Much concern has been expressed in recent years about the possibility that disability payments to mentally ill beneficiaries may facilitate substance use and discourage employment seeking. Shaner and associates (
1), studying a sample of veterans with both schizophrenia and cocaine addiction, reported that drug use and psychiatric symptoms both became more severe early in the month in association with receipt of federal disability checks. A more recent study examined mortality rates in the entire U.S. population from 1973 to 1988 and found higher rates of mortality due to substance abuse, homicide, and suicide early in the month, which the authors attributed to receipt of checks from the federal government (
2).
Other studies, however, have demonstrated the important safety-net function of public support benefits (
3,
4), and several cross-sectional studies have suggested that adverse effects of disability payments may be less widespread than some observers have feared (
5,
6). One outcome study of homeless persons also reported that increased benefit payments were associated with a greater likelihood of becoming housed but not with increased alcohol or drug use (
7).
These studies were limited, however, either because they were cross-sectional and thus did not evaluate causal relationships, or because they examined short-term cyclical variations in behavior that were associated with monthly receipt of disability checks but not with the initial award of benefits. Evaluation of the impact of disability payments on health and community adjustment would ideally obtain assessments before and after the initial award of benefits and would compare award recipients with similar applicants who did not receive benefits. Although random assignment to receive or not receive benefits would be both illegal and unethical, observational studies have compared applicants who received benefits and applicants who were denied benefits; the studies reported only moderate differences in subsequent employment or mortality (
8,
9). However, no published study has prospectively compared the effect of the initial award of benefits on a broad range of health and community adjustment outcomes.
In 1992 the Social Security Administration (SSA) and the Department of Veterans Affairs (VA) initiated the Joint Outreach Initiative to facilitate access of homeless mentally ill veterans to Social Security Disability Insurance (SSDI) and Supplemental Security Income (SSI) benefits, especially when they were ineligible for VA benefits. A previous report from that initiative demonstrated that it was successful in increasing the number of veterans who received benefits at participating sites (
10).
The study we report here is a comparison of veterans who received awards and veterans who were denied awards. Working with a sample of veterans who participated in the joint outreach project, we used detailed assessment data obtained just before the initial award decision was made and three months later. The study had two objectives: to identify sociodemographic or health characteristics before the initial award decision was made that might predict who would receive awards and who would not, and to determine whether veterans who were awarded SSA disability payments differed three months later from those who were not awarded such payments in measures of clinical status, quality of life, spending, and income.
Methods
Sample
The study sample included 280 veterans enrolled in the SSA-VA Joint Outreach Initiative between 1992 and 1999 who gave written informed consent to participate in an outcome study in which they would complete a face-to-face interview just before receiving the initial SSA award decision and another three months later. The 280 veterans were a convenience sample identified during periods when an evaluation assistant was available to recruit them and to obtain their written informed consent to participate in the study. Because of the close working relationship between VA case managers and SSA field office personnel, the evaluation team at each site was notified when a decision was near, without being informed of whether an award would be made. Participating sites were located in New York City in Manhattan and Brooklyn, in Dallas, and in Los Angeles.
The SSA-VA Joint Outreach Initiative, described in detail elsewhere (
10), served a total of 2,490 veterans during the time of recruitment for the follow-up study; additional veterans had been served before the follow-up study was initiated. Before entering the program, each participant completed a standard administrative intake form that documented basic sociodemographic characteristics and clinical status indicators. These data were used to compare 32 sociodemographic and clinical status measures between veterans who agreed to participate in the outcome study and veterans who either refused to participate or were not asked to participate. The lack of statistically significant differences between the two groups on any of these measures suggests that the study sample subjects were similar to other program participants.
Of the 280 veterans interviewed at baseline, 175, or 62 percent, were located for a follow-up interview three months later. Two of these participants had reported receiving Social Security disability payments at baseline and were excluded from the analyses, leaving a total sample of 173 veterans. Of this group, 50, or 29 percent, received Social Security benefits—SSI or SSDI payments—and 123, or 71 percent, did not receive Social Security benefits.
