Schizophrenia is a chronic mental disorder that has been described as the worst disease afflicting human beings (
1). The prevalence of schizophrenia is approximately 1 percent, yet in the United States expenditures for its treatment have been estimated to be more than 2.5 percent of the total costs of health care (
2). The total expenditures for the treatment of schizophrenia in 1994 were about $45 billion, which is more than a quarter of the total cost of treatment of all mental illnesses (
3,
4).
Atypical antipsychotics, such as risperidone and olanzapine, are increasingly being used to treat schizophrenia. Although the atypical agents cost more than conventional antipsychotics, studies have shown that risperidone and olanzapine can reduce the costs of hospitalizations (
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15,
16). It remains unclear, however, whether use of these medications can generate savings in overall health care costs and, if so, which medication would reduce costs more.
The atypical antipsychotics account for the largest budgetary expense in the central nervous system drug class in the Veterans Administration (VA) hospital system (
17). Given the high cost of these agents, the VA is interested in studying changes in health care utilization among patients for whom treatment with these agents is initiated.
The purpose of this study was to determine differences in the changes in health care utilization and costs among patients with schizophrenia in a VA population between the one-year period before treatment with risperidone or olanzapine was initiated and the one-year period afterward.
Methods
Study design
This was a retrospective comparative database analysis of health care utilization and cost among patients with schizophrenia who had never been treated with atypical antipsychotics and were started on treatment with risperidone or olanzapine.
The VA hospital in which this study was conducted, a multi-unit medical complex in a metropolitan-suburban setting, comprises four physically distinct entities: an acute care general hospital, an acute and extended care hospital, and two outpatient clinics. No treatment protocols for atypical antipsychotics were in use during the study period. Physicians at the VA facility were free to select any of the antipsychotic medications for their patients.
Male patients from this VA system were included in the analysis if they had an initial prescription for risperidone or olanzapine dispensed between March 1997 and March 1999; if they had been continuously enrolled in the VA system for one year before receiving the prescription and one year afterward; if they had at least one claim for services with a diagnosis of schizophrenia (defined by an ICD-9 code of 295.x) during the year before receiving the prescription; and if they had received no atypical antipsychotics during the year before receiving the prescription. Study subjects who received prescriptions for both drugs at some time during the year after treatment was initiated were assigned to the risperidone group or the olanzapine group on the basis of which drug they received first. The date of the prescription was designated as the index date, and the analysis was conducted on an intent-to-treat basis.
Outcome measures
The change in total health care and total mental health care costs between the one-year period before and the one-year period after the index date were the primary end points. Total health care costs during each of the periods before and after the index date were computed as the sum of the costs of all inpatient hospitalizations, all outpatient visits, and all medications. The difference between these sums for the periods before and after the index date was calculated for each patient.
The secondary end points for the study were the changes in several utilization and cost variables between the two periods: number of inpatient hospitalizations, mean length of stay per inpatient hospitalization, cost of inpatient hospitalizations, number of outpatient visits, cost of outpatient visits, and cost of medications.
The secondary end point measures were analyzed for both mental health care and total health care services. Mental health care services were those associated with a primary diagnosis of the following ICD-9-CM codes: 290 to 319, 332.1, 333.1, 333.7, 333.8, 333.81, 333.82, 333.90, and 333.92. Medications related to mental health care were antianxiety agents, antidepressants, antipsychotics, hypnotics, ethanolamine antihistamines, valproic acid, antiparkinsonian anticholinergics, propranolol, lithium, and carbamazepine. Total health care services and medications were defined as all services and medications used during the study period.
Data and data sources
Inpatient health care utilization data were collected from the Patient Treatment File (PTF). The PTF contains information such as demographic characteristics, length of inpatient stays, and diagnosis for each inpatient admission. Outpatient and medication utilization data were obtained from the Veterans Integrated Health Systems Technology and Architecture (VISTA). VISTA is a computerized data system containing detailed information on all outpatient visits, procedures, and prescriptions.
