Most discussions of schizophrenia start at the beginning—that is, at the first episode of the illness. Today a great deal of interest is focused on the identification of patients with schizophrenia before they manifest florid signs and symptoms. However, the development of a test with both sensitivity and specificity in identifying such patients has not yet been achieved. By and large, then, the first encounter between a clinician and a schizophrenia patient is when the first episode of psychosis occurs.
Our experience has shown that this first encounter can be a seminal event. It can lead to the patient’s engagement with treatment and to clinical improvement, or to the patient’s becoming alienated and receiving only partial, inadequate treatment for a significant period of the illness. The earlier the treatment and the more sustained it is, the better the prognosis (
1–
4). We hope in this paper to provide some clinical “pearls” for students, residents, and other clinicians who are unaccustomed to treating patients with psychosis. We present our schema for the identification, diagnosis, and stabilization of a patient experiencing a first episode of psychosis. We do not discuss subsequent acute or maintenance treatment.
Encountering the patient for the first time
There are a myriad of ways that a person experiencing a first episode of psychosis can come to our attention. Usually, the patient presents fairly soon after the first signs and symptoms appear. Some patients, however, wait years before seeing a clinician. Such delays may be due to a family bias against identifying the symptoms as part of an illness or to social and physical isolation from others, with or without profound negative symptoms that lead to the person’s becoming essentially a shut-in. The majority, however, come to the attention of a clinician within the first two years after their first symptoms appear (
1). Referrals from family, teachers, and friends are most common, but it is not unusual for patients to self-refer when they can appreciate that they have a problem and are not afraid to discuss their symptoms.
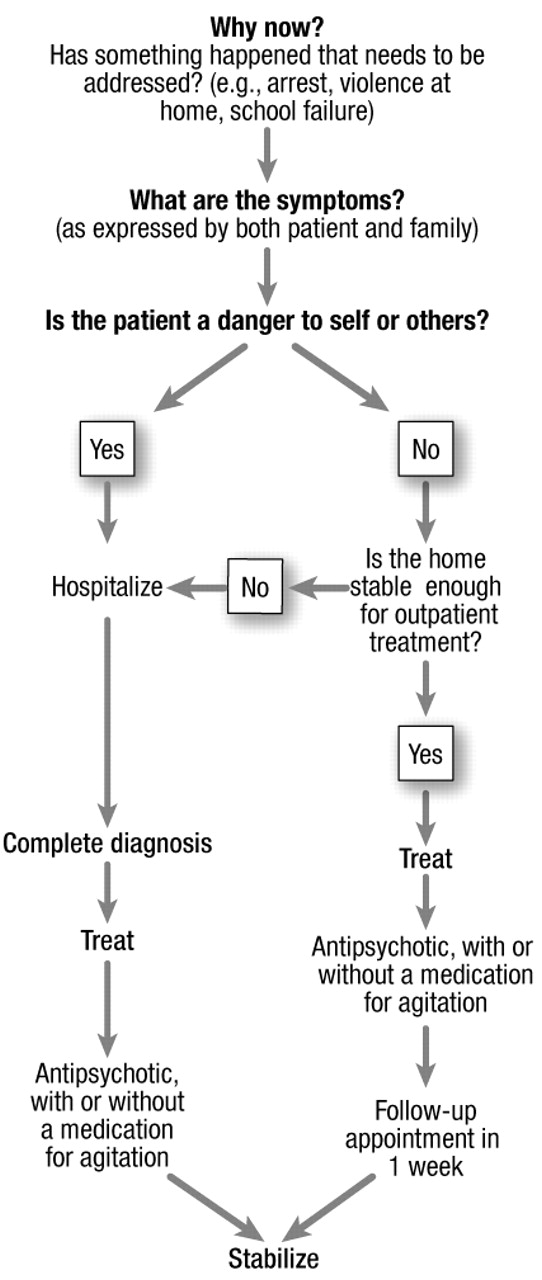
Once the patient comes in contact with a clinician, a complex set of questions and decisions must be considered and a plan determined. Figure 1 outlines a sample decisional algorithm. Safety is a primary consideration. Is the patient a danger to himself or others? With patients who are openly evasive, guarded, or paranoid, the answer may not be obvious. The clinician must ask gentle but direct questions about the patient’s thoughts about hurting himself or others. With patients who have children, it is very important to ask if they feel that they need to protect their children, even if that could mean “taking them away from this world.” If there is a strong suspicion that a patient with psychosis might harm himself or others, the patient will need to be hospitalized. A mildly psychotic patient who voices no such dangerous intents may be able to undergo outpatient treatment. Forcing patients into hospitalization when there are less restrictive options can drive them away from long-term treatment. We recommend a close follow-up for patients who are sent home after the first visit. We find that seeing them after 1 week is ideal, to allow time for the medication—usually an antipsychotic agent—to take effect. However, we let patients and their families know that they can call in earlier or return to our crisis center earlier if necessary.
