Fish contains high concentrations of omega-3 polyunsaturated fatty acids, in particular docosahexaenoic acid (DHA). Because DHA is required for optimal neuronal function but is derived solely from dietary sources (
1), it has been proposed that infrequent dietary intake of fish may increase predisposition to depressive illnesses.
Estimates of Paleolithic diets and the diets of evolutionary adaptation, which may be considered optimal for brain development and function, indicate that human beings evolved consuming diets containing equivalent proportions of omega-3 fatty acids and omega-6 fats. Corn and soy seed oils, which are rich in omega-6 fats, were not available in abundance during human evolution but have become prevalent in modern Western diets in the past 100 years and have lowered the ratio of omega-3 to omega-6 to about 1:25 (
2). During the past century, the prevalence of major depression has increased worldwide.
Consistent with these observations, recent studies of depressed patients have reported depletions of plasma or cell membrane omega-3 polyunsaturated fatty acids (
3,
4). Furthermore, a cross-national comparison revealed a 50-fold variation in the annual prevalence of major depression, with higher prevalence rates strongly predicted by lower fish consumption (
5). In addition, in a recent double-blind, placebo-controlled trial involving 30 patients with bipolar affective disorder, omega-3 supplements along with usual treatment had a significant beneficial effect on symptoms (
6).
The purpose of our cross-sectional study was to examine the hypothesized association between fish consumption and depressive symptoms in a large random sample of the population of Finland. In the areas of the country surveyed, dietary fish comes from thousands of lakes and from the Baltic Sea.
Methods
A large survey of cardiovascular risk factors among Finnish adults was carried out in 1992 in two coastal and two lakeside areas. A random sample of persons between the ages of 25 and 64 was drawn from the National Population Register for each of the four areas. Details of the survey procedures and other measurements have been described elsewhere (
7).
The total sample size for the study was about 8,000. The initial mailed questionnaire included 132 health-related questions. Respondents returned the completed questionnaires to local health centers, where their responses were checked during a medical examination. Participants born between the 12th and the last day of each month were chosen as a subsample for the study addressing psychosocial factors (N=5,105).
After some clinical measurements, this subsample was given another questionnaire that included psychosocial measures. Participants were instructed to complete the questionnaire at home and return it by mail. The total response rate in this subsample was 67 percent (N=3,403). Another 199 persons were excluded from the study because of missing data on some variables. The remaining 3,204 subjects constituted our sample population.
The level of depressive symptoms was estimated with the 21-item Beck Depression Inventory (BDI) (
8). The BDI score ranges from 0 to 63. According to established guidelines, we considered scores below 10 to indicate no depressive symptoms or minimal depressive symptoms; 10 to 18, mild symptoms; 19 to 29, moderate symptoms; and 30 to 63, severe symptoms. For bivariate analyses, we dichotomized the BDI scores to normal mood (scores of 0 to 9) and mild to severe depressive symptoms (scores of 10 to 63). Cronbach's alpha for the BDI was .87, indicating good reliability.
Fish consumption was assessed with a frequency question with six response options: "How often do you usually eat fish or fish meals? Please consider the last six months." Responses were 1, less than once a month or never; 2, once or twice a month; 3, once a week; 4, twice a week; 5, almost daily; and 6, once a day or more often. Respondents who selected 1 or 2 were considered infrequent fish consumers.
All statistical analyses were conducted with the SAS/STAT software program. A hierarchical logistic regression analysis, with all the covariates forced into the model before the fish consumption variable was entered, was used to estimate the association between depressive symptoms and fish consumption.
Results
On the basis of the BDI scores, 20 percent of the study subjects (N=647) had mild depressive symptoms, 6.3 percent (N=201) had moderate symptoms, and 1.5 percent (N=48) had severe symptoms. Nearly two-thirds of the respondents (64 percent, N=2,053) reported eating fish or fish meals once or twice a week, 6.3 percent (N=201) ate fish daily or almost daily, and about 30 percent (N=950) consumed fish once or twice a month or less often.
At the bivariate level, mild to severe depressive symptoms were more prevalent among women who were infrequent fish consumers (those who ate fish less than once a week) than among women who were frequent fish consumers (more than once a week) (34.2 percent versus 27.0 percent; χ2=9.05, df=1, p<.01). Among men a similar trend was observed (28.5 percent versus 25.9 percent), but the results were not statistically significant.
Bivariate analyses showed that compared with frequent fish consumers, infrequent fish consumers were younger on average, physically less active, and less obese, and they were more likely to have a lower serum total cholesterol concentration, to be unmarried, to smoke, and to drink large amounts of coffee. Higher age, unmarried status, unemployment, smoking, lower levels of physical activity, greater degree of obesity, low level of education, and higher serum cholesterol concentration were associated with depressive symptoms at the bivariate level.
