Among U.S. military veterans, mental and substance use disorders are prevalent, impairing, and often chronic without treatment (
1,
2). Although evidence-based interventions are often effective (
3–
6), up to one-third of veterans with mental disorders do not receive treatment (
7,
8). Further, even when veterans ultimately engage in services, delayed treatment initiation is common, with one nationally representative study estimating median times of 16 and 2.5 years for pre- and post-9/11 veterans, respectively, between onset of diagnosis and treatment for posttraumatic stress disorder (PTSD) (
9). To engage more veterans in treatment in a timely manner, it is critical to identify determinants and correlates of mental health care utilization.
Treatment utilization research among veterans has primarily focused on psychotherapy for PTSD (
10). Less is known about other disorders, such as depression, anxiety, and substance use disorders, which frequently co-occur with PTSD and each other (
2,
11,
12). Additionally, research has primarily examined veterans in the Veterans Health Administration (VHA) (
10), yet most veterans receive health care outside the VHA (
13). Only one in five veterans use the U.S. Department of Veterans Affairs (VA) for primary health care (
2,
13,
14), and many maintain other health care coverage (
15). Consequently, the prevalence and correlates of mental health care utilization in the population of U.S. veterans remain unknown.
A widely used model to understand use of health care is the behavioral model of health service utilization (BMHSU) (
16), positing that use is determined by predisposing, enabling, and need factors. Predisposing characteristics, such as nonminority ethnic-racial status (
17,
18) and trauma or combat exposure (
18,
19), have been linked to higher rates of health care utilization among veterans. Enabling factors, such as unemployment (
19) or closer proximity to services (
20), may also facilitate use. Need factors have been most robustly associated with use (
19,
20), particularly greater severity of PTSD or depressive symptoms (
17,
20–
23), medical conditions (
19), and screening positive for mental or substance use disorders and comorbid psychiatric conditions (
20,
24,
25). Researchers have also frequently studied factors related to perceived barriers to care, such as stigma, pragmatic barriers, and treatment-related beliefs. Among veterans, more positive treatment beliefs (
21,
24,
26,
27) and lower perceived stigma (
14,
24,
26) have been linked to greater likelihood of mental health care utilization.
Although studies of need factors have often emphasized psychological distress and impairment, we have also examined medical conditions and insomnia, given their associations with mental health (
28), possible links to health care utilization (
24,
29), and the older age of the veteran population. Further, we have considered the role of protective psychosocial characteristics (e.g., grit, defined as trait perseverance that extends to one’s decision or commitment to address mental health needs on one’s own; dispositional optimism; and purpose in life) as possible need factors, because these factors could inhibit or facilitate use by affecting an individual’s perceived need for services. Given the links of these factors to lower psychological distress (
30), individuals scoring higher on these characteristics may perceive an ability to manage distress on their own, in turn dissuading them from seeking care (
21). Furthermore, these traits may moderate the relation between need-based correlates and mental health care utilization; for example, among individuals with high distress, those with higher grit may be less likely to engage in treatment.
In this study, we applied a BMHSU-informed model of health care utilization that included predisposing, enabling, and need factors and perceived barriers to care to examine the prevalence and correlates of current use of mental health care (i.e., counseling, psychotherapy, or medication) in a nationally representative sample of veterans and a subsample of those with a probable current mental disorder (e.g., PTSD, major depressive disorder, or generalized anxiety disorder [GAD]) or substance use disorder (e.g., alcohol use or drug use disorder). Veterans with a probable mental or substance use disorder were grouped together, given high diagnostic overlap among these disorders and because they frequently co-occur among U.S. veterans (
28,
31). We examined correlates of care utilization in the full sample given that functional impairment or distress occur in subclinical or subthreshold conditions (
32,
33) and to adhere to previous methods in utilization literature (
24). We hypothesized that need factors (
10,
17,
20–
22,
24,
25) and fewer barriers to care (
14,
21,
24,
27) would be most strongly associated with use.
Methods
Participants, Procedures, and Variables
Data were drawn from the 2019–2020 National Health and Resilience Veterans Study, a nationally representative survey of 4,069 U.S. military veterans. The human subjects subcommittee of the VA Connecticut Healthcare System approved the study protocol, and all participants provided informed consent. Table S1 in an
online supplement to this article describes the study variables, which included predisposing, enabling, and need characteristics and perceived barriers to care.