Calculations of costs for inpatient and outpatient health care were made according to the VA Cost Distribution Report (
18,
19). Year-specific and ward- or clinic-specific costs from the report were multiplied by units of utilization (outpatient visits and inpatient days) to calculate inpatient and outpatient costs. Emergency services and ancillary costs were included in outpatient costs. Home care and nursing home costs were not considered in this analysis. The VA Drug File was used to calculate medication costs. The medical services component of the Consumer Price Index was used to convert all costs to year 2000 dollars.
Statistical analyses
Many of the utilization and cost variables used in the calculations of our study's end points were skewed. However, because the changes in these variables between the two periods had an approximately normal distribution, parametric techniques were used.
Univariate and multivariable analysis of variance modeling techniques (ANOVA and ANCOVA) were used to compare changes in health care utilization and costs for the two treatment groups. Age, race, substance abuse status, and Chronic Disease Index scores (
20) were used as potential covariates to adjust for differences related to these variables in each multivariate model in the analysis. Correlations among the potential covariates as well as interactions between the potential covariates in their effects on the end points were examined and incorporated into the modeling process. Subsequently, all descriptive statistics, adjusted for the covariates, were calculated for each resulting ANOVA and ANCOVA model. Standard residual plots were used to check the assumptions of the models, nonconstancy of error variance, nonindependence of error terms, and nonnormality of error terms.
A two-tailed alpha of .05 was used for primary analyses (total health care and total mental health care costs). A stricter alpha level, .01, was used for analysis of secondary end points to address the problem of multiple comparisons. SAS version 6.12 and SPSS 10.0 for Windows were used for the analyses (
21,
22).
Results
A total of 325 patients in the risperidone group and 285 patients in the olanzapine group met the inclusion criteria.
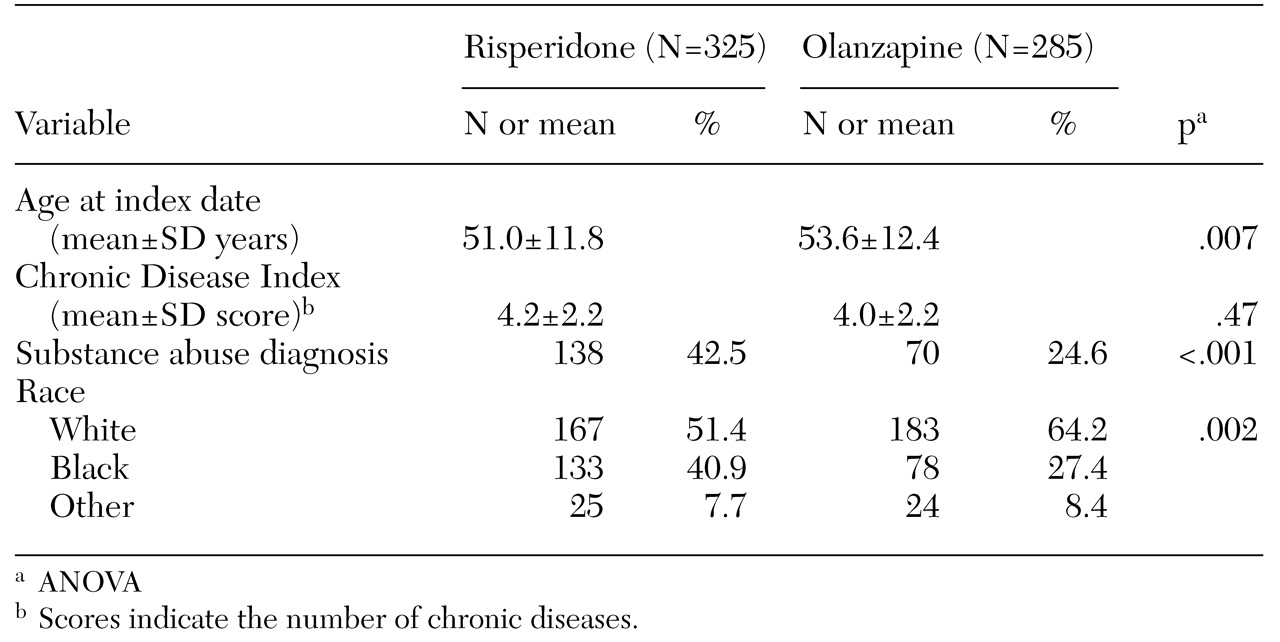
Table 1 lists some of the characteristics of the two groups. Significant differences between the groups were observed in mean age, in the proportion of substance abusers, and in racial distribution.
