Utility of Investigations, History, and Physical Examination in “Medical Clearance” of Psychiatric Patients: A Meta-Analysis
Abstract
Objective:
Methods:
Results:
Conclusions:
HIGHLIGHTS
Methods
Data Sources and Searches
Study Selection
Data Extraction
Data Analysis
Quality Assessment
Results
Search Results
Study Characteristics
| Investigationsb | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study | Sample | Design | Outcome | Overall | Individual | Historyb | Physical examb | Comments |
| Amin and Wang, 2009 (27) | N=375; sex and age unspecified; diagnosis, “normal mental status to florid psychosis” | Prospective, 21 months; ER; protocolized; evaluator, ER resident | Change in management among patients with a normal history and physical exam | 0% | UA, 0%; thyroid, 0%; CBC, 0% | Indet | Indet | Patients with normal history and physical exam had low likelihood of significant yield from investigations |
| Chandler and Gerndt, 1988 (28) | N=224; males, 47%; mean age, 39; diagnoses: 18% schizophrenia, 8% substance use disorder | Prospective, 4 months; inpatient; evaluator, psychiatric resident | Change in diagnosis or treatment | Indet | CBC, 0%; thyroid, 0% | 4% | 12.1% | History and physical exam played an important role in the detection and treatment of illness |
| Colgan and Philpot, 1985 (29) | N=167; females, 71%; mean age: 79 for females, 75 for males; diagnosis, 41% dementia | Retrospective, 18-month chart review; inpatient; protocolized; evaluator, admitting psychiatrist | Change in management among older inpatients | 49% | CBC, 8.1%; glucose, 2.8%; folate, 3.8%; B12, 5.3%; thyroid, .7%; syphilis, .8%; UA, 17.5%; CT head, 3.5%; CXR, 7.7%; ECG, 14.3% | Indet | Indet | CBC, serum folate, urea, electrolytes, and UA recommended |
| Crede et al., 2011 (30) | N=604; males, 67%; median age, 29; diagnosis, “acute psychosis” | Retrospective, 6-month review; ER; protocolized; evaluator, ER physician | Change in diagnosis or management | .3% | LP, 0%; thyroid, 0% | Indet | Indet | Investigations provided little additional information to that obtained by history and physical exam |
| Dolan and Mushlin, 1985 (31) | N=250; females, 60%; mean age, 42; diagnosis, 58% major affective disorder | Retrospective, 11 months; inpatient; protocolized; evaluator, internist | Change in diagnosis or management | 4.4% | Na, .4%; thyroid, 3%; CR, 0%; syphilis, 1.1%; CBC, 3.8%; WBC, 3% | 20.8% | Indet | Routine investigations unnecessary; select tests in patients with high pretest probability of disease may be of benefit |