A differential diagnosis must be developed at the first visit. There are many medical, toxic, and substance use causes of psychosis, and these should be listed and ruled out (Table 1). A correct working diagnosis is crucial in developing an appropriate treatment plan. For example, a psychosis due to systemic lupus erythematosus requires treatment of both the psychosis and the underlying autoimmune disorder. A working diagnosis is not always the definitive or final diagnosis, but it is informed by the evidence at hand and modified as new information is collected.
Finally, the first encounter requires a special touch with the patient’s family. A tactless pronouncement of a premature diagnosis and prognosis can confuse or even devastate the family. The first encounter can be the beginning of the family’s treatment as well as the patient’s.
The interview
There is no “best” approach to the first interview for a first-episode patient, and experienced clinicians employ a variety of techniques and styles. What all successful styles have in common is the understanding that the symptoms, diagnosis, prognosis, and treatment can all be extremely frightening for patients and their families. The true extent of the problem may present overtly, or it may unfold over the course of the interview and subsequent treatment. For the practiced clinician, the presentation is one they have seen before; the patient and family, however, may have no experience with or reference for it. Interestingly, though, as mental illnesses are increasingly brought into the open through the media, the general population is gaining some knowledge of them, especially depression, anxiety, and schizophrenia. For example, one patient who presented for the first time with extreme paranoid delusions stated, “My husband thinks I may be like that Beautiful Mind guy.”
Sometimes a patient presents alone, in which case the face-to-face interview includes only the patient. More typically, patients come with or are brought in by friends or family. The interview should include all participants, sometimes together and sometimes individually. If the patient is so disturbed that an interview is impossible, ensuring his or her safety comes first, and the clinician must rely on the family to provide the necessary information. If the patient can be engaged, asking whether he or she would feel more comfortable talking with the family present or talking alone gives the patient both respect and a sense of autonomy. At some point, the patient and the family should each have a chance to speak alone with the clinician. Families often provide a wealth of information about the onset and course of the illness. They can describe the patient’s temperament and premorbid functioning, which are critical for the differential diagnosis. Of course, patient confidentiality must be maintained as it is in any physician-patient encounter. A tricky situation that commonly arises is when the family wants to provide information but expresses a strong desire to withhold this fact from the patient. We make it clear to the family that if the information is necessary to decide whether the patient needs to be involuntarily committed, we will have to present it to the patient. A good rule of thumb is to tell families not to provide confidential information that will place the physician-patient relationship in a bind.
As in any good interview, the clinician should begin with open-ended questions and, if needed, progress to more structured and direct questions. Be mindful that if the family is present, it may be the first time they hear the patient describing his or her symptoms, and this can be a shock to the family. When patients are reluctant to speak, for whatever reason, first ask if they feel safe in the room or if they are uncomfortable having family members or other clinicians in the room. Asking leading questions can often help in getting the patient started. For example: “I know this may be a scary time for you, but I often hear from people who come here that they are hearing unusual voices in their head. Has this ever happened to you?” It can be comforting to the patient to learn that psychotic symptoms are not rare and that you have treated others with similar problems.
