Spiritual psychotherapy involves the utilization of spirituality and religion by clinicians within mental health treatment settings to affect positive symptom changes among patients (
1). Although this area of clinical innovation and research remains at the sidelines of mainstream psychiatry because of historical tensions and a lack of funding (
2), it has gained some traction in recent years in light of accumulated data highlighting both the positive and negative effects of spirituality and religion on mental health (
3,
4). Several clinical trials have been conducted on spiritual psychotherapy to date, and meta-analytic results suggest that such approaches are as effective on the whole as secular psychotherapies for a range of clinical targets (
5–
10). However, methodological limitations are common in these studies, and caution should be used when interpreting previous findings (
11). Another significant limitation is that the vast majority of research on spiritual psychotherapy has been conducted in outpatient settings, and little is known about the feasibility of spiritual approaches within inpatient, residential, and intensive (e.g., partial hospitalization) levels of care. This latter concern is significant because more than half of acute psychiatric patients report a desire to integrate spirituality into treatment when asked (
12).
The practice of spiritual psychotherapy is heterogenous, mirroring the diversity of spiritual and religious practices worldwide and the myriad ways in which clinical psychiatric presentations manifest. However, its primary methods are to promote spiritual resources and to alleviate spiritual distress as catalysts to clinical change (
13). Promoting spiritual resources involves harnessing spiritual core beliefs in cognitive therapy approaches (
14), practicing spiritual exercises in vivo to modulate affective states (
15), and helping patients to recognize aspects of spirituality in order to aid in their recovery and make them aware of how spiritual distress contributes to their symptoms. Spiritual distress involves tensions and conflicts about spirituality or religion and is strongly associated with a host of psychiatric symptoms (
16). Although methods to address spiritual distress are still evolving within the clinical literature, it is generally thought that simply helping patients to identify, recognize, and articulate such concerns is clinically useful (
1).
In psychiatric hospital settings, psychotherapeutic interventions tend to be focused, brief, and part of a comprehensive treatment approach that typically includes psychopharmacology, neurotherapeutics (e.g., electroconvulsive therapy), case management, and milieu therapy (
17). Additionally, patients generally self-refer to psychotherapy groups and participate voluntarily. Evaluation of psychotherapy’s clinical effects (e.g., reduced distress and improved functioning) within such settings is therefore methodologically challenging; however, it is possible to determine the feasibility of new psychotherapeutic methods by assessing patient experiences and acquisition of psychosocial skills (
18).
Research on spiritual psychotherapy is particularly methodologically complex because patients seeking spiritual psychotherapy tend to perceive nonspiritual treatments in a spiritual light, whereas patients who are not interested in spiritual approaches tend to perceive spiritual material as having little sacred meaning (
15). However, spiritual psychotherapy, even within acute settings, can be evaluated in terms of patients’ perceived benefit from treatment: do such approaches help patients to identify spiritual resources they can use to reduce distress (including spiritual distress) contributing to their symptoms?
In 2019, we published a clinical protocol titled, Spiritual Psychotherapy for Inpatient, Residential, and Intensive Treatment (SPIRIT) (
19). We reported our process for developing this flexible group-based spiritual psychotherapy protocol, described each module of our approach in detail, and made the entire protocol available to the academic community via online supplemental material (see
online supplement to this article). In this study, we describe empirical findings from a dissemination trial of SPIRIT conducted across the entire divisional structure of a large academic psychiatric hospital over a 1-year period. We evaluated the feasibility of our approach and the extent to which patients’ demographic, clinical, and spiritual and religious characteristics predicted their perceptions of benefit from this treatment. We also evaluated the extent to which clinicians’ demographic characteristics and religious affiliations were associated with observed effects.
Methods
Procedures
A detailed description of the SPIRIT clinical protocol and of its development has been previously published (
19). Notably, our treatment approach provides structure, guidance, and materials (e.g., handouts) while giving clinicians flexibility to use various aspects of the protocol in each given session, depending on the demographic, spiritual and religious, and clinical characteristics of the group. Adult patients (ages ≥18 years, N=1,443) and clinicians (N=22) were recruited to participate in this study. Patients came from specialized units providing acute psychiatric treatment for mood, anxiety, psychotic, alcohol- or substance-related, traumatic, eating or feeding, personality, and other disorders. Patients self-referred to SPIRIT groups and voluntarily completed surveys. This study was approved by the Partners Healthcare Institutional Review Board.