Respondents lost to follow-up between baseline and three months were more likely to be black (χ2=6.26, df=2, p<.05), more likely to have a self-reported alcohol problem (χ2= 3.71, df=1, p<.05) or drug problem (χ2=6.32, df=1, p<.01), and more likely to be more impulsive (χ2=5.23, df=1, p<.05)—that is, to have higher discount rates, as discussed below. They were more likely to have legal problems (F=9.05, df=1, p<.01), more likely to be depressed (F=4.05, df=1, p<.05), and more likely to use tobacco products (F=4.29, df=1, p< .05). Hence veterans who were reinterviewed had less severe problems overall than those who were lost to follow-up. Unfortunately, we cannot determine whether this difference affected beneficiaries more or less than nonbeneficiaries, because beneficiary status was determined at the follow-up interview.
Study design
We used a nonequivalent control group design in which outcomes for veterans who received benefits were compared with outcomes for veterans who did not. Because this comparison might be biased by baseline differences between these groups, multiple regression was used to control for such potentially confounding differences.
Measures
The SSA-VA Joint Outreach Initiative baseline evaluation questionnaire documented each veteran's sociodemographic status; quality of housing (
11); sources of income; monthly expenditures on housing, food, and the like as well as on addictive substances; psychiatric problems; substance abuse; physical health status; and implicit time preferences, a measure of impulsivity discussed below. Overall quality of life was evaluated using Lehman's summary measure (
12) of subjective quality of life, rated on a 7-point scale ranging from delighted to terrible. Psychiatric and substance abuse problems were measured using several well-established measures such as the Addiction Severity Index (ASI) (
13), the Brief Symptom Inventory (BSI) (
14), and the Helzer Conduct Disorder Index, a measure of childhood conduct disorder (
15).
Time preference (discount rates). Because of our interest in impulsive spending, we included a measure of time preference or intertemporal choice that reflects each veteran's discount rate—the rate at which future benefits are devalued as compared with present benefits. A high discount rate means that a monetary amount anticipated in the future is much less valuable than the same amount if it was received at present and reflects unwillingness to delay gratification. High discount rates have been empirically linked to impulsivity (
16,
17).
We used a measure of personal discount rate that Fuchs (
17) developed for a study of the relationship between time preference and health status. Respondents were given three hypothetical situations and asked to choose between X dollars now or some amount Y percent greater than X dollars at some point in the future. The respondent's preference for a smaller amount of money now reveals an implicit rate of time discount (
18). By computing the compound interest rate at which the smaller amount of money would grow to an equal larger amount in the designated period, we can estimate whether the patient accepts or rejects the implicit discount rate for each question. Acceptance implies a discount rate lower than that presented in the example, and rejection implies a higher rate. Through a series of questions, this measure identifies a range for each individual's discount rate. High implicit interest rates have been equated with increased impulsivity and the inclination to want money without having to wait for it.
Attitudes about work. Because of our concern with whether cash benefits create work disincentives, respondents were presented with 11 questions that addressed motivation to work—for example, "I would be ashamed of myself if I didn't try to work" and "My friends and family might think poorly of me if I didn't work." They were asked to indicate how much they agreed with each statement on a Likert-type scale running from 0, strongly disagree, to 4, strongly agree. Scores for all 11 questions were summed, and higher scores reflected higher motivation for employment. Internal consistency for the 11 questions was evaluated with Cronbach's alpha, which was .70.
Social Security Administration benefits. All veterans in the analytic sample reported no Social Security benefits at baseline. For the purposes of this study, Social Security benefits were defined as all reported income from either the Social Security Disability Insurance program or the Supplemental Security Income program. All income data were based on self-report.
Data analysis
First, baseline characteristics of those who received Social Security benefits and those who did not receive Social Security benefits were compared using chi square testing and one-way analysis of variance. Multivariate models were then used to compare Social Security beneficiaries and nonbeneficiaries on various outcome measures, adjusting for variables that were significantly different at baseline and baseline levels of each outcome measure. Because we used multiple outcome measures, we used a Bonferroni correction; treating the income and spending categories as two variables yielded a count of 12 comparisons, and so our correction reduced the threshold of statistical significance to .004 (.05/12). We did not use a Bonferroni correction for the comparison of baseline characteristics because of the importance of identifying factors that could potentially confound the outcome analyses. In these analyses the conventional alpha level of .05 was used. All analyses were conducted in SAS System, version 6.12 (
19).
Results
Study participants
As one would expect in a study involving veterans, the final sample of 173 subjects was predominantly male, with 157 men (91 percent) and 16 women (9 percent). The mean±SD age was 47±8.13 years. Ninety-one veterans (53 percent) were white, 68 (39 percent) were African American, and 14 (8 percent) were Latino. More than half the sample was divorced, separated, or widowed (N=102, or 59 percent). The mean±SD number of years of education was 12±2.18.