| Dubin et al., 1983 (32) | N=38; males, 53%; mean age, 58; diagnosis, organic brain syndrome (89% disoriented) | Prospective, 1 year; psychiatric ER; protocolized; evaluator unspecified | Utility of physical exam and investigations | 16% | Glucose, 7.9%; BUN, 7.9% | Indet | Indet | Investigations largely not helpful in determination of etiology of organic brain syndrome |
| Eastwood et al., 1970 (33) | N=100; males, 53%; mean age, 34; diagnoses: 60% affective disorder, 8% schizophrenia | Prospective, study period unspecified; psychiatric ER; protocolized; evaluator, psychiatrist | Frequency of unrecognized nonpsychiatric illness | 1% | CBC, 1% | Indet | 11% | Excluding anemia, all patients had symptoms or signs apparent on history or physical exam |
| Ferguson and Dudleston, 1986 (34) | N=650; females, 55%; 26–35 age group, 21%; diagnosis, “affective psychosis” | Retrospective, 2-year chart review; inpatient; nonprotocolized; evaluator, psychiatrist | Incidence of tests resulting in change in treatment | .8% | Syphilis, 0%; thyroid, 0%; UA, .8% | Indet | Indet | Routine investigations of little value |
| Hall et al., 1980 (35) | N=100; females, 55%; mean age, 28; diagnosis, 38% schizophrenia; no “significant medical illness”; majority under mental health warrant | Retrospective, study period unspecified; inpatient; protocolized; evaluator, general practitioner | Illnesses that caused or exacerbated psychiatric symptoms | Unspecified | UA, 6%; ECG, 9%; CBC, 15% | 28% | 40% | Detailed history and physical exam and select investigations (e.g., ECG, CBC, UA) recommended |
| Hatta et al., 1998 (36) | N=259; males, 100%; age unspecified; diagnosis, “severely disturbed involuntary patients” | Prospective, 18 months; psychiatric intensive care unit; protocolized; evaluator, psychiatrist | Contributions of physical exam, history, and investigations toward new diagnosis | 21.6% | K+, 2.3%; CK, 13.9%; WBC, 3.1% | Indet | 2.7% | Investigations more important than history, VS, or physical exam in detecting illness among uncooperative patients |
| Henneman et al., 1994 (37) | N=100; males, 63%; mean age, 38; diagnoses: 13% schizophrenia, 63% “organic,” 66% agitated, 60% disoriented; “no medical complaints or physical findings” | Prospective, 9 months; ER; protocolized; evaluator, ER physician or internist | Admission or diagnosis of etiology of psychiatric symptoms | Unspecified | SMA 7, 10%; CBC, 5%; LP, 8%; CT head, 8% | 27% | 6% | Results support investigations for patients with new psychiatric symptoms |
| Janiak and Atteberry, 2012 (38) | N=502; sex, age and diagnosis unspecified | Retrospective, 8-month chart review; inpatient; protocolized; evaluator, ER physician | Influence of inpatient investigations on ER management | .2% | Indet | Indet | Indet | Routine investigations neither cost-effective nor necessary |