Data Analyses
Analyses proceeded in five steps. First, exploratory factor analyses combined variables assessing common constructs into one variable (e.g., functional difficulties). Second, in the full sample and a subsample of veterans with a probable mental or substance use disorder (N=924), independent-samples t tests and chi-square analyses compared characteristics of veterans who were engaged in mental health care with those of veterans who were not engaged. Third, hierarchical logistic regression analyses identified independent correlates of care utilization; we entered variables into sequential blocks by using the BMHSU-informed model of health care to determine specific variance explained by each variable cluster. After identifying significant correlates, we incorporated an interaction term to evaluate whether the strongest protective factor moderated the association between the strongest negative correlate and use of health care. Statistics from the final, comprehensive models with each block of variables are reported in Results. Fourth, post hoc analyses of multicomponent variables (e.g., psychological distress and functional difficulties) were conducted to specify features that drove associations with use. Fifth, relative importance analyses (
34) determined relative contributions of each significant variable in predicting use after accounting for intercorrelations among independent variables.
Results
The mean±SD age of the participants was 62±16 years (range 22–99), and 90% (N=3,564) were male (percentages were calculated with poststratification weighting). Most participants were non-Hispanic White (N=3,318, 78%), with 11% (N=296) being non-Hispanic Black, 7% (N=307) Hispanic, and 4% (N=148) other or mixed race. Veterans of all branches were represented (Army, 47% [N=2,707]; Navy, 20% [N=879]; Air Force, 19% [N=955]; Marines, 6% [N=260]; and National Guard, Reserves, or Coast Guard, 8% [N=409]). Overall, 35% (N=1,353) were combat veterans, and 36% (N=1,476) had served for ≥10 years. Nearly all (N=3,989, 98%) reported having health insurance such as Medicare (N=2,399, 47%) or through a current or former employer (N=1,447, 41%) or the VA (N=1,336, 33%); 21% (N=790) reported the VA as their primary source of health care. (Details regarding data collection are presented in the
online supplement.)
In the full sample (N=4,069), 433 veterans (weighted prevalence, 12%, 95% confidence interval [CI]=11%–13%) reported current engagement in mental health care, including psychotherapy or counseling (N=243, weighted prevalence, 7%, 95% CI=6%–8%), pharmacotherapy (N=383, weighted prevalence, 10%, 95% CI=9%–11%), or both (N=193, weighted prevalence, 6%, 95% CI=5%–6%). In total, 924 (26%) veterans screened positive on one or more of the respective self-report measures of PTSD, major depressive disorder, GAD, alcohol use disorder, or drug use disorder. Most of these veterans (N=685, weighted prevalence, 73%, 95% CI=71%–76%) reported no current engagement in treatment, and 157 (weighted prevalence, 19%, 95% CI=17%–21%) reported receiving psychotherapy or counseling, 211 (weighted prevalence, 23%, 95% CI=21%–26%) pharmacotherapy, and 129 (weighted prevalence, 16%, 95% CI=13%–18%) both types of treatments.
In the full sample, 10% (N=359) had alcohol use disorder, 9% (N=291) major depressive disorder, 9% (N=313) drug use disorder, 8% (N=229) GAD, and 7% (N=214) PTSD. In the subsample of veterans with a probable mental or substance use disorder (N=924), 40% (N=360) had alcohol use disorder, 37% (N=314) drug use disorder, 33% (N=292) major depressive disorder, 30% (N=232) GAD, and 25% (N=217) PTSD; 62% (N=612) had one probable disorder, 21% (N=190) had two, 10% (N=81) had three, 6% (N=34) had four, and 1% (N=7) had all five.
Bivariate analyses for the two samples are shown in Tables S2 and S3 in the
online supplement.
Tables 1 and
2 present results of multivariable regression analyses examining correlates of current health care utilization in the full sample and in the subsample with a probable mental or substance use disorder, respectively. Collinearity diagnostics did not reveal multicollinearity in either model, with variance inflation factors for all variables <5. Results from parallel analyses in a subset of veterans (N=3,007, 74%) unlikely to have a mental or substance use disorder per screening measures are available in the
online supplement.
Relative importance analysis in the full sample revealed that mental dysfunction (i.e., emotional difficulties, such as anxiety and depression and their impact on social and occupational functioning; 19% relative variance explained [RVE]) and cognitive dysfunction (12% RVE), PTSD symptom severity (12% RVE), chronic pain (9% RVE), and grit (6% RVE) accounted for most of the explained variance in health care utilization. In the subsample, mental dysfunction (24% RVE), PTSD symptom severity (18% RVE), the VA as primary source of health care (14% RVE), sleep disorder (12% RVE), grit (7% RVE), and history of suicide attempt (6% RVE) accounted for most of the explained variance (see Figures S1 and S2 in the
online supplement).
