Demands for administrative activity in substance abuse treatment organizations stem from a variety of sources, reflecting the fragmented and complex financing environment in this sector (
1,
2,
3). Treatment organizations may be involved in initial and ongoing accreditation and licensing processes. Many treatment providers must deal with increasing demands to document care processes and conduct preauthorizations, ongoing utilization review, and follow-up reviews for managed care clients (
4,
5,
6,
7). Some treatment providers must manage the complex requirements of various external funding sources—for example, state governments and private agencies such as United Way. In recent years, the relatively simple activities of hiring staff and billing for services have become more complex as a result of a larger number of federal employment requirements, patient information privacy concerns covered in the Health Insurance Portability and Accountability Act (HIPAA), and the greater sophistication of provider, payer, and government information systems. In sum, substance abuse treatment providers must manage the "hassle factor" of providing treatment services.
At the same time, substance abuse treatment organizations are facing increasing pressures to operate as efficiently as possible. There is a growing emphasis on outcome measurement and cost reduction as treatment organizations must survive with fewer available resources and negotiate with managed care firms, state governments, and other agencies (
2,
4,
5,
6). Treatment providers must do more with less and document their efforts to do so to myriad external and internal stakeholders. These parallel trends raise issues about whether and how administrative burden affects providers' ability to deliver substance abuse treatment services in an efficient and productive manner.
The purpose of our research was to examine whether and how administrative burden is associated with organizational efficiency and productivity in outpatient substance abuse treatment organizations. We expected that administrative burden would have a direct, negative relationship with efficiency in regard to operational expenses. As treatment providers experience greater administrative demands, they incur greater expenses, such as overhead, information technology, professional fees for consultants, and other operating expenses to provide the same volume of service.
Administrative burden may also be systematically linked to the efficiency of the human resource component of the organization. The need for intensive face-to-face therapy sessions and the relative "low-tech" nature of substance abuse treatment means that salaries are typically the largest expense category in this sector. Organizations must hire additional staff to meet increasing administrative requirements, including clerical and management workers and information systems experts. In addition, units may need to hire additional treatment staff if such staff must meet administrative demands in addition to providing therapy for clients. Thus we expected that a greater administrative burden would result in the need for additional salary expenses to deliver the same volume of therapy to clients.
In many substance abuse treatment organizations, highly trained and well-educated treatment staff may be called upon to manage some portion of administrative requirements. Overall, this approach reduces the productivity of outpatient substance abuse treatment provider organizations, because it means that fewer treatment sessions are provided for each available unit of staff. We therefore expected that administrative burden would have a direct, negative relationship with the number of treatment sessions provided by each full-time-equivalent (FTE) staff member in this sector.
We examined these relationships between administrative burden, efficiency, and productivity in a large national sample of outpatient substance abuse treatment providers, controlling for potential alternative explanations, including managed care activity, accreditation status, organization size, staff mix, ownership, affiliation, and client mix.
Methods
We used data from two nationally representative samples of outpatient substance abuse treatment units that were surveyed in 1995 and 2000 as part of the National Drug Abuse Treatment System Survey (NDATSS). The NDATSS is a longitudinal study of outpatient substance treatment units conducted by the University of Michigan's Institute for Social Research (ISR). In the NDATSS, an outpatient substance abuse treatment unit is formally defined as a physical facility with resources dedicated primarily (more than 50 percent) to treating persons with substance abuse problems on a nonresidential basis.
The details of the sampling method and procedures of the NDATSS have been described previously (
8,
9). Briefly, the NDATSS uses a mixed panel design, which combines elements from panel and cross-sectional designs. Units are selected for participation from a sampling frame of the most complete list of the nation's outpatient substance abuse treatment units, compiled by ISR (
8,
9). In both 1995 and 2000, each participating organization was assigned a weight that accounted for probability of entry into the study and for nonresponse (
8,
9). The weights were applied to the two waves to make the data nationally representative.