| Johnson, 1968 (39) | N=250; sex, age, and diagnosis unspecified; | Prospective, study period unspecified; inpatient; evaluator, psychiatrist | Utility of physical exam | Indet | Indet | Indet | 12% | Physical exam is an important tool in the exploration of psychiatric presentation |
| Kagel et al., 2017 (40) | N=682; males, 78%; 18–41 age group, 94%; diagnosis, “chief psychiatric complaints” (e.g., depression, anxiety) | Retrospective, 2-year chart review; ER; nonprotocolized; evaluator, ER physician | Percentage of dispositions that changed from admission to psychiatric service to medical service | .1% | UA, .1%; BAL, .1%; thyroid, 0%; ASA, 0%; APAP, 0%; CBC, 0%; pregnancy, 0% | Indet | Indet | Mandatory investigations rarely altered disposition |
| Kolman, 1985 (41) | N=68; females, 75%; mean age, 78; diagnosis, 51% dementia | Prospective, 7 months; psychogeriatric unit; protocolized; evaluator, psychiatric resident | Changes in diagnosis or management | Indet | UA, 13%; CXR, 8.5%; B12, 1.5%; ECG, 1.5%; glucose, 1.5%; urea, 1.5% | Indet | Indet | Author suggested UA, CXR, B12, ECG, and urea |
| Korn et al., 2000 (42) | N=80; sex unspecified; age range, 17–83; diagnosis, 20% “bizarre behavior,” 11% depression | Retrospective, 5-month chart review; ER; protocolized; evaluator, ER physician | Changes in management | 0% | CBC, 0%; Cr, 0%; BUN, 0%; pregnancy, 0%; CXR, 0% | Indet | Indet | No benefit to investigations |
| Olshaker et al., 1997 (43) | N=345; males, 64%; mean age, 35; diagnosis, “psychiatric complaints” (e.g., depression, psychosis) | Retrospective, 2-month review; ER; protocolized; evaluator, ER physician | Identification of “acute medical conditions” | .9% | CBC, .9%; glucose, .3%; K+, .6% | 17.7% | 9.6% | No benefit to investigations |
| Parmar et al., 2012 (44) | N=191; sex, age, and diagnosis unspecified | Prospective, two periods of 7 and 13 months; ER; nonprotocolized evaluator, ER residents and physicians | Change in disposition from admission to psychiatric ward | .5% | CBC, 0%; thyroid, 0%; ECG, 0%; UA, 0%; liver, 0% | Indet | Indet | Mandatory investigations did not change disposition of patients after initial history and physical exam |
| Saloojee, 2009 (45) | N=339; males, 69%; mean age, 26; diagnosis, aggressive patients requiring sedation | Retrospective, 11-month review; ER; protocolized; evaluator, ER physician | Utility of investigations, history, and physical exam in exclusion of illness contributing to aggression | 28.9% | CBC, 13.9%; glucose, 5.3% | Indet | Indet | Results support use of investigations for aggressive patients in the ER |
