The importance of improving outcomes for persons who have serious mental disorders is increasingly acknowledged, and outcomes are being conceptualized more broadly to include not only symptoms but also functioning. Because effectiveness research often uses lay interviewers to collect data in nonclinical community settings, brief self-report instruments are especially needed. This paper describes the psychometric properties of a scale that was developed to assess instrumental functioning in a population of homeless persons. Instrumental functioning, which is only one of many domains of functioning, refers to an individual's ability to effectively negotiate daily activities in his or her environment or community.
Although functional impairment and disability are central to the diagnosis of mental disorders, instruments for assessing these outcomes are often cumbersome and costly. Many instruments that are useful in clinical efficacy studies—such as the Global Assessment of Functioning (GAF) (
1)—are designed for clinician raters and require knowledge of the patient's clinical status over substantial periods. Other instruments —more readily completed by lay interviewers, such as the Social Adjustment Scale (
2)—are long and were designed to evaluate several domains of functioning, such as role, interpersonal, and instrumental functioning.
Newer measures of functioning and well-being, such as the 36-item Short-Form Health Survey (SF-36) (
3), may prove valuable for global comparisons of populations with and without mental illness. However, these measures are generic by design; they may not detect change, particularly in small samples, and they may not contain items that are especially relevant to populations with serious mental illnesses. The six-item Brief Instrumental Functioning Scale (BIFS) was designed to be a brief, oral self-report and to be administered by trained lay interviewers rather than experienced clinicians.
The BIFS items ask respondents whether they can perform six activities entirely by themselves: take medications as prescribed by a physician, fill out an application for benefits such as food stamps, keep track of or budget their money, use city buses to get where they want to go, set up a job interview by telephone, and find an attorney to help them with a legal problem. Respondents answer that they can do the activity by themselves, that they need help, or that they do not know whether they can do the activity by themselves. The BIFS is scored by assigning one point for each activity that respondents report being able to do by themselves. Items checked "don't know" are considered to be activities with which the respondent would need help.
Methods
A sample of 1,533 homeless adults in Los Angeles was selected for participation through probability sampling of shelters, soup kitchens, and city streets between October 1990 and September 1991 (
4). Complete baseline data were available for 1,509 of these, who were included in the baseline sample in the analyses. A panel of 520 individuals was selected from the initial sample for follow-up every two months over the course of 15 months. This panel was designed such that half the subjects met the criteria for serious mental illness and half did not; within these strata, the subjects were randomly selected from the baseline sample. Complete two-month follow-up data were available for 330 of the panel of 520, who were included in the follow-up sample in the analyses.
Instruments used at baseline included the BIFS, sections of the Diagnostic Interview Schedule (DIS) for the
DSM-III-R (
5), and sections of the SF-36 related to physical functioning and perceived global health. The instruments used during the follow-up assessments included sections of the Specific Level of Functioning Scale (SLOF) (
6) about personal care skills, social functioning, and community living skills as well as the GAF (
7). The GAF and the SLOF were scored by the same interviewers who conducted the structured interviews. Acceptable interrater agreement was established through the use of ratings on vignettes.
Participants were considered to have chronic mental illness if they met DIS criteria for lifetime schizophrenia, unless they had not had any symptoms in three years, and for lifetime affective disorder, unless their episodes fell outside of the DIS severity criteria, they had had only a single episode, or they had had no episode in three years.
Because the options for the item responses were binary, polychoric correlations were used to estimate the interitem relations. The unidimensionality of the scale was assessed with confirmatory factor analysis (
7) with the EQS program (BMPD Statistical Software, Los Angeles). We used confirmatory factor analysis to test the hypothesis that items on the BIFS measure a single construct—instrumental functioning—and to estimate internal consistency by using McDonald's method (
8). Pearson's correlation coefficients between baseline and follow-up were used to estimate stability. To assess convergent validity, zero-order correlations were used to compare scores on the BIFS with other measures of functioning. Discriminant validity was assessed by a comparison of scores on the BIFS across the four diagnostic groups of study participants.
Results
Of the 1,509 study participants, 1,011 (67 percent) were men. The participants ranged in age from 18 to 77 years (mean±SD=37±12.9 years). A total of 905 of the participants (60 percent) were black, 302 (20 percent) were white, and 302 (20 percent) were of other races. The mean±SD income for the previous 30 days was $230±$120. A total of 1,086 (72 percent) of the participants had at least a high school education. The 330 participants in the follow-up sample were not significantly different from the baseline sample in age, sex, income, or education.
Of the 1,509 participants, 432 (28.6 percent) had no mental illness, 766 (50.8 percent) had substance dependence only, 70 (4.6 percent) had serious mental illness only, and 241 (16 percent) had both serious mental illness and substance dependence.
Mean±SD scores on the BIFS ranged from 5.30±1.19 for participants who had no mental illness to 4.95±1.12 for those who had both a mental illness and substance dependence (F=4.43, df=1, 508, p≤.004). Interitem polychoric correlations were substantial and significant (p<.01), ranging from .35 to .71 at baseline. Because variables were not normally distributed, the generalized least-squares method was used to obtain the confirmatory factor analysis model parameters. The Yuan-Bentler corrected asymptomatic generalized least-squares chi square statistic (
9) was significant (χ
2=422, df=9, p<.01). The descriptive fit indexes (Tucker-Lewis index=.996, bootstrap-corrected comparative fit index=1.00) (
10) strongly supported the unidimensionality of the scale. The standardized factor loadings for individual items ranged from .60 to .88. The instrumental functioning factor accounted for 52.3 percent of the total variance. The lower-bound internal consistency was high (.86), as estimated from the confirmatory factor analysis solution.
