a well-respected group of people in the community with prior health work experience and an ethos for community service. Bimonthly supervision was conducted for all community health volunteers to oversee the quality of work as well as to discuss challenges and possible ways to overcome them. Supervision included monitoring of the use of CIDT.
This study was implemented in 24 health facilities (catchment population: intervention arm, N=155,114; control arm, N=131,724) where the PRIME package was being rolled out. The study was a pragmatic RCT because it was embedded within routine practice. All health facilities participating in the PRIME scale-up phase with planned integration of mental health services were eligible, excluding only health facilities located in the same village (because of risk of contamination) and urban centers with overlapping catchment areas. (Table S2 in the online supplement contains descriptions of the health facilities.)
Randomization
The eligible health facilities were randomly assigned to the two study arms in a 1:1 ratio. After randomization, community health volunteers attached to the randomized health facilities received basic training in community outreach for mental health services (community awareness raising) (control group condition), or the same training in community outreach combined with training in using the CIDT. Randomization sequence generation was done by using SPSS (
22).
Ethical Conduct
Ethics approval for this study was obtained on April 7, 2016, from the Nepal Health Research Council (no. 1620).
Outcome and Analysis
We assessed the number of patients with depression, psychosis, alcohol use disorder, and epilepsy as well as other mental, neurological, and substance use disorders who were registered in the health facilities’ routine patient data collection system. Within each health facility, there is an outpatient department register booklet specifically for documenting care of patients with depression, psychosis, alcohol use disorder, and epilepsy. Primary care providers can also register patients with other mental, neurological, and substance use disorders. This register was provided to all health facilities through PRIME and was routinely reviewed for completion by clinic supervisors and PRIME research staff. Registration reflects patients who have started treatment for a mental, neurological, or substance use disorder.
For the baseline, we collected the total number of patients with depression, psychosis, alcohol use disorder, and epilepsy recorded over a period of 6 months prior to the training of community health volunteers and prior to the implementation of the MHCP. Baseline data were collected to assess comparability between the groups in number of registered patients with depression, psychosis, alcohol use disorder, and epilepsy before the start of the program. For the follow-up, we collected the total number of patients for whom treatment was recorded during the 6 months after the training of community health volunteers and the start of MHCP service provision.
Given the small sample size (12 facilities in each arm), we used a nonparametric test (Mann-Whitney U test) to compare the median number of patients with depression, psychosis, alcohol use disorder, and epilepsy at each health facility, with study arm as the primary outcome. In addition, we compared the number of patients at each health facility relative to the facility’s population catchment (presented as per 10,000 population catchment) and relative to the number of trained community health volunteers per facility. Data were collected between July 2016 and June 2017. (The trial protocol registration is available through ISRCTN,
http://www.isrctn.com/ISRCTN28071919.)
Results
Of the 24 eligible health facilities in the Chitwan district, 12 were randomly assigned to each arm (see Figure S2 in the
online supplement). A total of 105 community health volunteers were trained in the intervention arm, compared with 91 in the control arm (
Table 1). At baseline, only two patients with a mental disorder (depression) were registered, both in the intervention arm. Six months after the community health volunteers had been trained and after initiation of mental health care services, there was a rise in the number of patients with registered mental disorders in both study arms.