The mean±SD dosage for patients in the risperidone group was 3.3±1.8 mg a day (range, .5 to 9 mg a day), and the mean dosage for patients in the olanzapine group was 11.5±5.5 mg a day (range, 2.5 to 30 mg a day). The median index date was nearly identical for the two groups—April 27, 1998, for the risperidone group and May 1, 1998, for the olanzapine group. The proportion of patients who switched from their initial atypical antipsychotic to another atypical agent was similar—15 percent in the risperidone group and 12 percent in the olanzapine group, although the difference was not statistically significant.
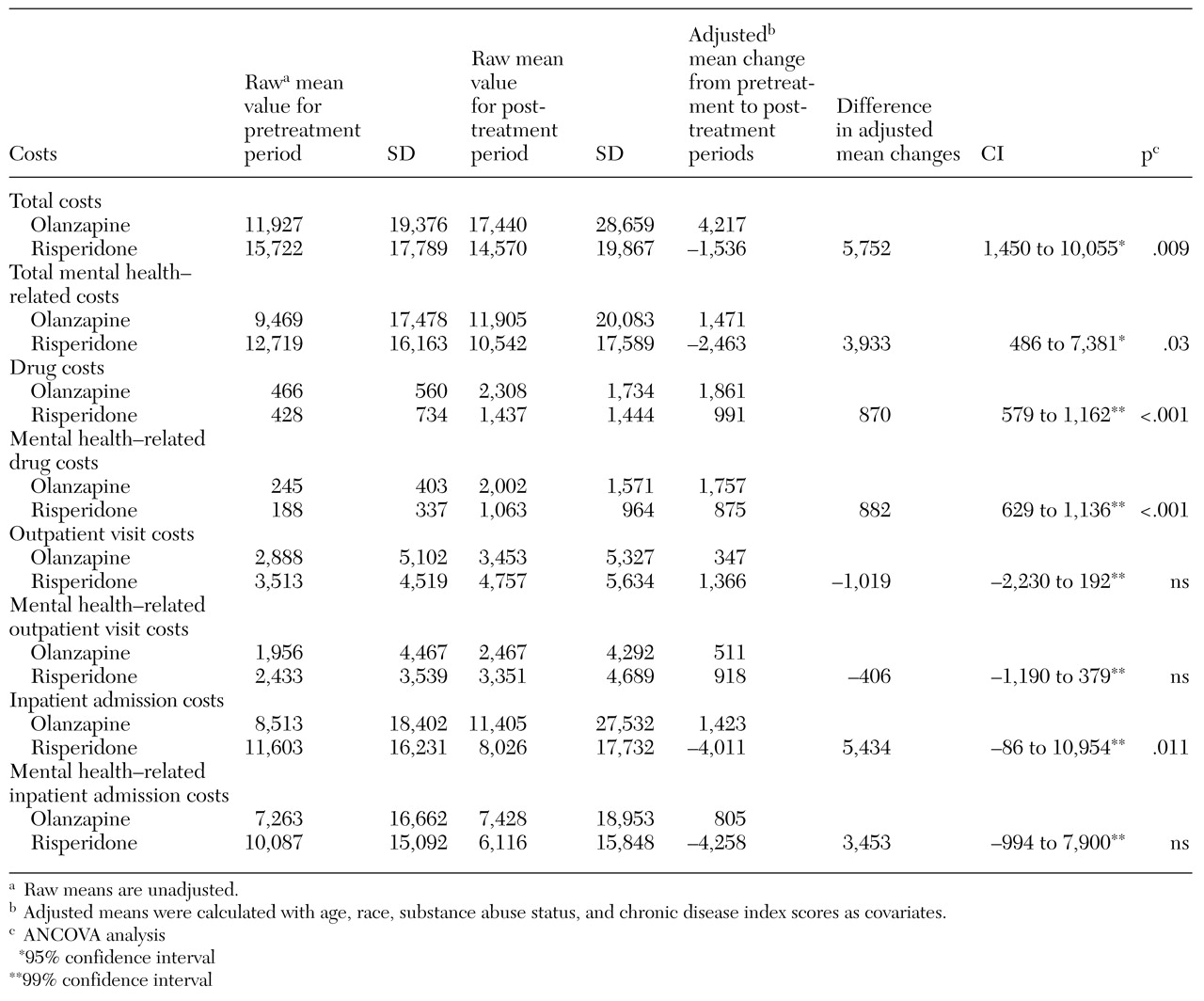
Table 2 lists the total mean costs and various mean component costs for the two groups for the years before and after initiation of treatment.