This study was conducted at McLean Hospital, an independent psychiatric hospital in Belmont, Massachusetts, affiliated with Harvard Medical School, on various clinical units throughout the hospital providing treatment for a broad spectrum of mental disorders. Given the nature of this clinical setting, there was some heterogeneity in how patients were recruited and whether other concurrently run psychotherapy groups were offered in lieu of SPIRIT; however, patients generally were provided with the option to participate in a “spiritual psychotherapy group” or an alternative intervention. All patients completed just a single SPIRIT group session. Subsequent to SPIRIT participation and completion of measures (described below), research staff accessed patient medical records to obtain additional demographic and clinical data (e.g., age, gender, race, employment status, psychiatric diagnoses, medications, electroconvulsive therapy, suicidality, self-harm, and recent hospitalization within the past 6 months). No adverse events were reported with any patients during the course of the study.
Clinicians were recruited to participate in a brief training and to provide SPIRIT to patients over a 1-year period. Training involved one individual meeting (lasting 30–60 minutes) with each clinician to review the treatment protocol, followed by observing study staff facilitating a SPIRIT group (for 30–60 minutes). Subsequently, depending on the clinician’s comfort level with the material, clinicians observed or co-led additional groups with study staff until they felt ready to provide SPIRIT independently.
Measures
Immediately after participating in SPIRIT, patients completed items from the Clinically Adaptive Multidimensional Outcome Survey (CAMOS) (
20), which assesses several aspects of spirituality and religion (affiliation, importance of spirituality, importance of religion, and belief in God) as well as indicators of spiritual distress (concerns about spiritual life, loss of spiritual inspiration or direction, distance from God, and spiritual guilt). The latter four items were summed to produce a summary measure of spiritual distress. Patients also completed two items about the extent to which they benefited clinically from participating in the SPIRIT group: “This group helped identify spiritual/religious resources that I can utilize to reduce my distress” and “This group helped identify spiritual/religious struggles that are contributing to my distress.” A 5-point Likert-type scale ranging from “not at all” (0) to “very much” (4) was used for all items.
Analytic Plan
We tabulated descriptive values for patients and clinicians with regard to demographic, clinical, and spiritual and religious characteristics. We used Pearson correlations, t tests, and analyses of variance to examine the extent to which patients’ demographic, clinical, as well as spiritual and religious characteristics predicted their reported benefit from the group along two dimensions: identifying spiritual and religious resources to aid in recovery and identifying spiritual and religious struggles that contribute to distress. For the latter analyses, we included only patients who reported a minimum score of 2 on the CAMOS spiritual distress subscale (representing the top three quartiles within our sample). Finally, we evaluated the extent to which clinicians’ demographic as well as spiritual and religious characteristics predicted these outcomes. Given that most demographic and clinical factors did not predict patient response to treatment (see Results), we did not control for type I error inflation despite conducting multiple comparisons.
Results
The 1,443 patients had heterogeneous diagnoses (
Table 1) and highly acute characteristics: 30% (N=440) had three or more psychiatric diagnoses, 42% (N=609) had suicidal ideation, and 55% (N=787) were taking antipsychotic medications. Surprisingly, the mode of patients reported being spiritual but not religious or having no religious affiliation (39%, N=566); however, most patients were diversely affiliated, including Catholic (29%), Protestant Christian (15%), Jewish (6%), and other (4%) religious groups. The vast majority of patients endorsed “fairly” or higher belief in God (76%, N=1,101) and “fairly” or greater importance of spirituality (82%, N=1,190).
Clinicians’ demographic characteristics are presented in
Table 2. The clinicians had a range of educational and career backgrounds, including bachelor-level mental health specialists (N=8); master’s-level social workers (N=3), expressive art therapists (N=5), nurses (N=1), and chaplains (N=1); and doctoral-level psychologists (N=4). Most clinicians reported a personal religious affiliation (36% Protestant, 14% Buddhist, 14% Catholic, 9% Jewish, and 5% Muslim), and about one-quarter reported being spiritual but not religious or no affiliation (23%, N=5).
Overall, the vast majority of patients (69%, N=998) reported that SPIRIT helped them to identify spiritual and religious resources to aid their recovery to a “fairly” or greater extent (top three scale anchors), and 47% (N=676) reported such benefits to a “moderately” or greater extent (top two anchors). Predictors of patients’ responses to SPIRIT are presented in
Table 3. Demographic factors did not predict reported benefits from SPIRIT, except for college students, who were slightly less likely to identify spiritual resources (p=0.05). Thus, patients of various ages, genders, races, and socioeconomic statuses were equally likely to identify spiritual resources from participating in SPIRIT.
Similarly, clinical factors were not associated with perceived benefits from SPIRIT. That is, patients presenting with diverse diagnoses, irrespective of whether various psychiatric conditions were primary or simply present or absent, responded equally to SPIRIT, as did patients with higher versus lower levels of acuity (e.g., number of diagnoses, number of medications, use of antipsychotic medications, electroconvulsive therapy, recent previous hospitalization, recent self-harm, or recent suicidality). Patients’ spiritual and religious characteristics, including religious affiliation, belief in God, importance of religion, and importance of spirituality, all predicted greater perceived benefit from SPIRIT. However, most patients with no religious affiliation (80%, N=200 of 251), no belief in God (76%, N=127 of 167), and no importance of religion (78%, N=255 of 325) or spirituality (64%, N=51 of 80) reported at least “slight” perceived benefits from SPIRIT.
