Advance directives gained national attention with the implementation of the Patient Self-Determination Act of 1991 (
1). The durable power of attorney for health care is an advance directive that allows a patient to retain a proxy for decision making when the patient experiences a loss of capacity (
2). The durable power of attorney for health care has had limited use in psychiatric care (
3,
4). Its only use in geropsychiatry that has been studied is the practice of allowing a proxy to give written consent when incapacitated patients with Alzheimer's disease participate in research (
5,
6).
Recently we became aware that a number of psychiatrists use the durable power of attorney for health care to compel psychiatric admissions of unwilling geropsychiatric patients with dementia. Crumpacker (
7) eschews such practice and considers it a violation of a patient's rights, which leaves the participating psychiatrist vulnerable to a lawsuit. To examine the frequency and conditions under which a durable power of attorney for health care is used for this purpose, the authors conducted a survey of hospitals nationwide.
Methods
Medical directors from 630 psychiatric facilities in 50 states were surveyed from August to October 1999. Only facilities in which geropsychiatric patients constituted at least 10 percent of the facility's total admissions were included in the survey. The survey described a geropsychiatric patient who was incapacitated by severe dementia and who refused needed psychiatric admission.
Survey questions included:
• Does the facility have an active policy for using a durable power of attorney for health care to admit such patients?
• Will the facility use a durable power of attorney for health care to admit such a patient if:
—the patient does meet commitment criteria?
—the patient does not meet commitment criteria?
• How frequently does the respondent currently use a durable power of attorney for health care when confronted with either of the above situations? (never, 0; rarely, 1; sometimes, 2; frequently, 3; or always, 4)
• Why doesn't the facility use involuntary commitment instead of a durable power of attorney for health care for such patients meeting commitment criteria?
• What are the respondent's beliefs about the legality of using a durable power of attorney for health care to force admission instead of involuntary commitment?
Results
Of 630 questionnaires mailed, 223 (35 percent) were returned from 46 states. Twenty-five (11 percent) returned responses were invalidated because the geriatric patient population at the respondent's facility was less than 10 percent of the total. The final sample included 198 respondents (31 percent of all mailings and 89 percent of returned responses). A total of 196 hospitals (99 percent) treated voluntary patients, and 165 (83 percent) treated involuntary patients. Sixty-eight hospitals (34 percent) had a dedicated geropsychiatric inpatient unit.
The respondents were almost evenly divided on whether their facility had an active policy for allowing use of a durable power of attorney for health care in coerced admissions. Ninety-four hospitals (47 percent) had such a policy, and 104 (53 percent) did not.
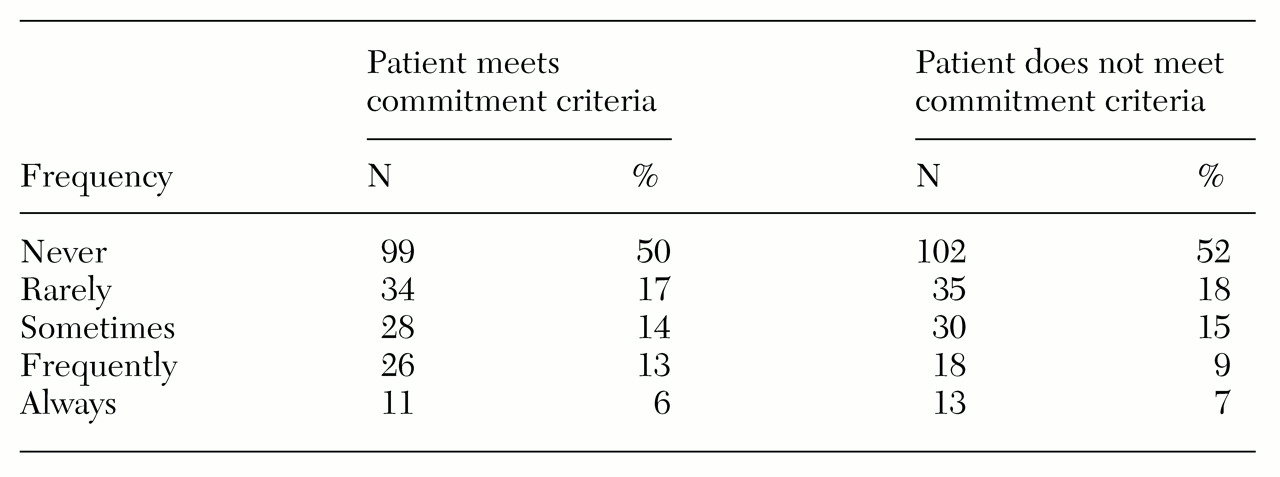
Table 1 lists the frequencies with which the respondents' hospitals used a durable power of attorney for health care in coerced admissions.