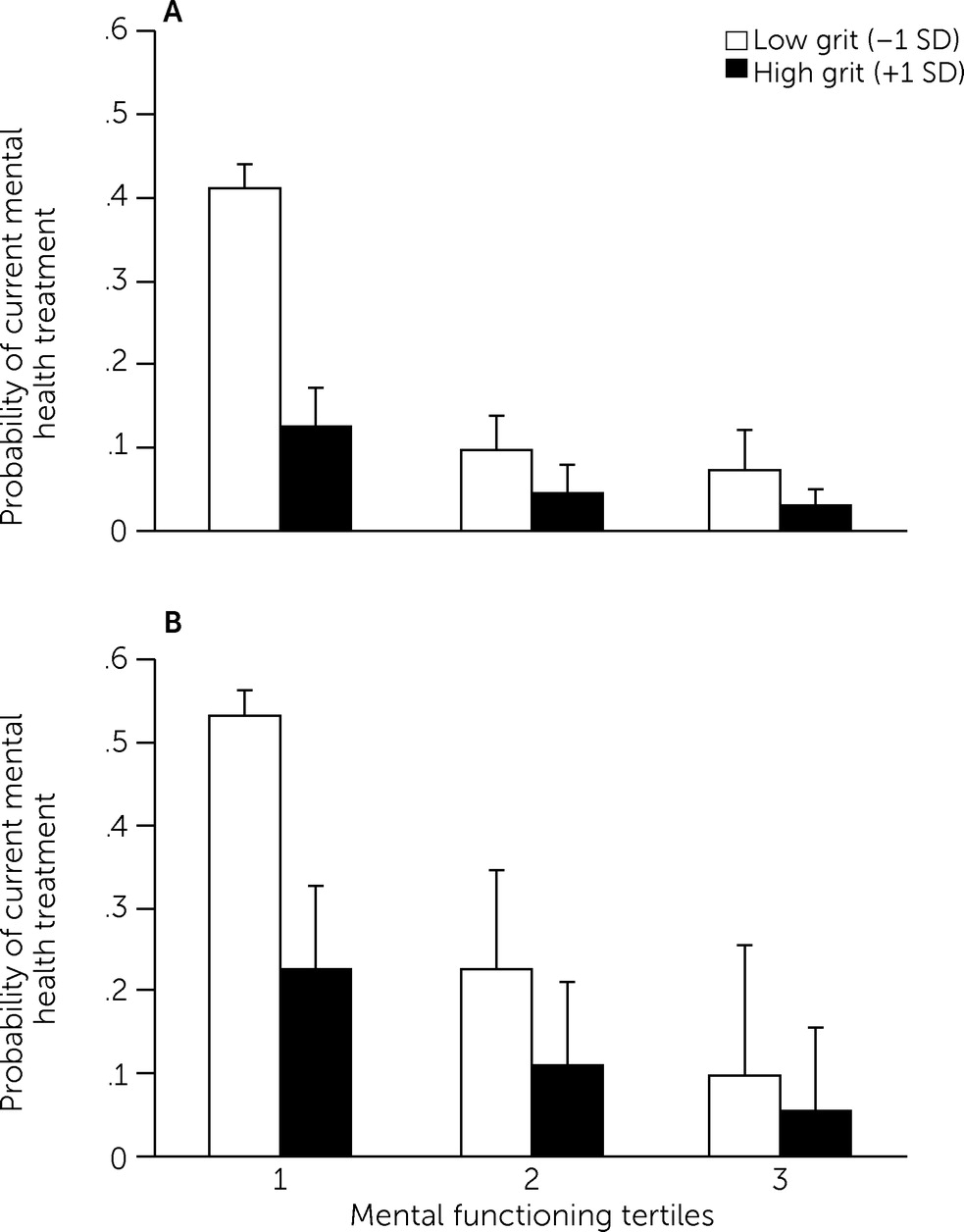
To examine whether the strongest protective correlate—grit—moderated the effect of the strongest need correlate—mental dysfunction—on use of care, we incorporated a mental functioning × grit interaction term into regression models. This interaction was statistically significant in both the full sample (Wald χ
2=4.82, p=0.028; odds ratio [OR]=0.88, 95% CI=0.78–0.99) and the subsample (Wald χ
2=7.94, p=0.005; OR=0.80, 95% CI=0.68–0.93). Among veterans with high mental dysfunction, those with high grit (23%) were significantly less likely to use services than were those with low grit (53%) (
Figure 1).