Most patients and families would like to have a specific diagnosis at the first interview. We think a diagnosis at that time would be premature, and we explain that any medical diagnosis requires a thorough collection of information and is best done longitudinally, not cross-sectionally. We do not even mention schizophrenia at this interview; instead we focus on symptoms, safety, and treatment. An exception may be cases in which there is a family history of schizophrenia and there have been similar presentations in other family members. The patient or family may have made the diagnosis themselves and are looking for confirmation from the psychiatrist.
The initial workup
Once all available interview and collateral information has been obtained, a decision must be made on what tests need to be done to confirm or rule out medical and neurological causes of psychosis. Table 2 lists the tests we consider for all patients at the first presentation of a new-onset psychosis. Blood work should be done early in the course of treatment, including a routine blood count and chemistry screen, thyroid function tests, and tests for sexually transmitted diseases, such as syphilis and HIV. A urine drug screen should be done at the earliest opportunity, ideally in the clinic under monitored conditions, and it should be repeated at follow-up if there is a history of illicit drug use. If there are focal neurological signs, a computed tomography scan of the brain should be done to rule out an intracranial mass or a cerebrovascular event. After the first encounter, additional testing should be considered in light of the potential yield and the cost. Further investigations might include neuropsychological testing and neurophysiological and neuroimaging examinations such as electroencephalography (EEG) and magnetic resonance imaging (MRI).
If no other cause of the psychosis can be found, the differential diagnosis shifts to primary psychiatric illnesses. We first attempt to determine whether the illness has a prominent mood component. Many families of patients with psychosis later report that the diagnosis of schizophrenia was “missed” or dismissed early on in favor of another diagnosis, such as depression or an anxiety disorder. Nearly half of patients who have a final diagnosis of schizophrenia initially present with depressive symptoms that can warrant a diagnosis of major depression (
5–
7). If the psychosis appears directly related to periods of depression and/or mania, a diagnosis of major depressive disorder with psychotic features or bipolar I disorder is considered. If it does not appear that a significant mood disorder is fueling the psychosis, then a schizophrenia-like illness is considered. If there are distinct episodes of mood symptoms and periods when the psychosis seems independent of a mood disorder, then schizoaffective disorder should be considered. It is beyond the scope of this article to discuss the diagnostic criteria of these various illnesses, but we will describe the features of schizophrenia, which is the most common diagnosis given. Table 3 lists the DSM-IV-TR criteria for schizophrenia (
8). If the symptoms of schizophrenia are met but have not been present for more than 6 months, the diagnosis of schizophreniform disorder is more appropriate, although the patient must be reevaluated after the 6-month period has passed.
Patients who do not meet the full criteria for schizophrenia—in terms of intensity or number of symptoms—pose a diagnostic and treatment challenge. These patients can be viewed as having a schizophrenia-like disorder or a schizophrenia spectrum illness and may be characterized as exhibiting odd, eccentric, or asocial behavior. They may be diagnosed with a personality disorder (e.g., schizotypal, schizoid, or paranoid personality disorder) or receive the vague “psychosis not otherwise specified” designation. Their illness may progress to meet the full diagnostic criteria, and they may receive a diagnosis of schizophrenia. However, many patients remain subsyndromal and do not develop a full presentation of schizophrenia. Unfortunately, this does not guarantee a better prognosis. In fact, many such patients are resistant to the effects of antipsychotic medications and even more resistant to accepting that they need treatment.