The NDATSS is a telephone survey of the administrative director and clinical supervisor at each outpatient substance abuse treatment unit. Directors provided information about the unit's control status, environment, finances, parent organizations, and managed care arrangements. Clinical supervisors provided information about staff, clients, treatment practices, and services provided.
After screening and nonresponse, 618 organizations completed interviews in 1995 and 745 in 2000, for response rates of 88 percent and 89 percent, respectively. Several steps were followed to produce reliable and valid telephone survey data, including elaborate interviewer training, two pretests, extensive checks for consistency within and between sections of the survey instrument, and, when necessary, recontacting of respondents (
10).
Measures
Operating efficiency, measured by operating expenses per therapy hour, reflects the nonsalary expenses per therapy hour provided by the unit. Such expenses include overhead, rent, supplies, professional fees, and other expenses. Therapy hours reflect the total number of hours of individual, group, and family therapy provided by the unit during the most recent complete fiscal year. Higher values of operating expenses per therapy hour suggest lower levels of operating efficiency. Salary efficiency, measured by salary and wage expenses per therapy hour, reflects the total staff salary and wages per therapy hours provided by the unit. Salary and wages are reported for all types of employees of the unit—for example, full-time and part-time. Therapy hours are the total number of hours of individual, group, and family therapy provided by the unit during the most recent complete fiscal year. Higher values of salary and wage expenses per therapy hour suggest lower salary efficiency.
Productivity, measured by treatment sessions per FTE, is a ratio of the total number of substance abuse treatment sessions to the total of the unit's FTE staff. Therapy sessions include individual, group, and family modalities. FTEs are calculated on the basis of the total number of hours worked by all employees divided by 40 hours per week. The unit director provided the information for the three dependent variables. Higher values of treatment sessions per FTE suggest higher levels of productivity.
The independent variables in our analyses included number of administrative hours, number of clerical hours, percentage of clients enrolled in managed care programs, number of years of experience with managed care, whether the organization was accredited by the Joint Commission on Accreditation of Healthcare Organizations (JCAHO), organizational size, percentage of professional staff (those with a master's degree, a Ph.D., or an M.D.), whether the organization was affiliated with a hospital or a mental health center, ownership (private for-profit, private not-for-profit, or public), methadone status, percentage of clients who were unemployed, and percentage of clients with dual diagnoses.
Analytic strategy
We used the generalized estimating equations (GEE) method of Zeger and Liang (
11) to examine the relationships of interest, test for changes over time, and account for within-unit correlation over time. An important feature of the GEE method is that parameter estimates have the same interpretation as parameters estimated with generalized linear models for cross-sectional data. Also, the GEE method does not require the correct specification of the within-unit correlation matrix. Longitudinal studies such as these have the advantage that each unit essentially serves as its own control (
12).
Three dependent variables were considered: operating expenses per therapy hour, salary and wages per therapy hour, and number of treatment sessions per treatment staff member. The 1995 variables for operating expenses per therapy hour and salary and wages per therapy hour were adjusted to the 1999-2000 data by using the consumer price index to account for inflation. Because of the skewed nature of the dependent variables, a logarithm transformation of each one was taken.
Two models were fitted for each dependent variable. The base model included the two predictors of administrative burden and covariates representing potential alternative explanations of the relationship between administrative burden and efficiency. In addition, we included a variable representing time (2000 compared with 1995).
In the interaction model, we entered interaction terms representing the joint effects of each administrative burden variable with each control variable and the joint effects of time and each administrative burden variable. Only interaction terms that were significant were included in the final interaction model.
