Patient Management Exercise for Psychosomatic Medicine
Abstract
CASE VIGNETTE
Consideration Point A:
| A1._____ | Alcohol withdrawal |
| A2._____ | Side effects from the narcotic analgesic agents |
| A3._____ | Urinary tract infection |
| A4._____ | Fat embolus from the femoral fracture |
| A5._____ | Depression or some other mood disorder, as suggested by the primary team |
VIGNETTE CONTINUES
Consideration Point B:
| B1._____ | Resume paroxetine, starting at 20 mg every evening. |
| B2._____ | Use lorazepam 0.5 mg every 6 hours as needed for restlessness. |
| B3._____ | Give a single dose of fluoxetine 20 mg. |
| B4._____ | Give haloperidol 0.5 mg orally every 8 hours as needed for agitation/irritability. |
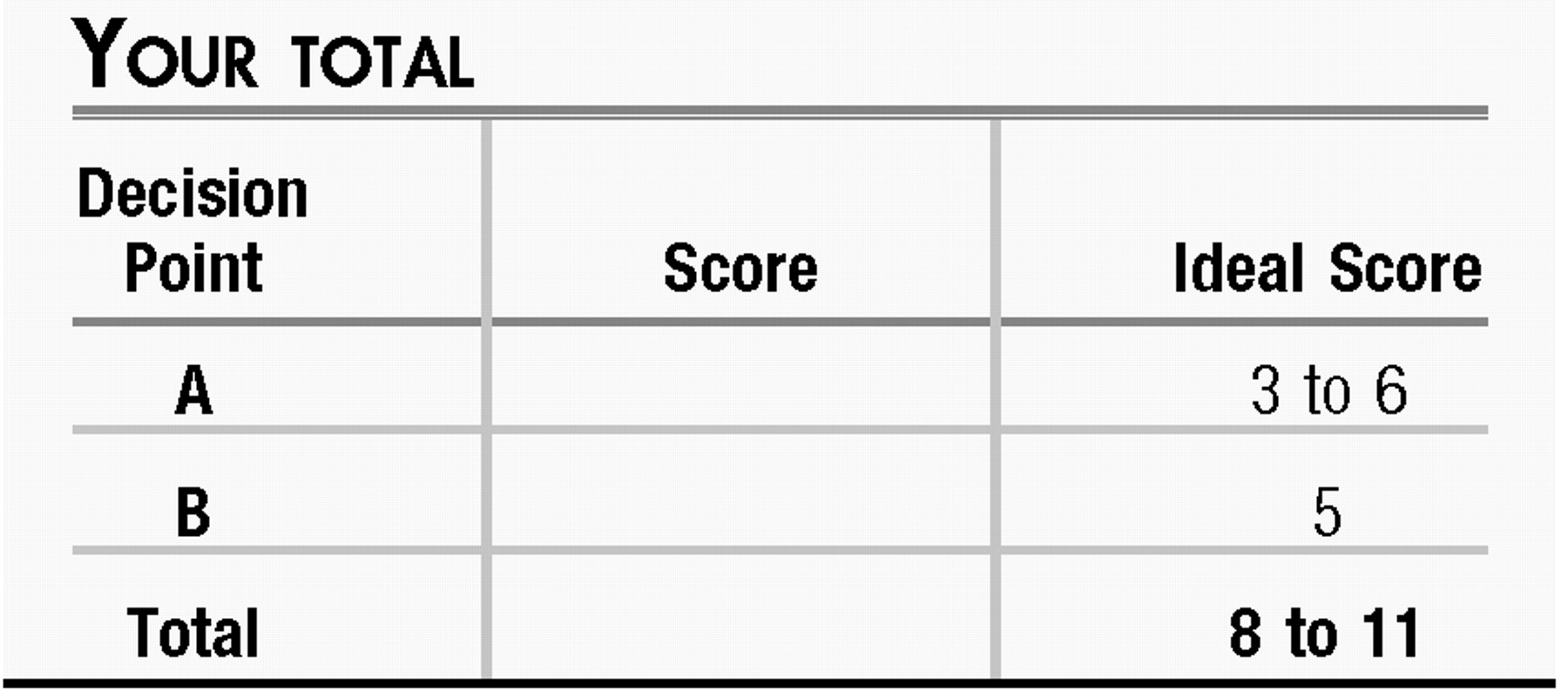
ANSWERS: SCORING, RELATIVE WEIGHTS, AND COMMENTS
Consideration Point A:
| A1._____ | −1 Alcohol withdrawal. A 20-something man who has been out celebrating with friends may fit an actuarial profile of being at risk for misusing alcohol, and withdrawal symptoms emerging after a few days of “enforced abstinence” are a common occurrence when patients are taking nothing by mouth. This patient's history is of only two beers on the night of the motor vehicle accident, and blood alcohol level data were consistent with that being the truth, going against this possibility. If liver function test results were elevated, the possibility of longer-standing alcoholism might be important to consider, but with normal results, this item can be de-prioritized. |
| A2._____ | +2 Narcotic analgesic side effects. Reactions of lability, disinhibition, and irritability may be idiosyncratically associated with the CNS effects of narcotic analgesics, along with the more classic effects of mental slowing or sedation. Assessing any temporal pattern relating times of doses with times of behavioral issues could help clarify the relevance of these agents to the patient's behavioral and emotional symptoms. |
| A3._____ | −2 Urinary tract infection. Although urinary tract infections are a common reason for delirium in older adults, they are not frequent in generally healthy men in this age group, and seldom are associated with CNS effects in the absence of urinary system findings of frequency, urgency, pain, and cloudy urine. Urine dip was performed on admission along with a urine toxicology screen, and both showed negative findings. |
| A4._____ | +1 Fat embolus. Fat emboli from fractures of long bones fortunately are not common but do have the potential to be lethal; confusion can be a presenting symptom. Jim's confusion was reported to be transient rather than persistent or progressive. If vital signs and pulse oximetry results are unremarkable, then the likelihood of this phenomenon is lower. |