| Schauer and Goolsby, 2015 (46) | N=204; males, 70%; mean age, 24; diagnoses: 52% “suicidal ideation,” 16% “depression” | Retrospective, 11-month chart review; ER; protocolized; evaluator, ER physician | Admission to medical or surgical unit | 0% | ETOH, 0%; CBC, 0%, APAP, 0%; ASA, 0%; pregnancy, 0%, UA, 0% | Indet | Indet | Investigations infrequently resulted in disposition changes |
| Sheline and Kehr, 1990 (47) | N=252; males, 59%; mean age, 33; diagnoses: 57% schizophrenia, 21%, bipolar disorder | Retrospective, 3-month chart review; inpatient; protocolized and nonprotocolized; evaluator unspecified | Change in management or diagnosis | 6.6% | Protocolized: CBC, 3.3%; UA, .6%; nonprotocolized: CBC, 6%; UA, 3.7% | Indet | Indet | Investigations were of low utility; nonprotocolized testing had higher yield than protocolized |
| Thomas, 1979 (48) | N=613; sex, age, and diagnosis unspecified | Retrospective, 12-month review; inpatient; protocolized; evaluator unspecified | Influence of investigations on management | 10% | Syphilis, 0%; thyroid, 2.1%; B12, 8%; CBC, 2.2%; liver, 1%; CXR, 3.1% | Indet | Indet | Investigations of high utility |
| Tobin et al., 2020 (49) | N=441; males, 57%; 18–33 age group, 69%; diagnoses: 52% suicidal ideation, 21% anxiety | Retrospective, 8-month chart review; ER; protocolized; evaluator, ER physician | Changes in disposition | .9% | Indet | Indet | Indet | Protocolized investigations rarely altered patient disposition |
| White and Barraclough, 1989 (50) | N=719; males, 71%; 25–64 age group, 62%; diagnosis unspecified | Retrospective, 15-month chart review; inpatient; protocolized; evaluator, psychiatrist | Change in management or diagnosis | Indet | Thyroid, 2.7% | Indet | Indet | Select investigations may be of benefit |
| Willett and King, 1977 (51) | N=636; females, 59%; mean age, 32; diagnoses: 25% schizophrenia, 19% personality disorder | Retrospective, 17-month review; inpatient; protocolized; evaluator, psychiatric resident | Detection or confirmation of missed nonpsychiatric illness | 2.2% | Indet | Indet | Indet | Investigations were not useful in the psychiatric care of inpatients |
Quality and Bias
Outcome
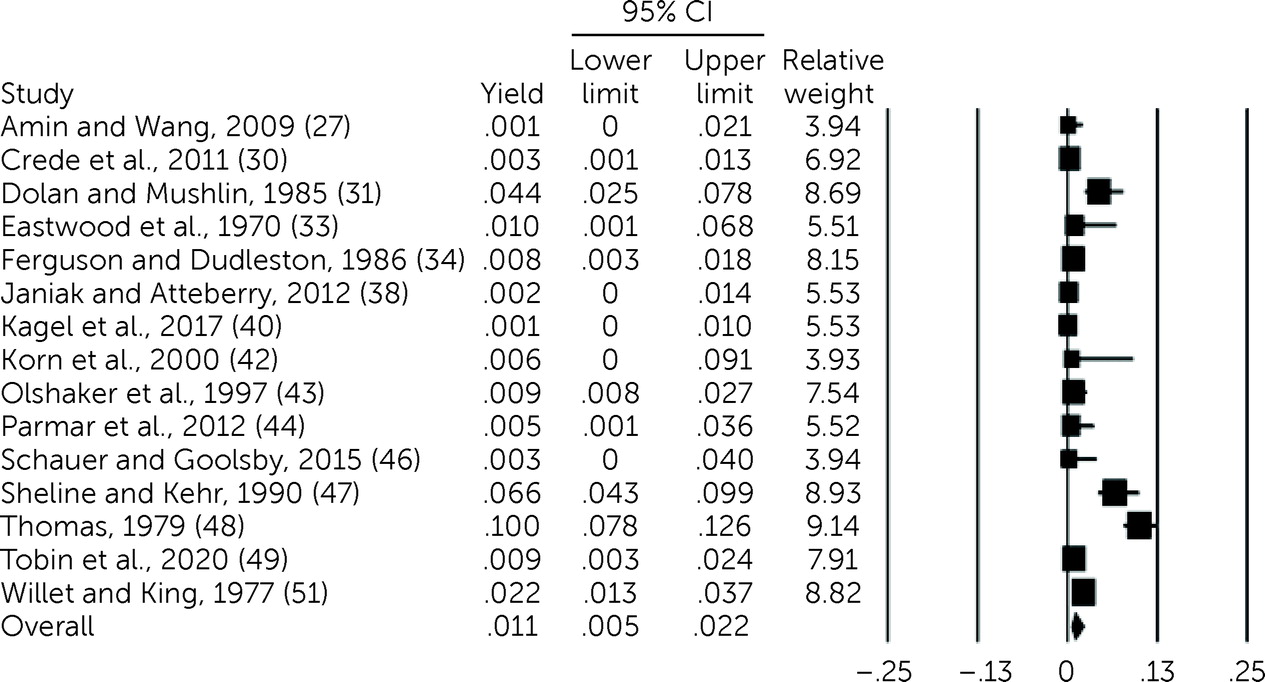
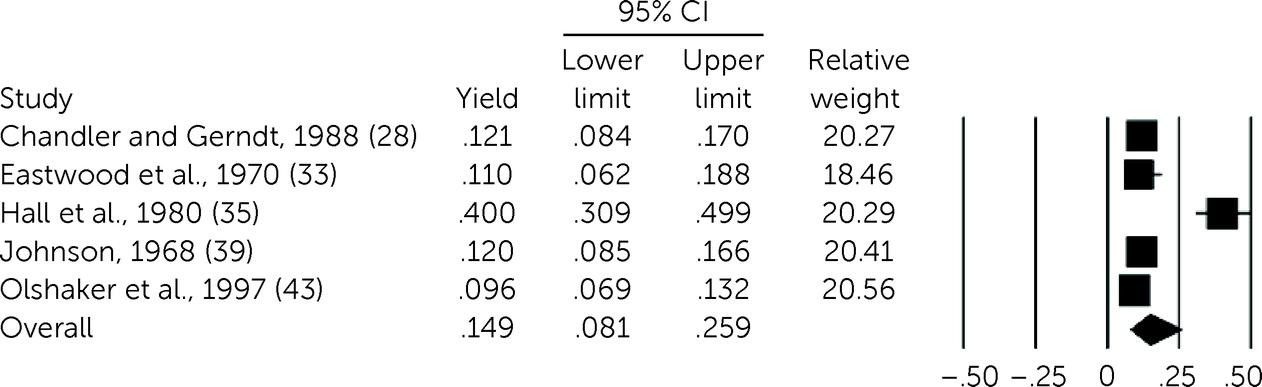
Investigations.
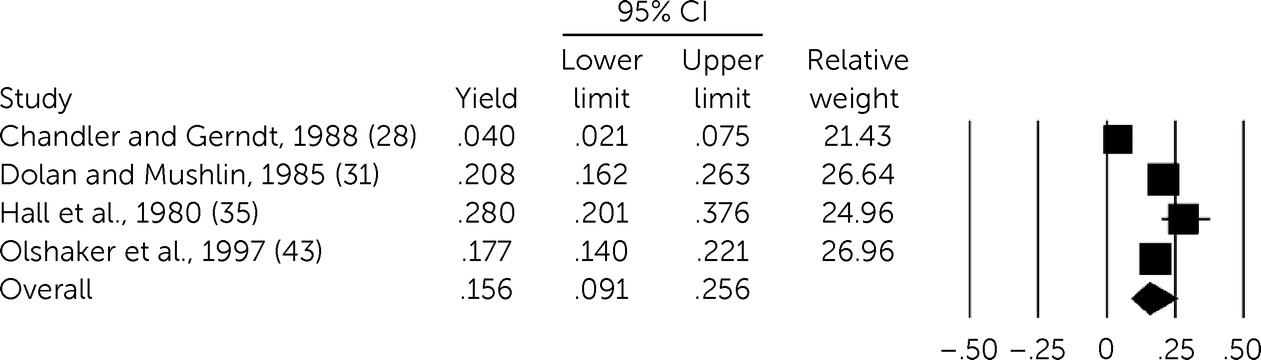
History and physical examination.
Discussion
Conclusions
Supplementary Material
- View/Download
- 229.53 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Competing Interests
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).