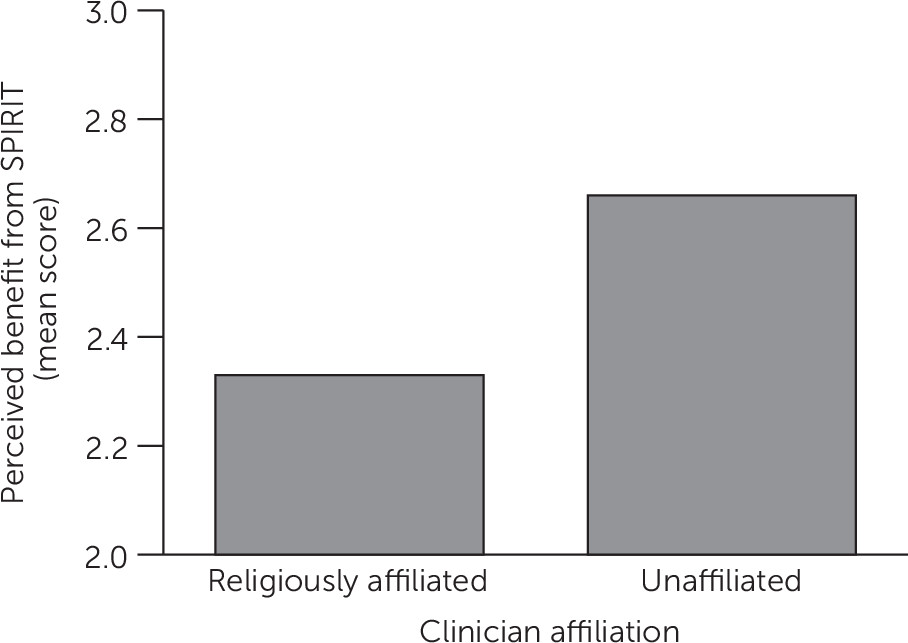
Patients attending SPIRIT groups run by younger (vs. older) clinicians reported more benefit from treatment, as did patients attending groups run by non–religiously affiliated clinicians as compared with religiously affiliated clinicians (
Figure 1). We ascertained that clinicians’ religious affiliation remained a significant predictor of less patient identification of spiritual resources, even after controlling for clinician age (partial r=0.07, p=0.01); moreover, clinician age remained a significant predictor of treatment benefits when the analyses controlled for clinician religious affiliation (partial r=−0.10, p<0.001). We also found that clinician religious affiliation did not interact with patient religion in predicting responses to spiritual psychotherapy, suggesting that religious clinicians were less effective in delivering SPIRIT, irrespective of patient religious affiliation.
Among patients who reported significant spiritual distress, most (76%, N=735 of 973) reported that SPIRIT helped them to identify spiritual and religious struggles that were contributing to their distress to a “fair” or greater extent (top three anchors), and 51% (N=500 of 973) reported that SPIRIT did so to a “moderate” or greater extent (top two anchors). Several patient demographic factors were significant predictors of these effects: older age, geriatric age, non-White race, and lower socioeconomic status were associated with greater identification of spiritual distress. However, none of the clinical factors that we assessed were related to each other. Thus, patients of diverse diagnoses and acuity levels were equally likely to identify spiritual distress from participating in SPIRIT. Religious affiliation was not associated with greater identification of spiritual distress; however, belief in God and importance of religion and spirituality were significant predictors of spiritual distress identification. Demographic characteristics and religious affiliation of clinicians were unrelated to patient identification of spiritual distress.
Discussion and Conclusions
Our results indicate the feasibility of disseminating SPIRIT to demographically, clinically, and religiously diverse patients presenting to a psychiatric hospital for acute care. In the conceptualization process for this study, some clinical staff members raised concerns that acute psychiatric patients, particularly individuals with psychotic disorders, may decompensate when discussing spiritual and religious matters. It is therefore significant that no adverse events were reported throughout the study, that the vast majority of patients reported significant benefits, and that patients with highly acute characteristics (e.g., those who were suicidal, self-injurious, or receiving electroconvulsive therapy) and individuals with lower acuity levels (e.g., residential patients presenting with eating disorders or substance use disorders) reported equivalent effects of the intervention.