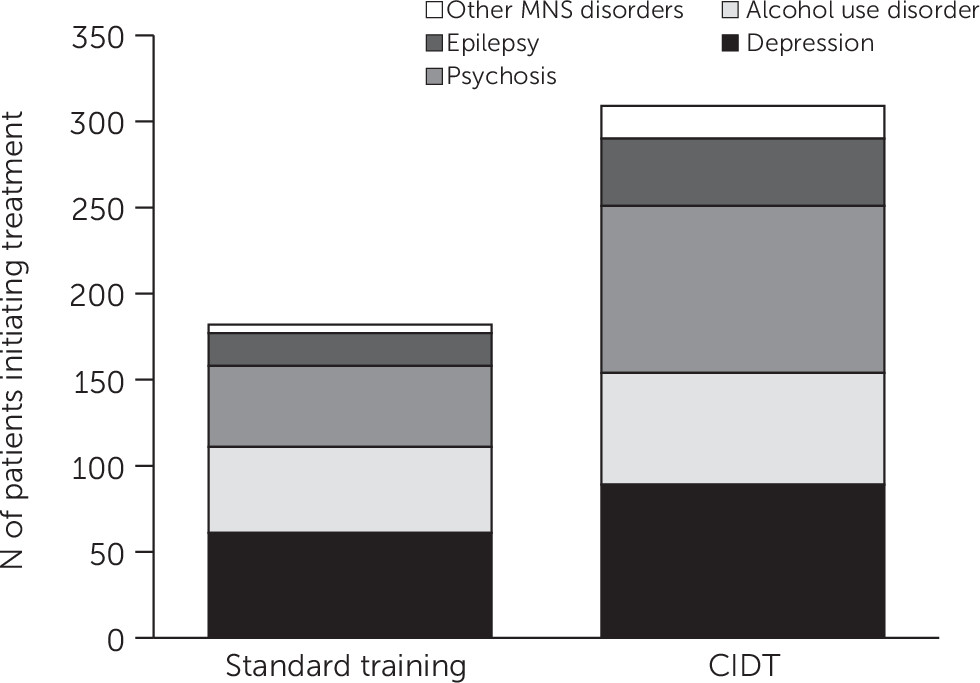
A total of 309 patients with mental, neurological, and substance use disorders were registered in the health facilities in which community health volunteers used the CIDT compared with 182 patients in facilities in the standard training arm (
Table 1). A Mann-Whitney U test indicated that the median number of patients who had received care for a mental, neurological, or substance use disorder was greater for health facilities with community health volunteers trained in the CIDT (median=23.50) than for health facilities with community health volunteers who received standard training (median=16.00) (U=36.50, p=0.04, r=0.42). This means that the median number of patients with depression, psychosis, alcohol use disorder, and epilepsy in facilities where CIDT training occurred was 46.9% greater than in facilities in the control arm. We did not find a significant difference between the number of patients registered by the treatment and control arms as a function of the number of community health volunteers trained per health facility. However, there was a significant relationship between the number of patients registered by the treatment and control arms as a function of the population catchment of the health facility (
Table 1).
Figure 1 provides a breakdown of the information in the mental health outpatient registry by disorder.
Discussion
With increased attention to reducing the treatment gap for people in need of mental health care, both supply- and demand-side factors should be considered (
13). Supply-side factors, for example, can be addressed by training primary care providers in the diagnosis and treatment of mental disorders. However, health systems may continue to face challenges in improving service access and utilization even after they have increased availability of care (
23). Demand-side factors refer to strategies that aim to improve service utilization, beyond increasing the availability of services. The CIDT was developed to facilitate identification of persons with potential depression, psychosis, alcohol use disorder, and epilepsy and their engagement with services. Such recognition of “illness behavior” at the community level is in line with tackling the first of five filters, or barriers, in Goldberg and Huxley’s (
24) pathways to psychiatric care model.
This study demonstrated that proactive community case detection using the CIDT led to an increase of nearly 50% in the number of people being initiated in care compared with community strategies relying only on raising awareness and self-referral. Previous studies have examined detection of persons with a mental disorder by community members and demonstrated that detection was accurate for approximately two-thirds of those detected (
18) and that approximately two-thirds of those detected sought help because of case detection (
20). This study provides evidence for the effectiveness of the CIDT as a strategy to increase relevant help seeking. This finding is particularly pertinent in contexts in which the challenges of routine screening for depression, psychosis, alcohol use disorder, and epilepsy in primary care settings remain unresolved (
25). In LMICs, where services are scarce and barriers to access abundant, facilitating help seeking may be especially important in reducing the treatment gap (
26).
