Participants
The data for the study were derived from two sources: the original Schizophrenia Patient Outcomes Research Team (PORT) study, which examined usual care in a random sample of persons with schizophrenia in Ohio and Georgia (
10), and a Department of Veterans Affairs (VA) PORT extension, which followed a parallel sampling strategy to provide an expanded VA-specific comparison group to the original study (
11), for a total sample of 1,076 (
10,
11).
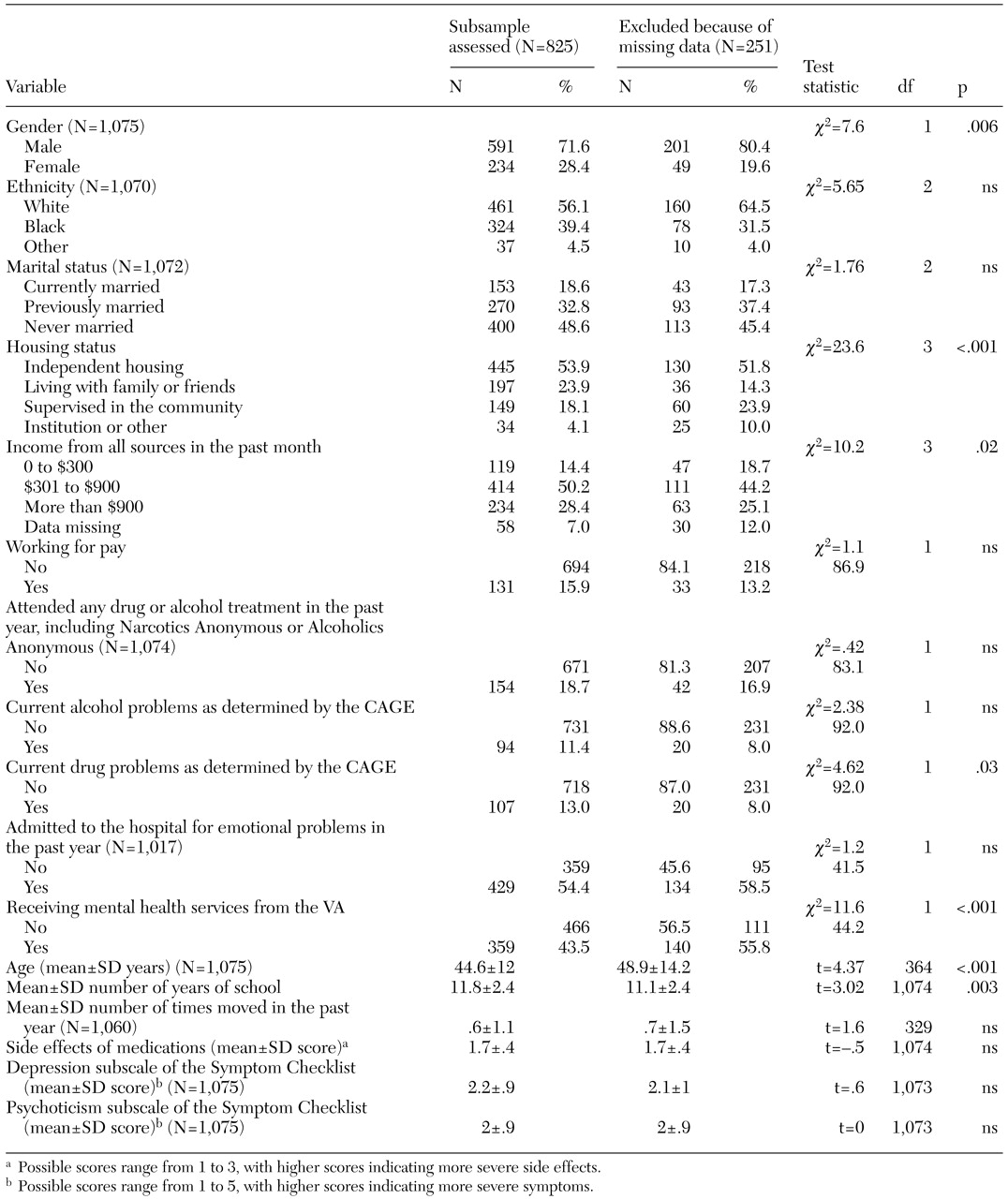
Client interviews were conducted from December 1994 through March 1996. All participants were aged 18 years or older, were legally competent, spoke English, had a working clinical diagnosis of schizophrenia, and provided written informed consent as approved by the applicable institutional review boards. A total of 825 persons were included in the analyses: 577 (70 percent) from the original PORT study and 248 (30 percent) from the VA extension; 251 participants were excluded from the analyses because of missing data on one of the main dependent variables. As can be seen from
Table 1, several significant differences were found between the participants for whom data were missing and the other participants. The participants with complete data were more likely to be male, to have current drug problems, to be younger, to have more education, and to be receiving VA services. The two groups also differed in housing status and income.