Results
Descriptive results
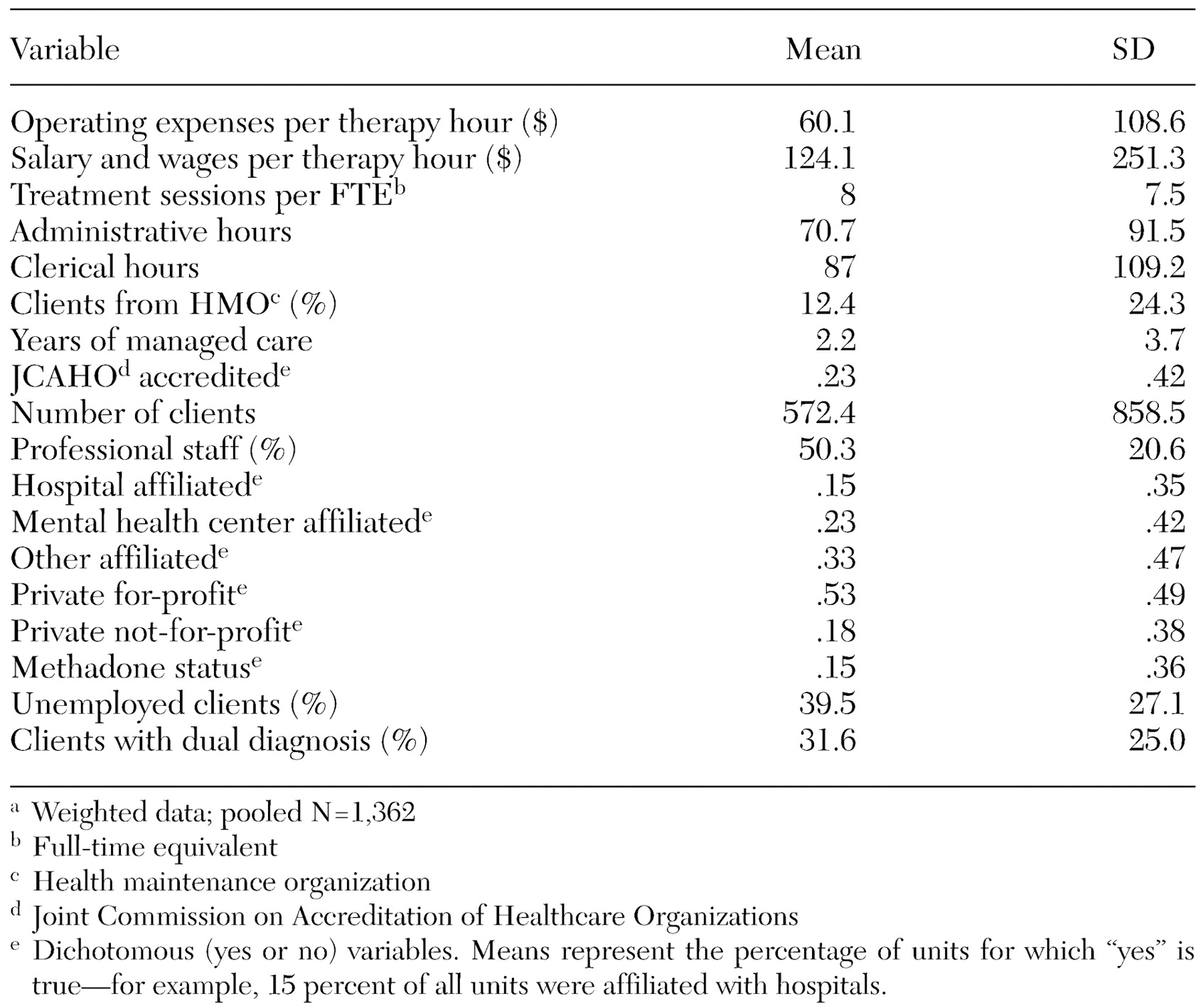
Means and standard deviations for each study variable are shown in
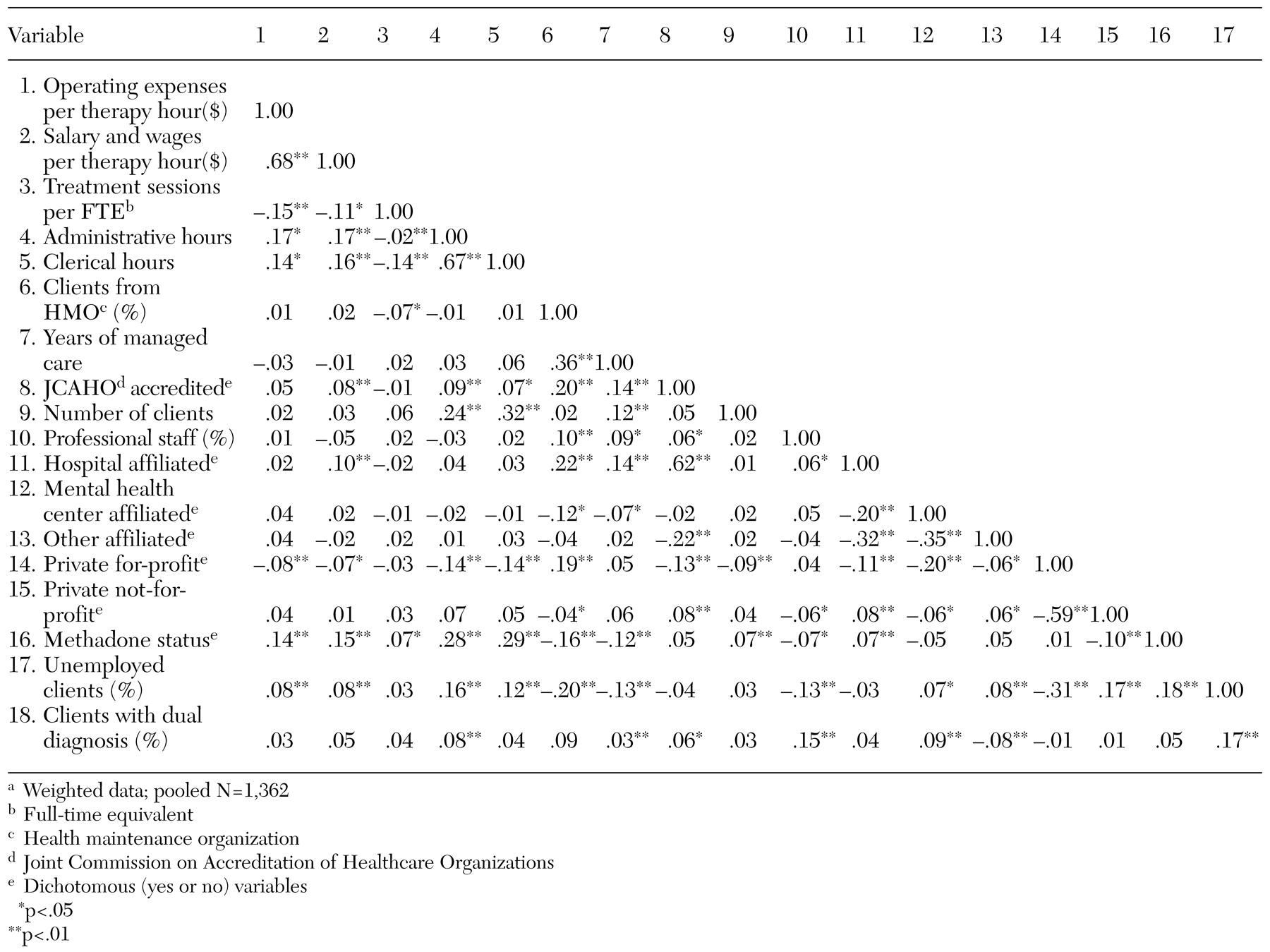
Table 1; bivariate correlations between variables are shown in
Table 2. Our weighted and adjusted national sample data showed that, on average, to produce one hour of substance abuse treatment therapy, outpatient substance abuse treatment organizations incurred about $60 of nonsalary operating expenses and about $124 in salaries and wages. (These amounts reflect the mean across both periods—1995 and 2000—adjusted to 1999 dollars). For each FTE in the organization (including all treatment and support staff), approximately eight treatment sessions were delivered each week. The average weekly administrative burden consisted of about 71 hours of administrative work and almost 87 hours of clerical work.