One-third of the sample (N=55, or 32 percent) reported having worked full time for at least half of the previous three years. Many in the sample (N=73, or 42 percent) reported some earned income during the previous 30 days, but this group had worked an average of only 5±5 days during that time.
Clinical assessments indicated that 42 veterans (24 percent) had a diagnosis of schizophrenia or some other psychotic disorder, 75 (43 percent) a mood disorder, eight (5 percent) a personality disorder, 20 (12 percent) posttraumatic stress disorder, and 40 (23 percent) adjustment disorder. These diagnoses were not mutually exclusive.
In addition, 39 veterans (23 percent) had a diagnosis of alcohol dependence or abuse (without drug abuse), 29 (17 percent) a diagnosis of drug dependence or abuse (without alcohol abuse), and 46 (27 percent) diagnoses of both alcohol and drug abuse. Thus 66 percent had diagnoses of substance abuse or dependence when they entered the program. Levels of active substance use were low at the time of baseline assessment, as by that time most had already been in treatment for several months. On average they reported drinking to intoxication or getting high 3.8±10.41 in the previous month.
Receipt of benefits
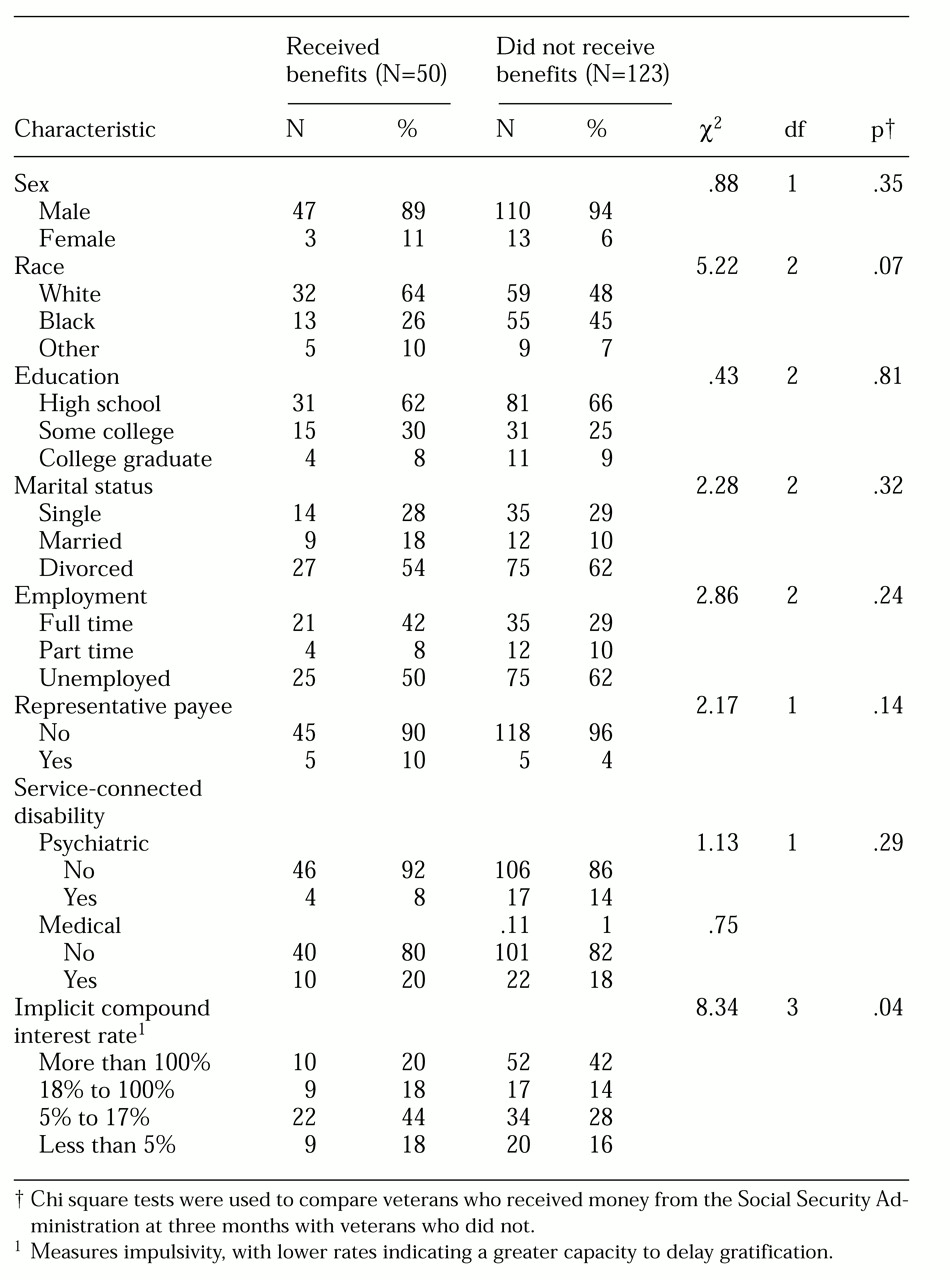
Table 1 compares veterans who received benefits and veterans who were denied benefits on categorical measures at baseline. The only significant difference observed between the two groups was on the time preference measure (χ
2=8.34, df=3, p<.05), with future recipients of Social Security benefits having lower implicit interest rates—reflecting greater time delay and less impulsivity—than those who did not.