Prognosis
At the initial interview, inevitably the patient or the family will request some estimation of the patient’s prognosis. Determining the prognosis for patients with a first episode of psychosis is quite difficult. A prognosis requires a definitive diagnosis, which is rarely made at the first interview. Even if it appears that the diagnosis will be schizophrenia, the illness course can have a wide range of outcomes as a result of the combination of biological, environmental, and protective factors. Nevertheless, some general trends can be expected for most patients. The early course of the illness—the first 2–3 years—is often unstable, with periods of remission and relapse (
9). It is rare for a patient to experience a single psychotic episode (as in an episode diagnosed as a brief reactive psychosis) with complete return of functioning. In general, first-episode patients tend to show a greater degree of symptomatic recovery—that is, to a greater degree and more rapidly—in response to pharmacological treatment than do patients with chronic illness (
10). In fact, longitudinal studies suggest that the maximum symptomatic improvement occurs within the first 6–12 months after initial treatment (
11). Responsiveness to pharmacological treatments early in the illness course is strongly predictive of a more favorable long-term course. In the first episode, control of symptoms can be quite robust, but traces of the illness remain, often in terms of more subtle negative symptoms. Several studies have shown that prolonged untreated psychosis is associated with a lesser degree of short-term and long-term recovery and slower response to antipsychotic medication, regardless of subsequent treatment (
12–
15). Although recent studies have not replicated this finding, initiation of treatment at the first appearance of symptoms is clearly desirable and may serve as a protective factor against active pathological processes in early psychosis.
The best-studied prognosis for any psychotic disorder is that for schizophrenia (
18–
19), which carries the worst long-term prognosis. Schizophrenia is a chronic, incurable illness that remains present at varying degrees of severity throughout the person’s life. Most patients with schizophrenia (over 80%) will relapse (
16) and are likely to demonstrate a chronic course of illness characterized by frequent episodes of symptom exacerbations and relatively poor interepisode functioning, typically requiring extended treatment with antipsychotic drugs. About two-thirds of schizophrenia patients will demonstrate a moderate to very poor outcome. Table 4 lists the factors most strongly associated with a good prognosis. Unfortunately, our ability to predict which patients will be among the one-third who have a relatively good outcome is quite limited; predictors of poor outcome demonstrate greater reliability. In our experience, the prognostic factors listed in the table are helpful but not certain. Patients with the best prognostic profile can often go on to have a terrible illness course, but the reverse is less common.
Several characteristics of the onset and the early course of illness in schizophrenia can predict prognosis. Insidious onset, which occurs more commonly in males, is associated with a chronic course of illness, negative symptoms, cognitive impairment, and poor long-term outcome (
9). Substance abuse in the early course of psychosis is also associated with poor outcome (
17–
18). Affective symptoms in the context of schizophrenia have historically been regarded as a good prognostic sign. However, research has not consistently demonstrated an association between depression and outcome (
5–
6). In fact, clinicians must vigilantly assess depression in patients with recent-onset psychosis, given that depressive symptoms are correlated with suicidal ideation and behavior in this group (
19). Psychosis due to an affective disorder in general carries a better prognosis. However, some patients with affective disorders may have long-term difficulties similar to those of patients with schizophrenia.
Treatment
Although a definitive diagnosis is needed before optimal treatment can be determined, in the case of the first encounter with a patient with psychosis, immediate therapeutic intervention is necessary. The speed and aggressiveness of the treatment depends on the clinician’s assessment of the patient’s distress and danger to self or others. Even when the working diagnosis is a psychosis induced by substance use, medication may be necessary until the effects of the substance abate. If the patient is clearly a danger to self or others, most likely hospitalization will be required, or at least an extended period of observation and medication in the psychiatric emergency room.