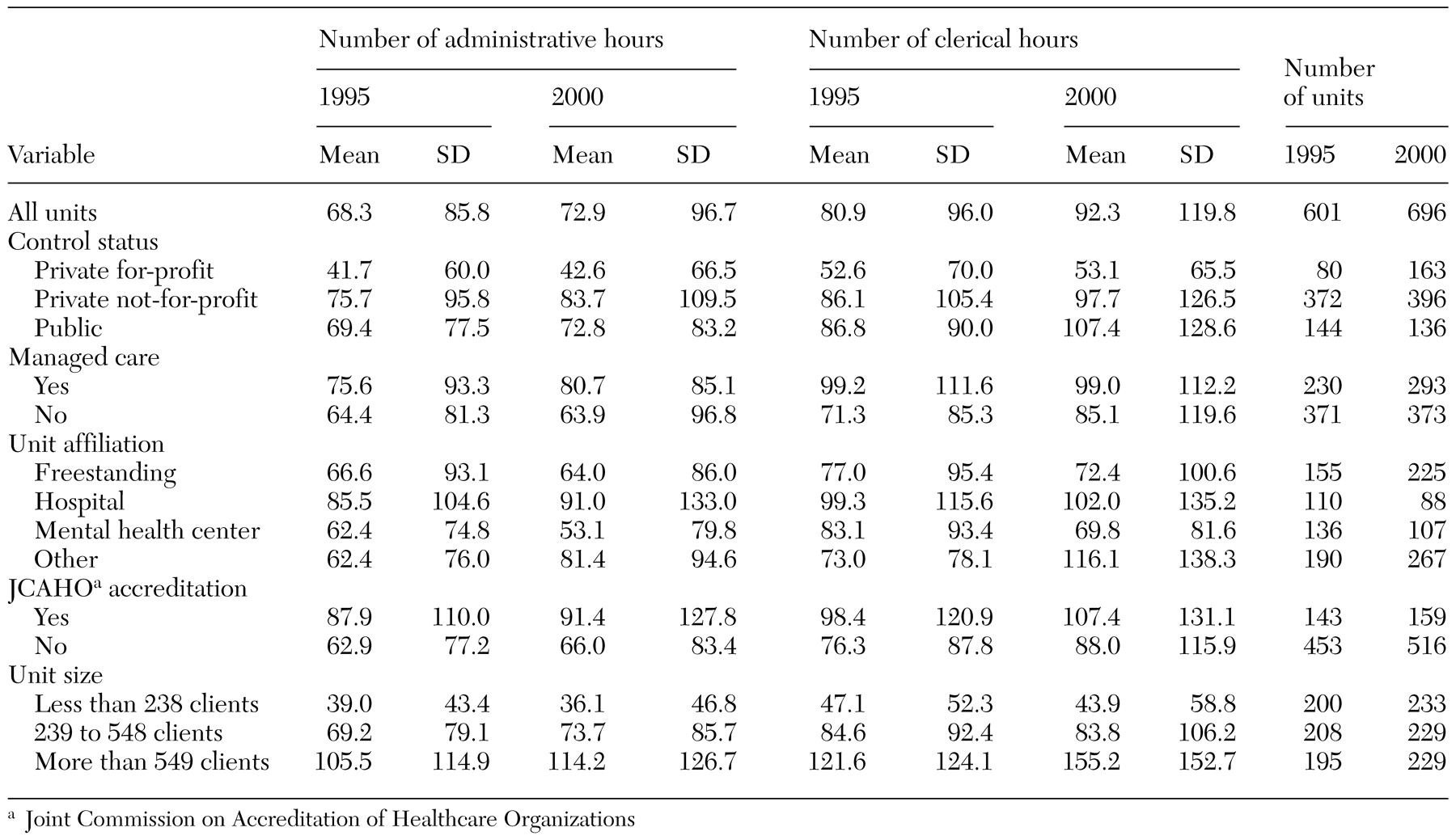
More detailed information on administrative burden is presented in
Table 3. Weighted data are presented for each period (1995 and 2000) and for several organizational categories. Our national data suggest that the average number of administrative hours and the average number of clerical hours increased between 1995 and 2000, the largest increase being for clerical hours (from 81 in 1995 to 92 in 2000). We found variation in the level of administrative burden experienced by units in different categories of control status, affiliation, accreditation, and size. For example, private not-for-profit units reported the lowest average number of administrative hours (around 40) and clerical hours (around 53). Furthermore, these organizations experienced no growth in administrative burden over the study period. By contrast, private for-profit and public units reported greater average administrative burden and large increases—especially for the number of clerical hours per week—between 1995 and 2000.