As expected, facilities with existing policies used a durable power of attorney to compel admissions much more frequently than facilities without such policies. Such admissions were coerced whether or not patients met commitment criteria. At facilities with an existing policy, the mean±SD frequency rating for using a durable power of attorney to compel admission of patients who met criteria for involuntary admission was 1.88±1.29; the rating for this patient group was .36±.75 at facilities that did not have a policy (Welch's t=10.02, df=146, p<.001). At facilities with an existing policy, the mean±SD frequency rating for using a durable power of attorney to compel admission of patients who did not meet criteria was 1.64±1.36; the rating for this patient group at facilities that did not have a policy was .45±.88 (Welch's t=7.21, df=157, p<.001).
Whether or not a respondent's psychiatric facility provided voluntary, involuntary, or exclusively geropsychiatric services was not correlated with how frequently a durable power of attorney for health care was used. The point-biserial correlations were .09, -.10, and .09, respectively. None of these Pearson product-moment correlations was significant beyond the .05 level.
Ninety-nine respondents gave one or more reasons why the facility used a durable power of attorney for health care to compel admissions. Forty said that using a durable power of attorney allowed them to keep the patient hospitalized longer than commitment would allow. Twenty-nine said that involuntary commitments for such patients are hard to secure. Fifteen stated that their units were not allowed to accept involuntary inpatients. The remainder used this procedure for particular reasons that were specific to their facility or state.
More than a third of the 198 respondents (68 respondents, or 34 percent) believed that using a durable power of attorney for health care instead of commitment is a valid option. More than a third (74 respondents, or 37 percent) believed that it did not violate mental health laws to use this means to compel admission of a patient who is not committable. In contrast, nearly half (94 respondents, or 47 percent) stated that they believed that geropsychiatric patients with severe dementia can be admitted against their will only through use of involuntary commitment procedures.
Discussion and conclusions
This study showed that there are major differences in how psychiatric facilities use a durable power of attorney for health care for the coerced admission of incapacitated geropsychiatric patients. Roughly half of the 198 surveyed hospitals reported having a policy allowing the use of a durable power of attorney for health care for compelling admissions.
About a third of the respondents reported that they coerce admissions through use of a durable power of attorney for health care at least some of the time. Approximately 18 percent said they frequently or always used a durable power of attorney for health care for this purpose. They used this procedure whether or not the patient met criteria for commitment.
The medical directors who responded to our survey cited three reasons why using a durable power of attorney for health care for this purpose may be preferable to involuntary commitment. First, a durable power of attorney allows the psychiatrist to hospitalize a patient for as long as the proxy agrees, whereas involuntary commitment requires release once the commitment standard is no longer met. Second, involuntary commitment can be difficult to obtain for demented geropsychiatric patients. Finally, a hospital may not be able to accept involuntary patients.
Beliefs about the ethics and legality of using a durable power of attorney for health care in forcing admissions of such patients varied markedly among respondents. Thirty-four percent believed that it is optional to use either a durable power of attorney or an involuntary commitment to force admission of such patients, whereas 47 percent believed that such patients can be admitted against their will only through involuntary commitment.
Weaknesses in this study include a disproportional response rate among states. Although the number of surveys sent to each state was proportional to the number of psychiatric facilities listed in that state (
8), the states did not all respond equally. Some states were overrepresented, inclu ding New York with 19 facilities (9 percent), Texas with 16 (8 percent), Pennsylvania with 15 (8 percent), North Carolina with 12 (6 percent), and Missouri with ten (5 percent). In four states, no facilities responded; in eight states, only one responded; and in eight states, only two. In addition, the study did not control for rural or urban location or facility size.
Some respondents reported that their state had laws specifically forbidding the use of a durable power of attorney for health care to admit psychiatric patients. Because three of the states in which respondents reported such laws also had the highest response rates (New York, Pennsylvania, and Texas), the actual use of a durable power of attorney for health care to compel psychiatric admission may be greater than reported in this study.
Despite these limitations, the results underscore the inconsistency with which a durable power of attorney for health care is being used in the United States to coerce admission of incapacitated geropsychiatric patients. The implications are important. If it is proper to force geropsychiatric patients into treatment with a durable power of attorney, then facilities that do not allow this practice are leaving many patients without needed inpatient treatment. Conversely, if it is unethical or illegal to use a power of attorney to forcibly admit patients, then significant numbers of geropsychiatric patients' rights are being violated.
Acknowledgments
The authors thank Beth Reichman for funding the purchase of the American Hospital Association list of psychiatric inpatient facilities in the United States.