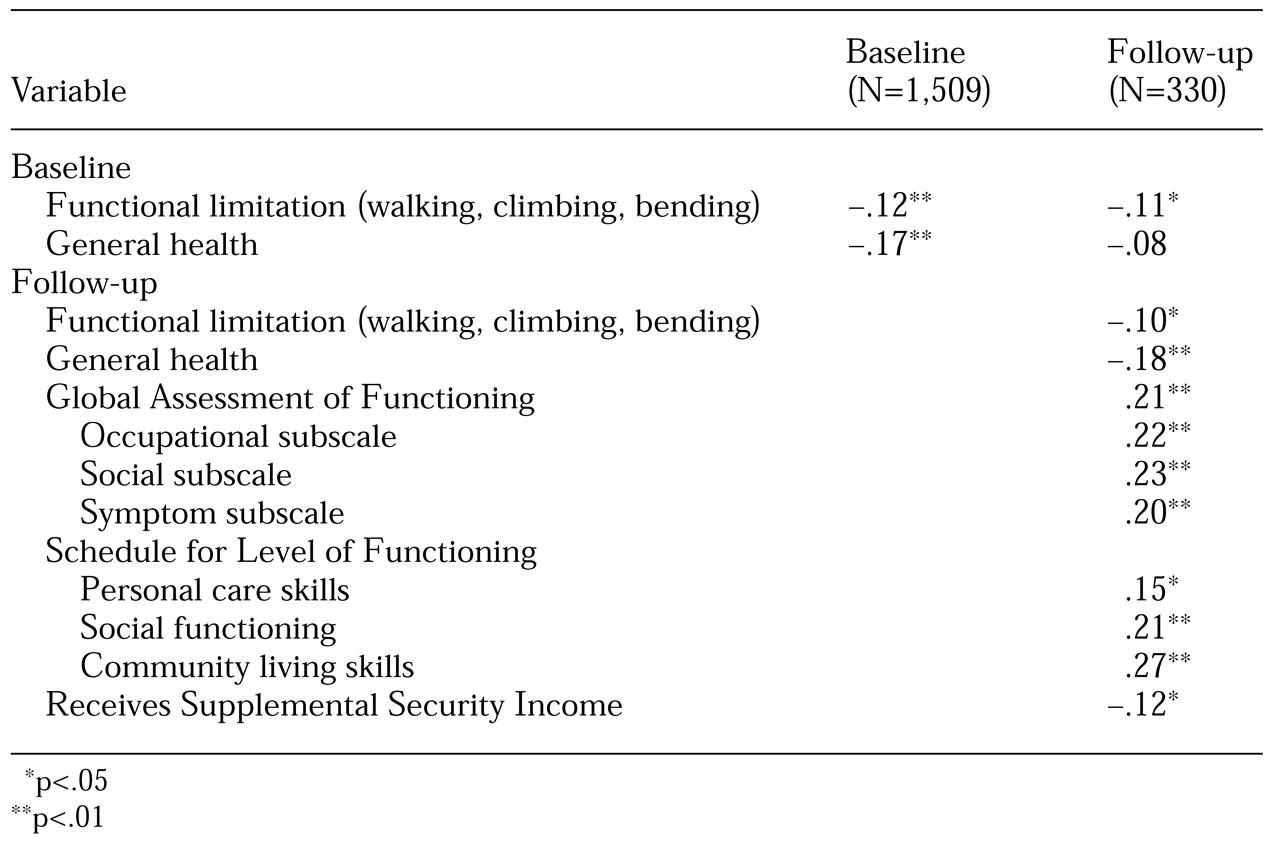
Table 1 shows correlations between the BIFS and other instruments at baseline and follow-up. Higher (better) scores on the BIFS were inversely correlated with more functional limitations and poorer general health. Better scores were positively correlated with higher (better) scores on the GAF and on the SLOF. Although the magnitude of correlation was not high, correlations were highest for instruments that assess aspects of functioning that are most congruent with instrumental functioning—social and community living skills. For the panel of 330, the stability coefficient was high (.60), indicating that scores on the BIFS did not change markedly between baseline and follow-up.
Discussion and conclusions
Measuring the functioning of individuals in nonclinical settings remains a challenge. The BIFS was designed to assess the narrow but clinically important domain of instrumental functioning among homeless persons and persons with mental illness. The BIFS proved to be a unidimensional scale with good stability. The high stability coefficient substantiates the impression of many clinicians working in psychosocial rehabilitation settings who find that without targeted interventions, an individual's functioning does not change markedly over time. However, an alternative explanation is that the BIFS in its current format is not highly sensitive to change.
Comparisons of the BIFS with other instruments that assess functioning yielded significant correlations in the directions expected, but the discriminant validity of the BIFS was not as robust as we had hoped. However, in multivariate models that predict exit from homelessness, the BIFS was the only measure that effectively discriminated between participants who did and did not have mental illness (unpublished data, Koegel P, 1996). The discriminant validity of the scale may be better if covariates are taken into account or if an expanded response set is used instead of a binary one.
The brevity and the self-report format of the BIFS make the scale a feasible tool for use in nonclinical community settings in which lay interviewers collect data. Comparable scales for assessing domains of functioning in community populations of persons with serious mental disorders are needed.
Acknowledgments
This research was supported by grant RO1-MH-64121 from the National Institute of Mental Health through Rand, by the Centers for Mental Healthcare Research at the University of Arkansas for Medical Sciences, and by the South Central Mental Illness Research, Education, and Clinical Center.