Freestanding units and units affiliated with mental health centers reported less administrative burden than their hospital-affiliated and other affiliated counterparts. In addition, both mental health center-affiliated and freestanding units showed decreasing trends in the number of administrative and clerical hours from 1995 to 2000. Hospital-affiliated units reported the highest levels of burden in 1995, and other affiliated units reported significantly more clerical hours in 2000.
Units with managed care activity reported, on average, more administrative and clerical hours than units that did not participate in managed care. Similarly, units that were accredited by JCAHO experienced greater administrative burden than those that were not accredited. Although units involved in managed care experienced little growth in burden over the study period, the average number of clerical hours increased for accredited units between 1995 and 2000 (from 98 hours to 107 hours).
As expected, larger units reported a greater administrative burden than smaller units. Furthermore, the smallest organizations experienced slight decreases in the average number of administrative and clerical hours over the study period.
Regression results
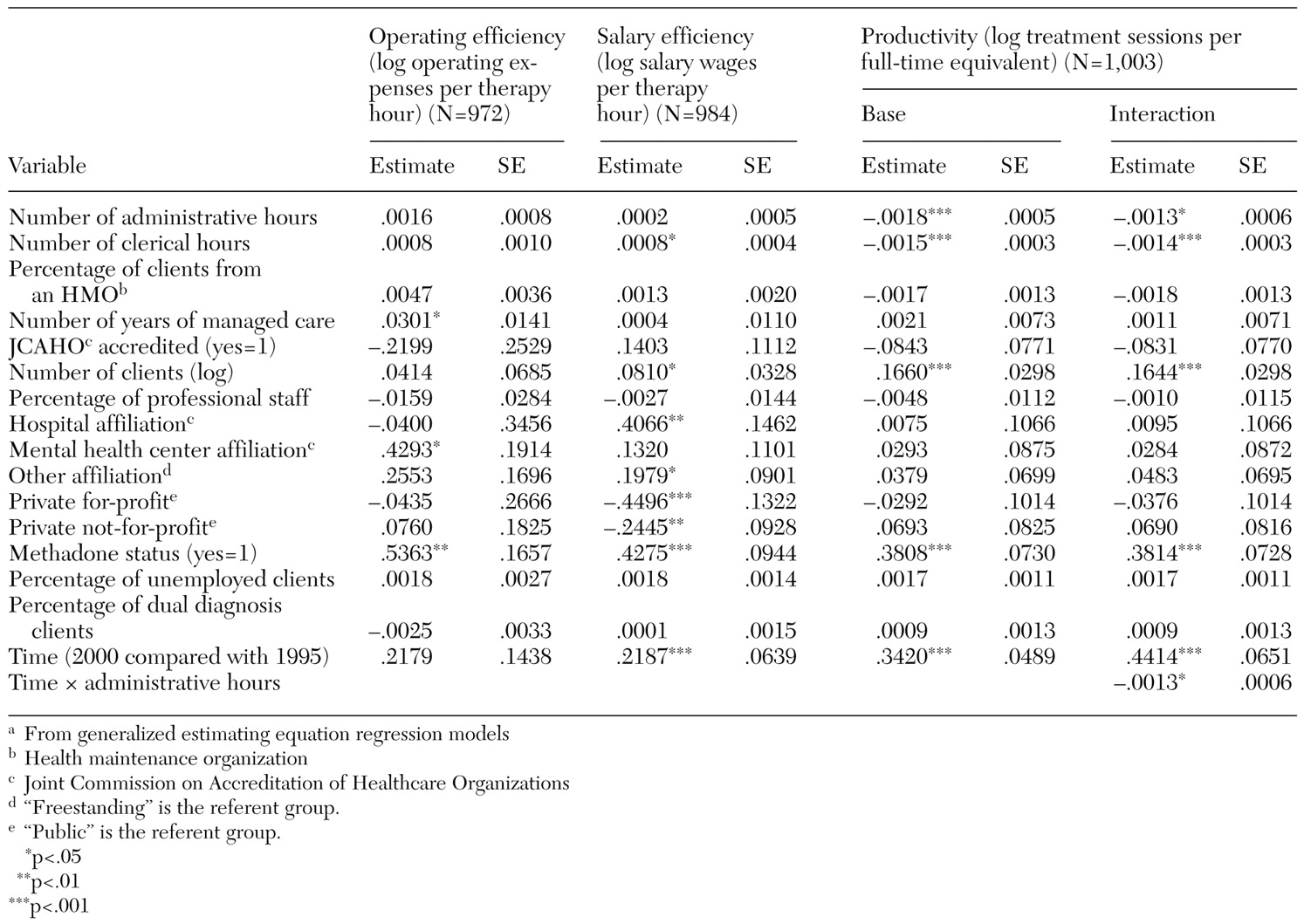
Administrative burden. Parameter estimates and standard errors from the regression models are presented in
Table 4. For ease of discussion, exponentiated coefficients are provided in the text.
Overall, after controlling for various organizational characteristics, we found support for our prediction that administrative burden would have negative relationships with organizational efficiency and productivity. However, differences in the pattern of findings were noted for different types of administrative burden (administrative versus clerical) and for different types of organizational performance. Specifically, there was some evidence that the number of administrative hours had a positive relationship with operating expenses per therapy hour, a negative relationship with treatment sessions per FTE (coefficient of .998, p<.001), and no relationship with salary efficiency. Thus a greater number of administrative hours was associated with lower operating efficiency but higher productivity. The relationship between the number of administrative hours and productivity was more pronounced in 2000 than in 1995. By contrast, the number of clerical hours had a positive relationship with salary and wages per therapy hour (1.001, p<.05), a negative relationship with treatment sessions per FTE (.999, p<.001), and no relationship with operating expenses per therapy hour. That is, a larger number of clerical hours was associated with lower salary efficiency and productivity.