Sociodemographic and clinical measures
Information about demographic characteristics (age, gender, ethnicity, education, income, and employment status), history of mental health treatment, and housing instability (number of times the participant had moved in the previous year) were self-reported through interview.
Symptoms of mental illness were measured with a shortened version (30 items) of the Symptom Checklist 90 (
12). Two subscales—depression and psychotic symptoms—were created by averaging the appropriate items; thus subscale scores ranged from 1, not at all, to 5, extremely. Internal consistency (Cronbach's alpha) was good at .90 for the depression subscale and .86 for the psychotic symptoms subscale.
We used the four-item CAGE (
13) as well as an analogue to the CAGE as dichotomous measures of current alcohol and drug problems. Each CAGE item is rated as absent or present; thus scores for each scale range from a low of zero to a high of 4. We used the standard cutoff of 2 to indicate the presence of current problems (
14).
Several questions assessed participants' perceptions of side effects of psychotropic medications and were averaged to create a total score ranging from 1 to 3. Cronbach's alpha for this scale was .72.
We also included questions about the use of various mental health, legal, and rehabilitation services in the year before the assessment.
The recovery orientation domains that served as dependent variables in our analyses are based on a previously derived empirical conceptualization of recovery orientation (
9). To create this measure, we first selected items from the PORT client survey that met two criteria. First, the item reflected a theme that is prominently used in the existing recovery literature (