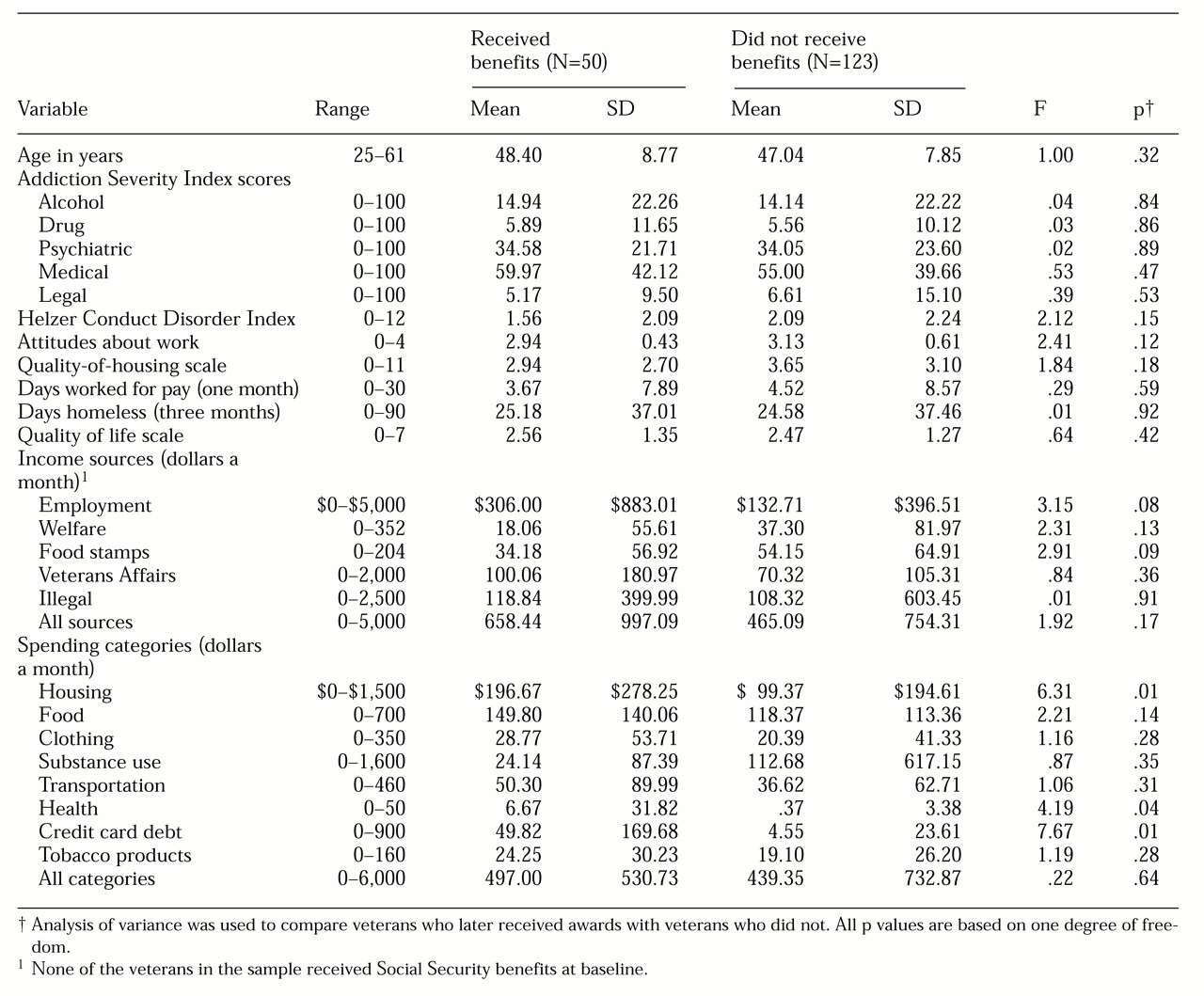
Table 2 compares the continuous variables at baseline for the two groups and shows that participants who later received Social Security benefits were not significantly different from those who did not receive Social Security benefits on measures of health status or community adjustment. Significant differences were noted in expenditure patterns, with future Social Security beneficiaries spending significantly more on housing, credit card debt, and health services.