Control variables. We found evidence of systematic relationships among our organizational control variables and the efficiency and productivity of outpatient substance abuse treatment units. For example, although no relationship was observed between managed care penetration and any measure of efficiency or productivity, the number of years of managed care experience had a significant, positive relationship with operating expenses per therapy hour (coefficient of 1.031, p<.05). Thus greater experience with managed care was associated with lower operating efficiency in this sector.
Overall, the results were mixed regarding the relationship between organizational size and efficiency and productivity. On one hand, we saw a positive relationship between organizational size (number of clients) and operating expenses per therapy hour (coefficient of 1.084, p<.05). Thus larger units were less efficient in terms of operating expenses. At the same time, larger organizations may get more sessions from each FTE, as evidenced by a large and positive relationship with productivity (1.79, p<.001).
Significant, positive effects were noted for methadone treatment status and operating expenses per therapy hour (coefficient of 1.710, p<.01), salary and wages per therapy hour (1.533, p<.001), and treatment sessions per FTE (1.464, p<.001). Thus methadone units were less efficient—in terms of both operations and salary expenses—but more productive than units that did not provide methadone treatment.
Differences were observed in the relationship of various affiliation categories and the three measures of organizational performance. Specifically, compared with freestanding units, hospital-affiliated units and units affiliated with other types of organizations had greater salary expenses per therapy hour (coefficients of 1.502, p<.01 and 1.219, p<.05, respectively), whereas mental health center-affiliated units had greater operating expenses per therapy hour (1.536, p<.05). That is, both hospital-affiliated and mental health center-affiliated units were less efficient on at least one dimension than freestanding units.