3,
15,
16). Second, the item was a self-reported measure of a personal attitude or disposition. We then randomly divided the PORT participants into two separate and distinct samples. We conducted a series of principal-components and confirmatory-factor analyses, using the first sample for hypothesis generation and the second for model confirmation, and ultimately derived a four-factor model.
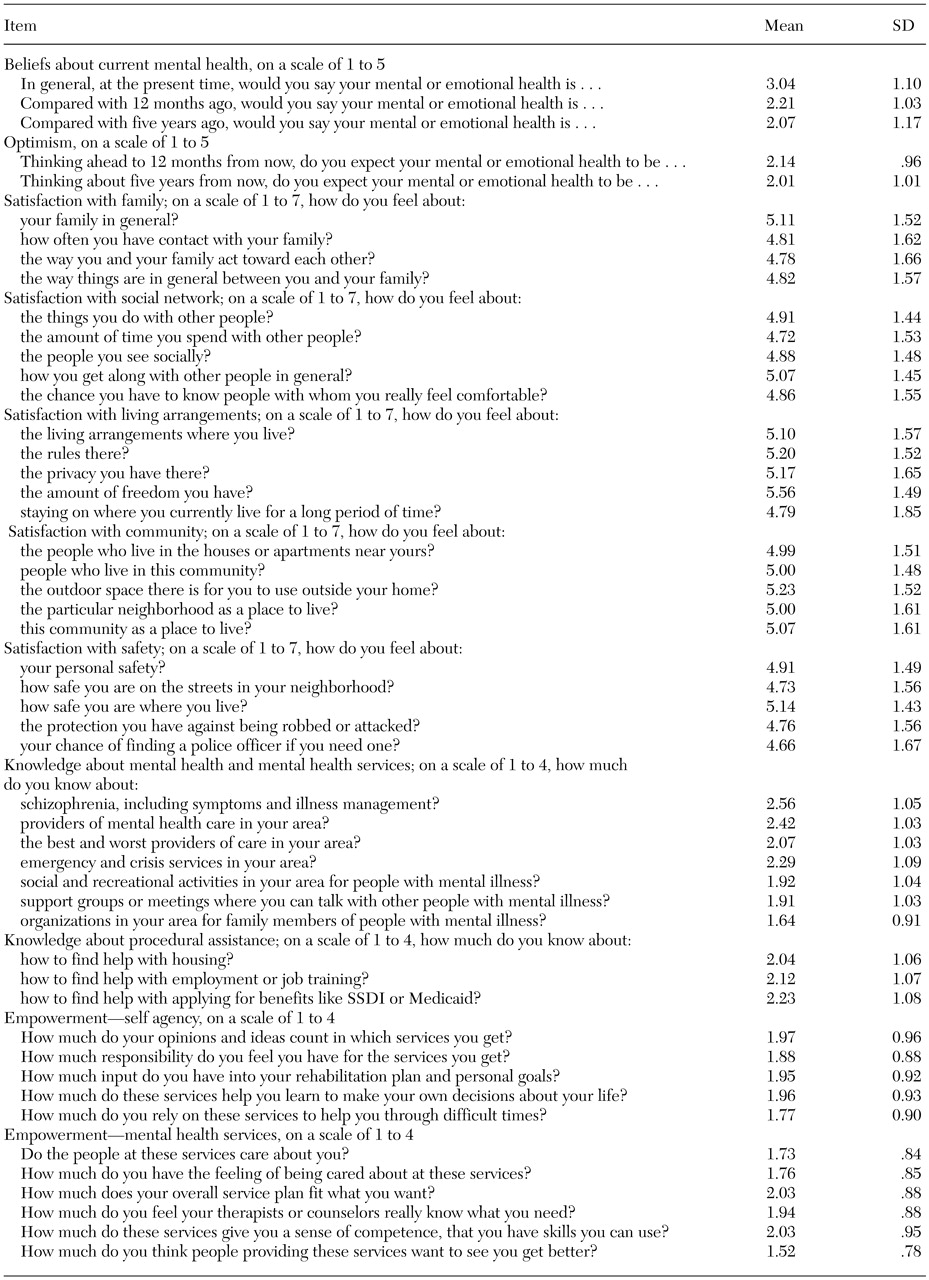
The fit indexes were good in both samples: sample 2 yielded a comparative fit index of .92, and a root mean square residual of .054; the confirmatory analyses repeated on the first data set yielded a comparative fit index of .94 and a root mean square residual of .066 (
9). The four dimensions of recovery orientation identified through this procedure were life satisfaction, hope and optimism, perceived knowledge about mental illness and services, and empowerment. The individual items from each domain and their means are listed in
Table 2. Details of these analyses are presented elsewhere (
9).
We created recovery orientation domain scores by converting item scores to Z scores and averaging the Z scores within each domain. Thus the domains all had a mean of 0 and a standard deviation of 1. Intercorrelations between the domains were small (r values ranging from .10 to .37) but significant (p<.01), which suggests that these dimensions are approximately orthogonal. Internal consistency was good, with a Cronbach's alpha of .92 for life satisfaction, .75 for hope and optimism, .86 for knowledge, and .90 for empowerment.