Three-month outcomes
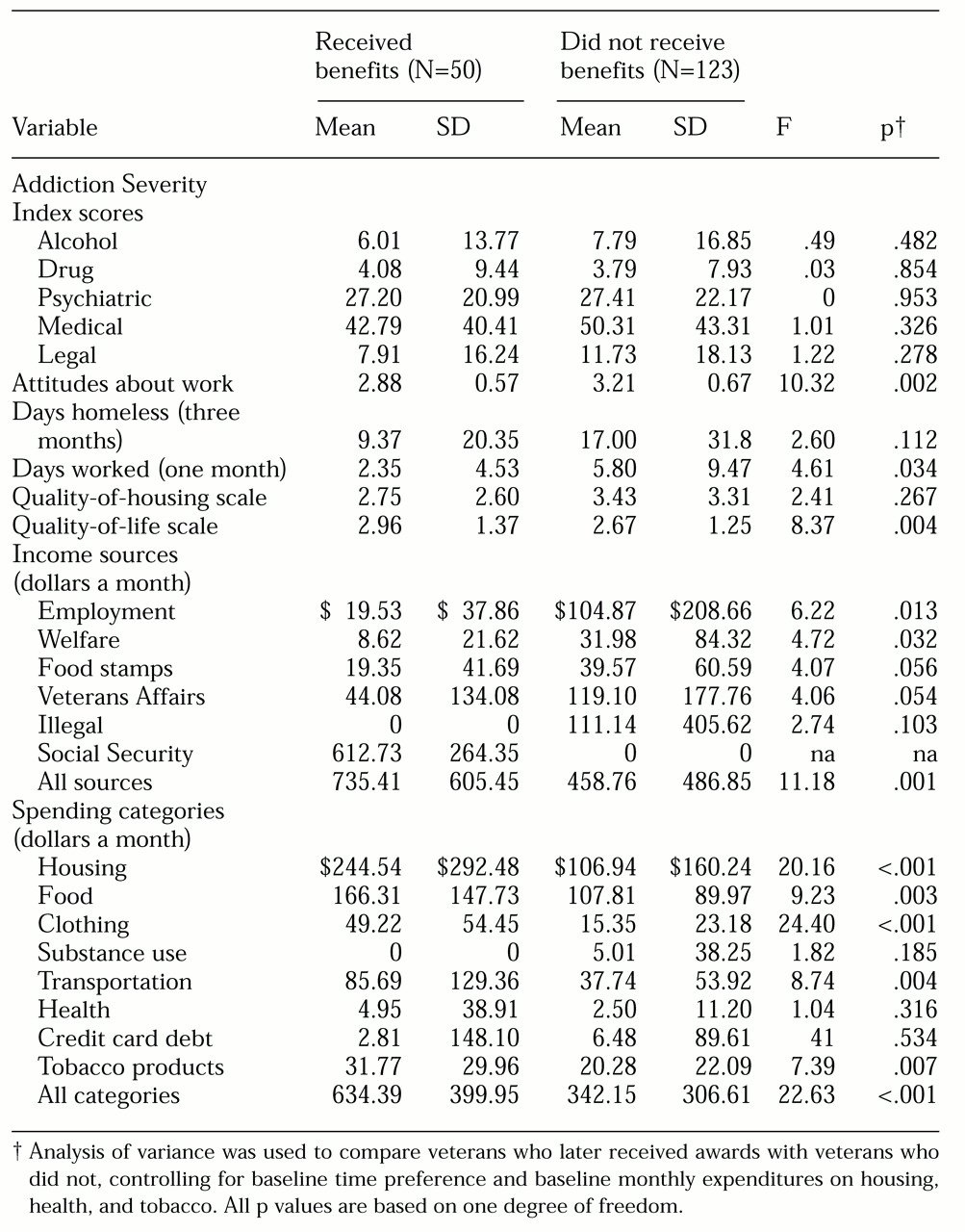
Table 3 presents three-month outcome data in which mean values have been adjusted for measures that were significantly different between the groups at baseline. Veterans who were awarded benefits reported receiving an average of $612 in the previous month from SSA. After baseline differences had been controlled for, significant differences were observed at three months on four measures. Social Security beneficiaries showed less motivation for work, greater overall quality of life, greater total income, and greater expenditures. They were not significantly different from nonrecipients on any health status measure, including measures of substance use (even at an unadjusted alpha level of p<.05).