We found that, compared with public units, private not-for-profit and private for-profit units had lower salary expenses per therapy hour (coefficients of .783, p<.01 and .638, p<.001, respectively). Thus private units experienced greater salary efficiency than public units. We found no evidence of relationships between client-mix variables and efficiency and productivity in our sample.
Discussion and conclusions
Four main themes emerged from our analysis. First, although administrative and clerical functions are a necessary aspect of any business, when "the hassle factor" becomes too great, it threatens the performance and viability of treatment organizations. Our research is the first of its kind to comprehensively examine the size of and trends in administrative burden in the outpatient substance abuse treatment system. To the extent that treatment organizations cannot absorb increased administrative activities into their ongoing operations, they may need to cut programs, restrict access to existing programs, or reconsider participation in various funding programs, including public and private managed care plans. Similarly, when paperwork, telephone contact, and billing issues become too great, only the most dedicated providers and the most motivated patients will see them through. Thus an unintended consequence of various oversight activities in the substance abuse treatment sector could be that treatment units offer fewer programs and, ultimately, fewer clients are served.
Second, we uncovered different relationships for various types of burden and different types of organizational performance. These findings have implications for managing treatment organizations and setting oversight policies. Treatment unit directors may need to evaluate more closely the administrative requirements that are more complex and require management attention (or example, interpreting the staff requirements of a managed care contract and hiring the appropriate mix of professional staff to meet those requirements) from those that involve only documentation and clerical functions (for example, providing evidence of staffing compliance to the managed care firm). There may be creative, innovative, and nontraditional solutions for dealing with these different types of activities. For example, outside specialty business firms may be more effective and efficient at the billing process. Professional consultation may be needed for the initial design and implementation of appropriate documentation and information system flows, and existing staff may need to be cross-trained. The strategic, proactive management of administrative components may be an important part of ongoing and effective leadership in substance abuse treatment organizations. Furthermore, managing complex and onerous administrative issues may be difficult for clinician-managers who may take on management roles with little formal management training or education.
As public and private insurance firms and government agencies establish oversight policies and requirements, the administrative burden for providers should be considered at multiple levels. Important questions should be raised: What types of oversight functions can be automated by using information technology? What activities are not vital for treatment planning or staff credentialing? Can treatment organizations be reevaluated less frequently for accreditation, licensure, or managed care participation? Are there systems of oversight that involve fewer administrative hassles for providers? As best practices are established in today's environment, consideration must be given to their potential effects on organizational efficiency and productivity. Although efficiency and productivity may be far less important aspects of organizational performance than treatment quality, effectiveness, and the long-term outcomes of care, the "hassle factor" associated with treatment provision is typically "unfunded" or is expected to be provided "in kind" in most formal and informal programs and contractual relationships.
Finally, we have provided some evidence that as treatment organizations face administrative burden, they may be shifting resources away from the provision of care to dealing with administrative requirements. To the extent that treatment staff spend less time actually providing services to clients, or if treatment organizations are unable to simultaneously manage treatment and administrative functions, administrative burden may directly affect treatment quality and outcomes. In addition, there may be other, negative implications for treatment organizations and treatment staff. Recent studies have shown treatment professionals' frustration in dealing with the many requirements of managed care and the potential detrimental effects on treatment processes (
13,
14,
15). If treatment professionals become dissatisfied working in an environment characterized by more administrative burden, they may leave the sector, choose not to participate in various public and private programs (
16), or make similar exit decisions. Retaining highly trained, well-qualified treatment professionals is a key challenge for treatment organizations and may become even more difficult if current trends in administrative burden continue.
The "hassle factor" associated with providing substance abuse treatment services has many potential implications. Our study has provided evidence of the overall extent of administrative burden in the outpatient substance abuse treatment sector and the variety of ways in which administrative burden is associated with poorer organizational performance in substance abuse treatment organizations.
Acknowledgment
This research was supported by grants 5R01-DA03272 and 5R01-DA087231 from the National Institute on Drug Abuse.