The limitations of this study were mostly related to the pragmatic nature of the design. First, although we randomized assignment to study arms, regional differences between the facilities in the control and intervention arms may explain the between-group differences in service utilization. We conducted an analysis of service use on the basis of population catchment of each facility, and the differences between the control and study groups remained significant. However, when we analyzed whether the number of trained community health volunteers was associated with service use, the difference between study arms was not significant, although the absolute median number of patients per trained volunteer was higher in the intervention arm (2.6 patients) than in the control arm (1.9 patients). The lack of significance can be explained by one health facility that had only one female community health volunteer in the control arm (compared with 5–10 women for the other health facilities). A larger sample size of health facilities is needed to accurately assess differences in detection rates per community health volunteer trained.
Second, because we were dependent on the limited data from the routine health information system, we could not evaluate the impact of other possible predictors on service utilization (e.g., average distance to health facility, socioeconomic status of households, and quality of services). Future replication studies should take these variables into account. Third, we do not report whether the specific CIDT prototype matched the diagnosis made by the primary care provider. This information was reported in another CIDT sample (
18). Moreover, because the goal of CIDT is to encourage help seeking, the referral was considered successful even if the CIDT prototype identified by the community health volunteer did not match the diagnosis made by a primary care provider.
It is important to note that the outcome assessed in this study was dependent on the primary care providers’ diagnostic skills. It is possible that the results presented here are an underestimation of the true effect of the CIDT, if we take into account the rate of false negatives, i.e., diagnoses missed by primary care providers. Our prior research indicates that some primary care providers fail to diagnose some cases of depression and alcohol use disorder (
27). These findings support the possibility that the CIDT is more effective than demonstrated here because this study captured only patients who received diagnosis of a mental, neurological, and substance use disorder from a primary care provider. Therefore, patients who sought care because of the CIDT but who were not diagnosed and registered by the primary care worker would not have been captured in the study design.
Moreover, future use of the CIDT in other settings should take into account the risks associated with applying the tool (as was the case in this study), ensuring that there is sufficient social capital in the communities where it is introduced, that the approach is implemented by community members who are respected and trusted, and that the risk of stigmatization is explicitly addressed.
Although this study did not include treatment outcomes, a prior evaluation for this project has shown that patients in other health facilities who were referred by using CIDT had positive treatment outcomes (
27). Six months after treatment initiation, 93.9% of patients who had been diagnosed as having depression and 95.1% of patients who had been diagnosed as having alcohol use disorder had been provided with minimally adequate treatment. Effect sizes for treatment outcomes in this program were 0.58 for depression, 0.34 for alcohol use disorder, and 0.43 for psychosis (
27). Regarding whether those most in need of treatment were receiving care, routine monitoring of health care utilization data demonstrated an increase in the percentage of patients with alcohol use disorder contacting health care, from 0% at baseline to 7.5% after initiation of the MHCP (which included the CIDT). Contact coverage increased from 0% to 12.2% for depression, from 1.3% to 11.7% for epilepsy, and from 3.2% to 50.2% for psychosis (
27).
Efforts to scale up mental health care services to achieve adequate treatment coverage currently involve the integration of WHO’s mhGAP-IG within primary health care systems in over 80 countries (
28). In order to capitalize on governments’ investments to make mental health care available, a demand-side intervention, such as case detection using the CIDT, should be part and parcel of these programs, in order to optimize service utilization (
29). Furthermore, we recommend developing, evaluating, and comparing other low-cost demand-generating strategies—for example stigma reduction (
30), systematic awareness raising (
31), or invitation cards (
23)—alongside efforts to scale up mental health care in LMICs. A combination of strategies may be needed to facilitate uptake of mental health services, especially for the most vulnerable and hard to reach. Moreover, given that similar gaps in help seeking are observed in high-resource settings, such as North America and western Europe (
7–
12,
32), it will also be important to explore how lessons learned in LMICs can be applied in high-income countries. The existence of community networks among immigrant families, military families, and rural populations suggests that the CIDT could contribute to reducing the gap in access to mental health care.