When all sources of income are added together, Social Security beneficiaries had 60 percent more monthly income than nonbeneficiaries ($735 versus $459), with less income from employment, from welfare, from food stamps, and from VA. Beneficiaries spent more on necessities (housing, food, and clothing), transportation, and tobacco but not on alcohol or drug use. Although on average beneficiaries spent almost half as many days homeless as nonbeneficiaries (9.4 days versus 17 days) and worked half as many days, these differences were not statistically significant.
Discussion and conclusions
This is the first prospective study of the impact of receipt of disability benefits on people with serious mental illness. Although one would have expected veterans who received benefits to be clinically different from those who did not on measures of clinical status or community adjustment, no differences were observed on any of these measures. This result suggests that recipients in this clinical sample may have been no more disabled than nonrecipients.
The only significant difference between the groups was on a measure of time preference showing that the future recipients were more willing to delay satisfaction than nonrecipients. This finding suggests that a key factor in obtaining disability benefits may be patience—a willingness to carefully and thoroughly proceed through the various steps required to obtain benefits. Clients who are impulsive, impatient, or disorganized may be less willing to follow the procedures necessary to obtain benefits, even though they are severely disabled. Unfortunately, data are not available on the official reasons why applicants were turned down, and none of our measures were specifically designed to measure ability to work.
Comparison of follow-up measures three months after the benefit decision was made showed that the average total income of beneficiaries was 1.6 times that of nonbeneficiaries, at $735 per month. This sum represents an annual income of $8,820, about half the amount defined as poverty level. On the positive side, beneficiaries felt more satisfied with their lives and spent more money on necessities such as housing, food, clothing, and transportation. Unlike participants in a previous study in which receipt of benefits was associated with significantly reduced homelessness (
7), our sample showed no significant difference in days of homelessness. We found no evidence of any increased spending on alcohol or drugs, although beneficiaries did spend more on tobacco products. On the negative side, beneficiaries worked less than half as much as nonbeneficiaries, although this was not statistically significant after adjustment for multiple comparisons.
An important limitation of this study is that substance use was not evaluated through chemical tests, and it is possible that beneficiaries underreported their use of alcohol and drugs. In addition, only 62 percent of the sample were located for the three-month follow-up interview, and baseline data suggest that veterans who were not followed up were at greater risk for relapse than those who were. However, we cannot tell whether this bias affected beneficiaries more or less than nonbeneficiaries, as beneficiary status was determined at the follow-up interview.
It might be argued that because the sample was not composed of people with high levels of current alcohol or drug use at the time of the benefits decision, the risk of such use may have been relatively low. However, at the time of admission to the VA clinical program—typically several months before the benefits decision—more than 60 percent of the sample had a diagnosis of current alcohol or drug abuse or dependence. Reanalysis of substance abuse outcomes for this subgroup also showed no significant differences between the groups. Although we do not have measures of severity of substance abuse at the time of program entry, data from previous samples of homeless veterans seen in VA outreach programs show high levels of abuse and dependence at the time of program entry, and this sample was thus likely to be at substantial risk of relapse. We believe these data are informative, suggesting that even among homeless applicants for SSDI and SSI with recent but not current substance use, receipt of disability payments is not likely to trigger or exacerbate an episode.
We conclude that among homeless people with serious mental illness, receipt of disability benefits is not a stimulus to alcohol or drug use but does improve subjective quality of life.