Discussion
In line with literature indicating underuse of mental health care among veterans (
24), we found that only 27% of U.S. veterans with a probable mental or substance use disorder and 12% of U.S. veterans in general were currently engaged in mental health treatment. A key implication of this finding is that available treatments—although often effective—may not be reaching most veterans who could benefit from them. Correlates were generally consistent with literature reporting that need factors are most robustly associated with mental health care utilization (
10,
17,
19–
22,
24,
25). However, previous studies have rarely examined need factors that may be protective. This study therefore extends this literature, showing that protective psychosocial factors and their interaction with more commonly studied need characteristics may shed additional light on veterans’ health services use and could help inform strategies to engage veterans in treatment.
As hypothesized, need factors emerged as the strongest correlates of mental health care utilization among veterans. Psychological distress—indexed with a composite variable of depressive, anxiety, and PTSD symptoms—was strongly associated with use of care, primarily driven by PTSD symptoms. Indices of cognitive dysfunction and mental dysfunction were also salient contributors, accounting for nearly a third of the explained variance in care utilization. Previous findings suggest that functional impairment accompanying psychological distress may motivate use of mental health services (
35) and underscore the importance of assessing functioning in addition to psychiatric symptoms to most accurately gauge veterans’ mental health care needs. In the full sample, a diagnosis of a substance use disorder was not associated with mental health care utilization, suggesting that the reasons underlying treatment seeking may differ between individuals with mental or substance use disorders. It is also possible that individuals with a substance use disorder sought treatment through 12-step programs rather than psychotherapy, counseling, or medication.
The relationship between functioning and use of health care was further clarified when considered in the context of protective psychosocial factors. Specifically, grit was negatively associated with use and also moderated the relationship between mental functioning and utilization. Grit is positively correlated with constructs such as self-efficacy and conscientiousness (
36,
37), suggesting that this factor may reflect individuals’ self-efficacy and belief in their ability to handle mental health difficulties on their own. These traits are often considered assets or strengths (e.g., self-reliance and perseverance), but in the context of help seeking could also be a barrier (e.g., reluctance to seek help). Protective factors were included as need factors within the BMHSU framework, given that they may affect perceived need for services. Our results suggest nuanced relationships between service use and need and protective factors that merit attention.
Veterans who reported higher levels of mental dysfunction and scored lower on a measure of grit were particularly likely to be engaged in treatment, suggesting that these individuals may reflect a particularly distressed subgroup of veterans. Conversely, veterans reporting similar levels of mental dysfunction who scored highly on grit were less likely to be engaged in treatment. This pattern suggests that higher levels of grit among veterans may reduce their likelihood of seeking treatment, even in the presence of clinically meaningful distress. Clinically, our results highlight the potential utility of promoting grit once veterans begin treatment (i.e., leveraging grit to bolster treatment motivation and engagement and emphasizing goal setting). For veterans reporting greater functional impairment and lower protective factors, interventions designed to cultivate personal strengths (
38)—in addition to mitigating symptoms and functional difficulties—may be beneficial for boosting treatment engagement and response. Notably, of the four protective factors examined (i.e., resilience, purpose in life, grit, and optimism), only grit was strongly associated with mental health care utilization in the subsample. Our findings therefore need replication, and additional research is needed regarding protective factors, their links to distress, and how these factors affect treatment engagement.
Other need factors linked to greater likelihood of use in both samples included a history of attempted suicide, sleep-related difficulties, and medical burden. Although it is encouraging that veterans with suicide attempt histories were more likely to be engaged in treatment, continued efforts in suicide prevention (
39) are critically needed. Suicide rates among veterans have increased in the past two decades (
40), and 60% of veterans endorsing suicidal ideation are not engaged in mental health treatment (
26). Regarding sleep-related difficulties and medical burden, screening veterans for mental health and substance use and connecting them with needed treatment via integration with primary care and nonmental health clinics are effective methods for increasing care access and boosting use (
41,
42) and have been increasingly adopted by the VA and other health care settings (
43,
44). Results suggest that health care systems should continue to leverage this overlap between medical, sleep, and mental health difficulties, because assessment of less stigmatized need factors (i.e., sleep and general medical health) may help identify veterans in need of mental health care. Insomnia treatment, for example, is preferred to PTSD or depression interventions among veterans (
45) and has been theorized as a possible gateway for connecting veterans with needed mental health services (
45,
46). The broad array of need factors also highlights the significance of interdisciplinary, integrative care, which has been increasingly adopted within the VA and has effectively increased veterans’ mental health care utilization (
47).