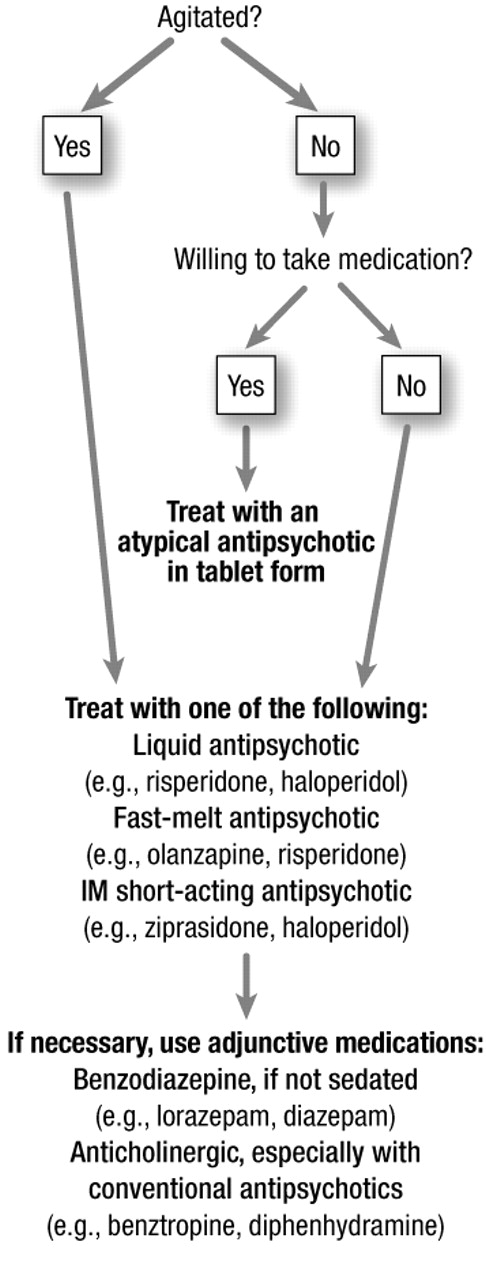
A variety of medications are available for use at the first visit. If the patient is acutely agitated, oral (in capsule or liquid form) or injectable intramuscular antipsychotics, with or without a benzodiazepine or an anticholinergic, can be used. Figure 2 presents an algorithm for the initial medication treatment of psychosis. The mainstay of treatment is the atypical antipsychotic agents, which include risperidone, olanzapine, quetiapine, ziprasidone, and aripiprazole. The efficacy of these medications was established in studies with chronic patients, but preliminary data from studies with first-episode patients appear promising (
3). All of these medications are superior to placebo and compare favorably with the conventional antipsychotics (e.g., haloperidol) (
4). They all possess the significant advantage of a lower incidence of extrapyramidal side effects—which are often distressing and thus limit dosing or compliance—than the conventional antipsychotics. Preliminary data also show that the atypical agents have a much lower rate of future tardive dyskinesia. As with all medications, the atypical antipsychotics are not without side effects. Sedation, weight gain, tachycardia, and elevation of prolactin levels are a few that have been identified.
At the first visit, the goal of treatment is to alleviate the immediate suffering and to ensure safety. While agitation can be treated in an hour, psychosis can take days, weeks, or even months. It is important to explain to patients that the medications prescribed should make them feel better quickly but that symptoms may still be present for a time. While it is not wise to dwell on side effects, since that may give patients an excuse to refuse medication, we recommend that patients be told to look out for the major immediate side effects, such as sleepiness, restlessness, and severe muscle stiffness. We often tell patients to note any unusual physical symptoms and to bring them up for discussion at the next visit.
A common question asked by patients and families is what length of time treatment will be necessary. We always state that this differs with each person and depends on the degree of response. For patients whose symptoms disappear completely with treatment, we recommend that they continue to take an antipsychotic for up to a year. Patients who remain symptomatic need to continue taking the medication. Because it is impossible to determine such outcomes at the first visit, we present a wait-and-see stance.
Conclusion
The first encounter with a clinician is a watershed for the patient with first-episode psychosis and can be a determinant of future treatment and prognosis. An experienced and reasoned approach to the patient is required, coupled with an understanding of how distressing and frightening psychosis is to patients and their families.