The large number of patients in our study, all of whom self-referred to treatment and completed measures voluntarily and without any compensation, is also noteworthy and consistent with previous findings suggesting that patients have a broad-based desire for spiritual psychotherapy (
12). It is also noteworthy that non-White patients were more likely to identify spiritual struggles during participation in SPIRIT, suggesting that our approach may help improve clinical engagement with people of color, who have higher rates of religious (
21) and spiritual struggles (
22) compared with White adults. These findings are likely generalizable to other acute psychiatric settings, given that treatment was provided by diverse staff with minimal training, within a relatively irreligious area of the United States (
23).
We observed several surprising findings. Nearly 40% of the sample, representing the statistical mode, reported no religious affiliation, and most of these patients reported benefits from SPIRIT. Religiously affiliated and unaffiliated patients were equally likely to identify spiritual distress during SPIRIT participation. This finding is consistent with other recent results suggesting that spiritual distress can occur among individuals without faith systems (
24,
25). It is commonly thought that spiritual psychotherapy is primarily, if not solely, for patients who are religious (
26); however, our results suggest that religious affiliation is not a prerequisite for benefiting from spiritual approaches to treatment.
Similarly, clinical diagnoses, including the presence of mania, psychotic, and obsessive-compulsive disorders, which can involve symptoms that have religious themes and resemble spiritual concerns, were unrelated to patient identification of spiritual distress. This finding indicates that spiritual struggles and spiritual symptoms may be orthogonal to one another, which contrasts with what the clinical literature currently suggests (
27). We also observed that older age was not significantly associated with better or worse perceived benefits from SPIRIT. For the past several decades, demographic data from national studies have shown a clear trend, such that religious affiliation, belief, and practice are nearly twice as common among geriatric individuals as they are among younger adults (ages 18–29 years) and decrease with each younger age group (
28). Our results, however, suggest that spiritual psychotherapy is desired by, and potentially appropriate for, individuals across the entire spectrum of adult development. Taken in aggregate, all of these surprising findings speak to the importance of conducting empirical research on spirituality and religion and mental health; as we have shown here, this area of human functioning is highly nuanced and complex, and common assumptions and biases may be incorrect.
Perhaps the most surprising finding in our study was that a greater clinician religious affiliation was associated with worse treatment outcomes in the practice of spiritual psychotherapy, irrespective of patient religious affiliation. This finding is consistent with at least one previous, well-conducted controlled trial of spiritual psychotherapy by Propst and colleagues (
29). In that study, a cohort of religious outpatients with depression were randomly assigned to receive religiously accommodative cognitive-behavioral therapy delivered by either religious or secular therapists; results of this study showed that the latter outperformed the former on both interviewer and self-report assessments. Our results, along with these previous findings, suggest that religious therapists may be less apt in providing spiritual psychotherapy, compared with their secular colleagues. It is possible that religious therapists struggle to maintain objectivity about the subject matter when delivering clinical interventions that include spiritual content.
Along these lines, although no adverse events were reported that would suggest that any therapists in our study were perceived as proselytizing, some patients may view the delivery of spiritual psychotherapy by religious therapists as duplicitous. Conversely, secular psychotherapists providing spiritual support may be better able to focus on clinical change, as opposed to spiritual change. Moreover, secular clinicians might be better positioned to validate and convey the importance of patients’ spiritual needs because they have no personal or religious incentive. We did not assess whether clinicians disclosed their religious identity (or lack thereof) to patients or whether patients perceived their clinicians as having a religious affiliation. As such, we cannot determine whether the aforementioned effects were consciously or unconsciously mediated or whether they were potential mediators. Further research is required to study all of these interesting possibilities.
Our study’s findings were limited by the self-referral and voluntary participation of patients, heterogeneous treatment provision, and the fact that SPIRIT was only one component of comprehensive acute mental health care. The lack of a control group was also a limitation, although as discussed in our introduction, this setup was by design given the methodological challenges associated with conducting clinical trials of psychotherapy within acute psychiatric settings and with spiritual psychotherapy in particular. Furthermore, our statistical analyses evaluated predictive effects of numerous clinical, demographic, and spiritual and religious factors on patient experiences within a large and diverse clinical sample. Thus, because of our study design, patients themselves served as the between-subjects control group.
We believe our methods were sufficient to study the research question regarding the feasibility of SPIRIT for introducing spiritual psychotherapy into acute psychiatric treatment. Furthermore, our large sample size (of both patients and clinicians) and the naturalistic setting of the study render our findings to be more generalizable than laboratory-based randomized controlled trials. In addition, the relatively irreligious locale of our study created a conservative context for evaluation. We hope that SPIRIT will be disseminated to other acute psychiatric settings to provide patients with spiritual psychotherapy as a catalyst to clinical change, and we anticipate that such efforts may generate more knowledge relevant for the therapeutic field about this important yet understudied area of life.