Results
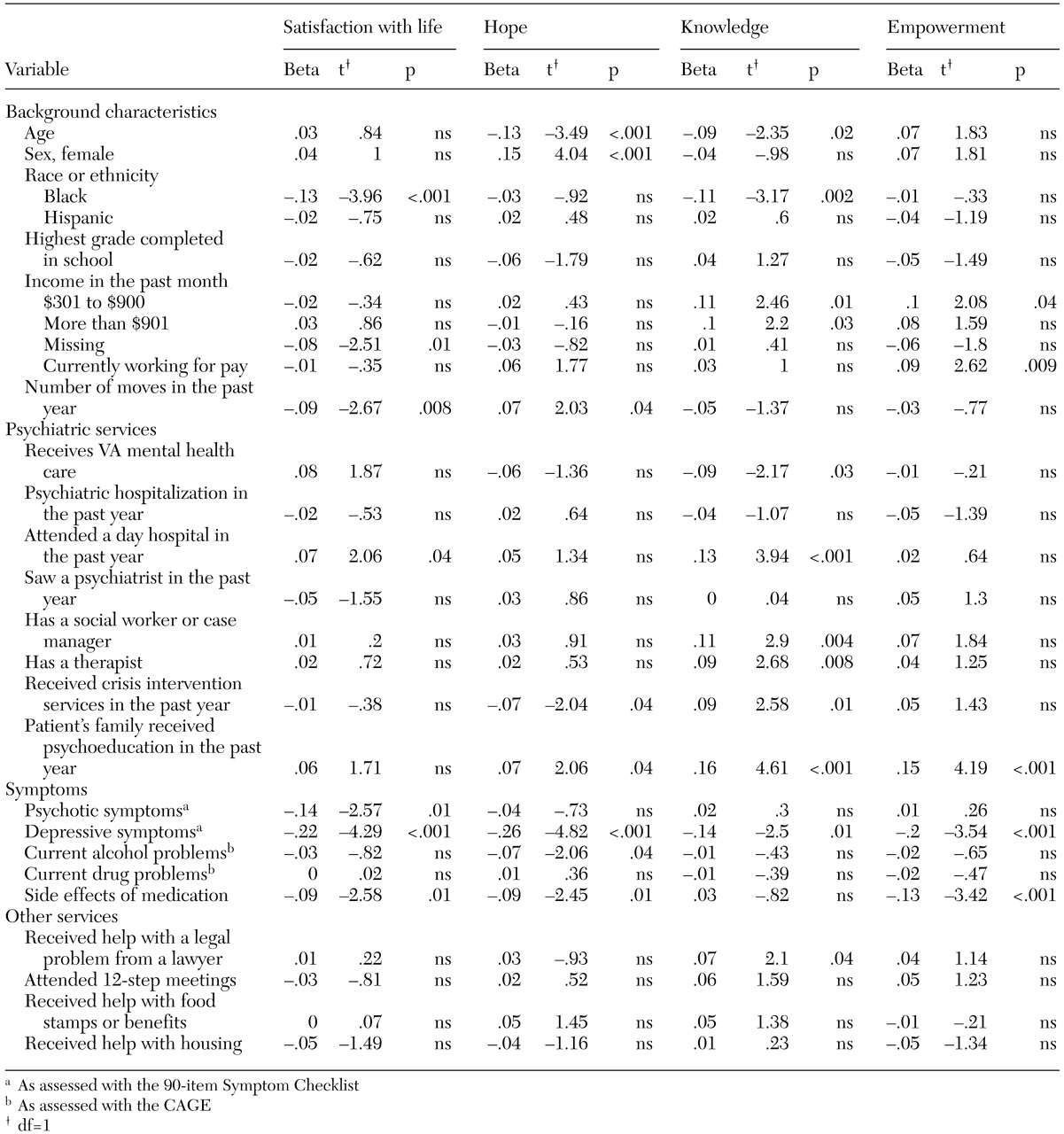
Four separate multiple regression analyses were conducted to identify associations between the four recovery orientation dimensions and client background, health status, and service use measures. The results are presented in
Table 3. In all four regression models, the strongest relationship was observed between recovery orientation and lower severity of depressive symptoms, and these associations were highly significant. Medication side effects were negatively and significantly associated with three of the four dimensions. Receipt of family psychoeducation was also strongly and positively associated with three dimensions.
General life satisfaction was significantly associated with less housing instability, fewer side effects of medications, lower severity of psychotic symptoms, attendance at a day hospital, absence of reported help with housing issues, and nonblack race or ethnicity.
Hope was significantly and positively associated with younger age, housing instability, absence of receipt of crisis intervention services, fewer side effects of medications, receipt of family psychoeducation, and female gender.
Knowledge was significantly associated with younger age, medium or high income, attendance at a day hospital, presence of a social worker or a case manager, visits to a therapist, receipt of crisis intervention services, receipt of help from a lawyer, and nonblack race or ethnicity.
Empowerment was associated with current paid employment, income of $301 to $900 in the previous month, fewer side effects of medications, and receipt of family psychoeducation.
Receipt of mental health services from the VA was significantly and negatively associated with only one measure: knowledge of mental illness and services.