Enabling factors were generally unrelated to use of mental health care, a result that aligns with literature indicating that need factors are more consistent and stronger correlates of use. Aside from use of the VA as primary source of health care, only unemployment was linked to use in the full sample, and no other enabling characteristics emerged as correlates in the subsample of veterans with a probable current mental or substance use disorder. Employment was negatively associated with use, possibly because employed veterans have less functional or occupational impairment, have less distress due to financial problems, or have work schedules that interfere with treatment. In both samples, health care users were more likely than nonusers to report the VA as their primary source of health care. Veterans who use the VA tend to have higher rates of psychiatric symptoms, suicidality, trauma exposure, and functional impairment (
13); however, the link between primary VA use and care utilization remained significant even when these factors were controlled for. Primary VA care may thus reflect an enabling factor that facilitates access to mental health care services and increases veterans’ likelihood of using them. Further research should examine specific facets of VA care that may promote mental health care engagement (e.g., no or minimal treatment cost, integrated primary and mental health care, routine mental health screenings, and increased telehealth availability), which may also promote mental health care engagement in non-VA systems.
Predisposing characteristics associated with health care utilization were female sex and deployments and, in the full sample, younger age. This finding highlights the potential importance of tailoring strategies to promote utilization among symptomatic veterans who are male, combat-exposed, and older. Outside the BMHSU framework, perceived stigma and barriers to care explained relatively little variance in utilization. Nevertheless, in the symptomatic subsample, endorsement of “it would be embarrassing to seek treatment” was associated with a highly reduced odds of use, whereas in the full sample, endorsements of “it would harm my reputation” and “mental health care does not work” also were associated with significantly reduced odds of use. Although stigma related to mental health treatment has decreased among U.S. military members in recent years (
48), these findings suggest that continued efforts to combat stigma, such as psychoeducation and promotion of mental health literacy, may help motivate treatment engagement. Fortunately, beliefs regarding stigma are modifiable and unrelated to use once veterans have attended even a single mental health visit (
22).
The results of this study should be interpreted in light of several limitations. First, its cross-sectional design precluded examining how changes in correlates over time may affect use of care. Second, screening instruments, rather than semistructured clinical interviews, were used to identify probable mental and substance use disorders. Although the results obtained with the scales we used are known to correlate strongly with results from gold-standard diagnostic interviews (
49,
50), screening via self-report measures may have inflated estimates of disorder prevalence. Third, because the sample comprised primarily older White male veterans, it is important to understand whether the results generalize to younger, more diverse veterans. Relatedly, although the sample was nationally representative, the participation rate from the larger panel of veterans was only 52%. Although poststratification weights enhanced generalizability of our results to the broader U.S. veteran population, it is possible that more symptomatic veterans may have been less represented in this sample, and homeless and institutionalized veterans were excluded altogether. Fourth, psychotherapy and medication categories were combined because only a small number of veterans engaged in psychotherapy only. This data handling may have limited the specificity of our findings, because correlates of medication and psychotherapy use may differ. Fifth, although we adhered to established theory and literature in classifying variables, some variables could have been placed in more than one cluster (e.g., activities of daily living could be an enabling or need factor). Finally, programs such as Alcoholics Anonymous and Narcotics Anonymous were not formally assessed and may affect utilization estimates.
Notwithstanding these limitations, strengths of this study included examination of a broad constellation of variables associated with mental health care utilization in a contemporary, nationally representative sample of U.S. veterans. Additionally, correlates examined in this study, including novel indicators of use (i.e., protective factors), explained 44%−50% of the variance in care utilization, thus providing insight into key correlates of use in this population.
Conclusions
Mental health treatments are often not reaching veterans who need them, a deficiency that may be especially pronounced among veterans who are distressed but also have high numbers of protective factors. Our findings underscore the importance for continued research on strategies to reduce stigma and negative beliefs and promote mental health literacy among veterans, particularly regarding the availability of evidence-based mental health interventions. Future work should also more precisely ascertain the impact of protective factors among veterans with mental and substance use disorders; specifically, our understanding of treatment seeking among veterans will be improved by deciphering whether protective factors reflect veterans’ self-reliance and capacity to manage distress on their own or whether they reflect a barrier to seeking help. Better understanding protective factors and their links to distress and impairment may help identify additional veterans who could benefit from care. Another future direction is to evaluate and disseminate self-help tools such as mobile apps and online programs (e.g., PTSD Coach, Virtual Hope Box, and VetChange), which may be treatment options ideal for veterans with high levels of both distress and protective factors and who want to manage mental health and substance use difficulties on their own.
Acknowledgments
The authors thank the veterans who participated in the National Health and Resilience in Veterans Study and Steven M. Southwick, M.D., and John H. Krystal, M.D., for their critical input into the design of this study.