Primary end points. A statistically significant difference between the groups was observed in the change in total costs—the sum of inpatient admission costs, outpatient visit costs, and drug costs. For patients in the risperidone group, the average adjusted change in total costs between the two periods was a decrease of $1,536, whereas for those in the olanzapine group it was an increase of $4,217.
A significant difference between the groups was also observed in the change in total costs related to mental health treatment. For patients in the risperidone group, the average adjusted change between the two periods was a decrease of $2,463, whereas for those in the olanzapine group it was an increase of $1,471.
Secondary end points. Significant differences between the groups were observed in total drug costs and in mental health-related drug costs. The adjusted average change in total drug costs for patients in the risperidone group was an increase of $991, and for those in the olanzapine group it was an increase of $1,861. Likewise, the average change in mental health-related drug costs for patients in the risperidone group was an increase of $875, and for those in the olanzapine group, an increase of $1,757.
The change in length of stay for all admissions was also significantly different between the groups for the two periods. For patients in the risperidone group, average length of stay decreased by 4.4 days, whereas for those in the olanzapine group it increased by 4.3 days.
A similar pattern was observed in the costs of all admissions. For patients in the risperidone group, the average adjusted change in costs between the two periods was a decrease of $4,011, whereas for those in the olanzapine group it was an increase of $1,423. No significant differences were observed in any of the measures of mental health-related hospital admissions or in total or mental health-related outpatient visits.
Discussion
To our knowledge, this study is the largest comprehensive, retrospective comparison of the costs of treatment with risperidone and olanzapine in the VA system. This study also improved on the design of many previous studies, some of which did not have a comparison group, measured only medication costs or hospital costs, had shorter follow-up periods, or had limited sample sizes.
The results suggest that for patients with schizophrenia who are started on risperidone therapy, total health care costs and total mental health-related costs undergo a significant decrease between the one-year periods before and after the start of therapy, whereas for patients who are started on olanzapine therapy, these costs increase.
The greatest contributors to the difference in change in total health care costs were significantly greater decreases in the costs of inpatient admissions and the costs of drugs in the risperidone group than in the olanzapine group. The costs of mental health-related hospitalizations decreased for both groups. However, the magnitude of the decrease was greater for the risperidone group. Drug costs increased for both groups, but the increase was significantly greater for the olanzapine group.
The changes in the cost of inpatient admissions for the two groups were largely accounted for by differences in length of stay. Length of stay decreased for patients in the risperidone group, whereas it increased for those in the olanzapine group. This result may suggest that patients in the risperidone group experienced a higher level of treatment effectiveness or more rapid effectiveness than patients in the olanzapine group. Alternatively, it might reflect differences in the patient populations, as indicated by differences in baseline measures. However, a survey of outpatient psychiatric clinics in which use of a concomitant second antipsychotic was evaluated (
23) suggested that olanzapine and quetiapine sometimes work more slowly and that clinicians add medications to a patient's regimen while awaiting improvement. In another study, Laux and associates (
24) found that among 601 patients with no baseline differences, risperidone and olanzapine showed similar efficacy, but that the mean time to improvement in symptoms was 14 days for patients treated with risperidone and 23 days for those treated with olanzapine (p<.001). Our data support these findings.