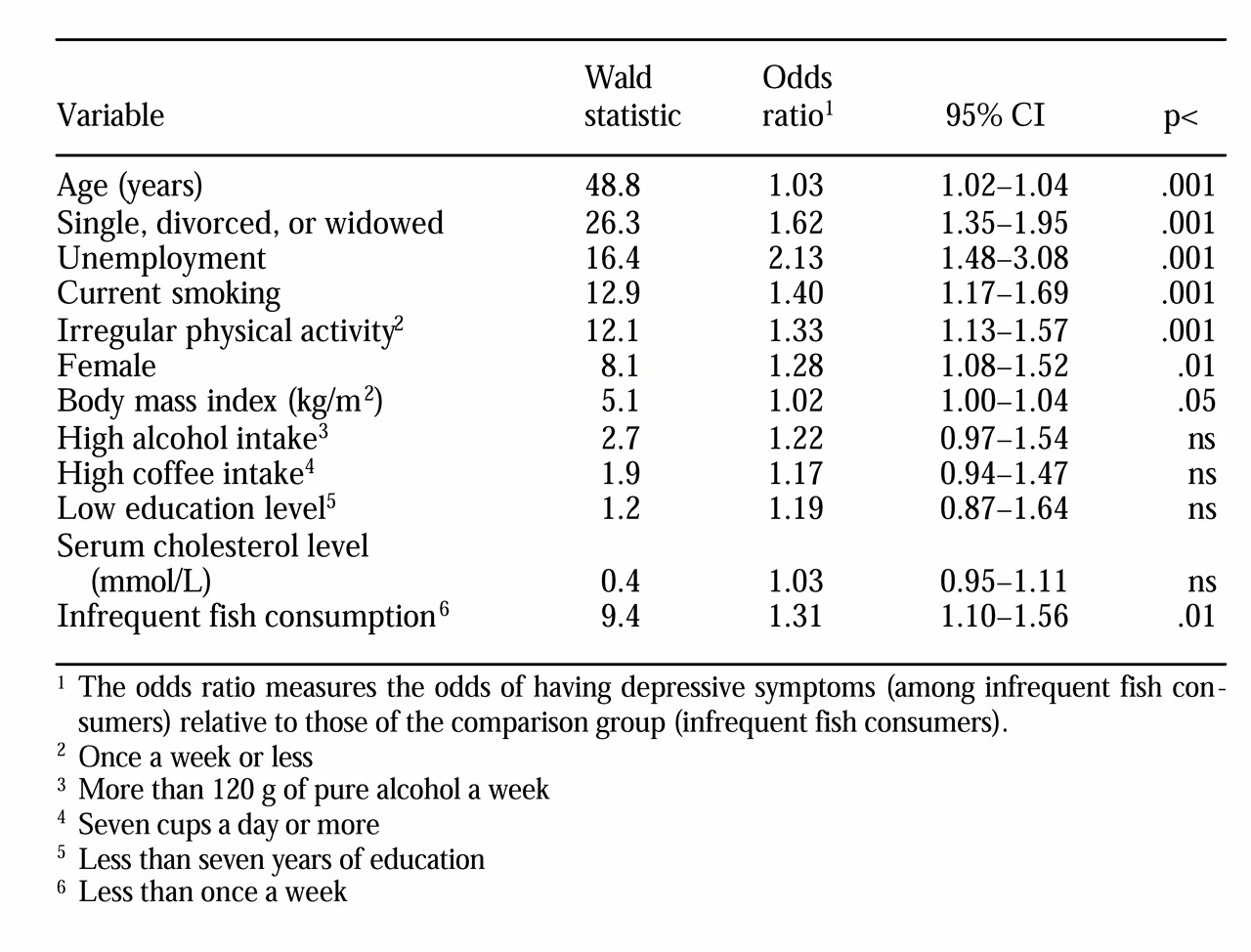
Table 1 presents the results of the multiple logistic regression analysis with potential confounders. Infrequent fish consumption was independently associated with depressive symptoms in the hierarchical logistic model. The likelihood of having mild to severe depression was 31 percent higher among infrequent fish consumers than among frequent consumers (odds ratio=1.31, 95 percent confidence interval=1.10 to 1.56, p<.01). When the analysis examined men and women separately, depressive symptoms were significantly associated with infrequent fish consumption among women (OR=1.40, 95% CI=1.11 to 1.78, p<.01) but not among men.
Discussion and conclusions
Our results showed a relatively powerful and independent association between fish consumption and depressive symptoms in this population sample of 3,402 Finnish adults; the strength of the association was especially impressive among women. The reason for the gender difference is unclear.
Fish and seafood are the major source of omega-3 fatty acids in the human diet. Thus infrequent consumption of fish could mean a low intake of omega-3 fatty acids and an elevated risk of depression. The findings reported here are consistent with cross-national comparisons of fish consumption and prevalence rates of depression and with direct tissue quantification of omega-3 fat concentrations among patients with depression.
Because of the large sample, the study did not include structured diagnostic interviews, such as the Structured Clinical Interview for DSM, or objective assessments of depressive symptoms, such as the Hamilton Depression Rating Scale. Use of these measures would have strengthened the findings.
We estimated the fish consumption with a food-frequency questionnaire, not with a food diary, which is a relative limitation of this study. However, use of a food frequency questionnaire to assess whether a person is eating a prudent diet that contains fish and other seafood has been shown to have reasonable validity (
9).
One mechanism linking fish consumption and depression may be the regulation of serotonergic nervous system function. Lower serotonergic activity has been well established in the pathophysiology of depression. High cerebrospinal fluid concentrations of 5-hydroxy-indoleacetic acid, a metabolite of serotonin and an indicator of brain serotonin turnover, have been shown to be associated with high plasma concentrations of omega-3 polyunsaturated fatty acids among healthy subjects (
10).
The findings reported here do not show any causal linkage. Large-scale intervention trials are needed before dietary recommendations to increase fish consumption or omega-3 polyunsaturated fat intake are applied to psychiatric patients or people in the general population.