Our results are also consistent with findings from previous studies in which increases in drug costs and decreases in hospitalization costs were observed after risperidone and olanzapine therapy were initiated (
11,
12,
13,
14,
15,
16). Our study supplements these previous findings by comparing the changes in costs between the treatment groups over a two-year period. In our study, drug costs increased to a lesser extent and hospitalization costs decreased to a greater extent for patients in the risperidone group than for those in the olanzapine group. The costs combined such that total costs decreased for the risperidone group and increased for the olanzapine group.
This study had several limitations. Initial differences in the populations, their relation to treatment assignment, and unmeasured factors could have confounded the results of the analyses. Several steps were taken to minimize these factors. The inclusion criteria, which required that patients have a diagnosis of schizophrenia in the year before the index date and that they not have taken atypical antipsychotics during the year before the index date, were designed to protect against historical bias. In addition, in our statistical analysis we attempted to control for differences in the initial severity of illness by using covariates such as the Chronic Disease Index and whether or not the patient had a diagnosis of substance abuse.
Post hoc analysis of the pretreatment period revealed a higher mean cost of all health care services for patients in the risperidone group ($15,721) than for those in the olanzapine group ($11,927). The major factor in this difference was use of substance abuse services, which was significantly higher in the risperidone group than in the olanzapine group, indicating that it made sense to use substance abuse as a covariate. An attempt was made to use costs in the pretreatment period as an additional covariate, but collinearity of this factor with other covariates precluded its inclusion in the statistical model. The selection of change from pretreatment period values as an outcome measure in itself allowed for adjustment of individual pretreatment period costs.
These efforts notwithstanding, historical bias could have influenced the results. Unmeasured factors, such as adherence to the medication regimen, the treating physician's preference of medication and other treatment options, multiple health insurance coverage, severity or duration of illness, and severity of comorbid conditions, also could have had a confounding effect. Whether these results are generalizable to other VA facilities or to non-VA settings is also unknown.
Comorbid substance abuse among people with schizophrenia has been associated with a variety of poorer outcomes, including a higher incidence of hallucinations and delusions (
25,
26,
27), a greater risk of violent behavior (
28), housing instability, homelessness, medical problems, poor money management (
29), and greater use of crisis-oriented services that result in higher costs of care (
30). Comorbid substance abuse has also been associated with noncompliance with treatment (
31) and with relapse (
32). Gupta and colleagues (
33) ensured compliance with decanoate neuroleptics and still found that patients with schizophrenia and substance abuse had significantly higher inpatient readmission rates than nonabusers. In a study by Hoff and Rosenheck (
34), dual diagnosis was associated with a significantly greater total cost of care, which was primarily explained by greater use of outpatient psychiatric and substance abuse services. Thus the reduction in mean total costs that we observed in the risperidone group may be even more impressive in the face of a higher rate of substance abuse in this group than in the olanzapine group.
The VA Cost Distribution Report, which was the basis of all inpatient and outpatient cost calculations in this study, reports average cost per day of stays for inpatient departments and average cost per visit for outpatient clinics for each year. Using year-specific and ward- or clinic-specific cost estimates allowed for more accurate analysis of actual resource utilization than using fixed costs. Given that costs may vary over time in any given ward or clinic, it is appropriate to account for this variation.
Conclusions
For patients with schizophrenia in the Cleveland VA system who had not previously been treated with atypical antipsychotics, total health care costs between the year before and the year after initiation of therapy with atypical antipsychotics underwent a significant decline for patients treated with risperidone therapy and a significant increase for those treated with olanzapine. The main contributors to this effect were declines in the costs of inpatient hospitalizations and of medications for patients taking risperidone. The declines in the cost of hospitalizations for this group were large enough to produce overall cost savings. Overall costs for the olanzapine group increased.
Because of limitations associated with retrospective database analyses, such as historical bias and uncontrolled confounding factors, additional studies are needed to substantiate these results. However, this study adds to the evidence that initiation of risperidone therapy for patients with schizophrenia may decrease total health care expenditures.
Acknowledgments
This study was funded by Janssen Pharmaceutica.