| A5._____ | +3 Mood disorder. Inpatient teams may raise the question of depression in a patient who presents as lacking the motivation to enthusiastically embrace their directions, whether for vigorous incentive spirometry or postoperative physical rehabilitation. However, other features of this patient's situation—being tearful and withdrawn, showing irritability, and wishing to be left alone—could also point to the possibility of a preexisting mood disturbance as well as adjustment disorder or acute stress disorder. Alas, a full and truthful response may not be forthcoming when the question “are you depressed?” is asked by an imposing figure towering over a patient in bed, especially when posed at 5:30 a.m. during rounds with an entourage of staff crowding around the bed; tactful assessment during a private interview is more likely to be revealing. |
Consideration Point B:
| B1._____ | +3 Resume paroxetine. By history, the patient has achieved remission with paroxetine at 30 mg/day and would still be taking it had he not been admitted after the motor vehicle accident. Resuming an SSRI is a common strategy for relieving discontinuation syndrome and tends to be effective with modest rapidity. Given that he has missed doses for several days, a conservative approach would be to restart this agent at 20 mg/day with a plan to increase the dose to his prior dose of 30 mg/day in a week. |
| B2._____ | +2 Address symptoms with lorazepam. Benzodiazepines can ease some of the symptoms of discontinuation syndrome (1), and the use of low-dose lorazepam can be justified as an intervention for restlessness and agitation while waiting for resumption of his antidepressant to remedy the underlying pathophysiology of the discontinuation syndrome. (This can also be a useful tactic when it is not possible for a patient to resume antidepressant treatment promptly, e.g., because of continued nothing by mouth status.) |
| B3._____ | −1 Fluoxetine. Some have suggested that the pharmacokinetic properties of fluoxetine can be advantageously used to manage antidepressant discontinuation syndrome (2, 3), particularly when one is tapering a medication that is being discontinued. Because the goal you and the patient share is for him to resume taking a therapeutic dose of the agent that had led to his remission, rather than stopping antidepressant treatment or transitioning to something else, this is not a preferred strategy in this situation. |
| B4._____ | −3 Haloperidol. Neuroleptic agents have a long history of off-label use in helping to manage the agitation and confusion associated with delirium. The patient's mental status examination showed fairly good cognitive function, so the possible benefits do not clearly outweigh the potential risks. |
REFERENCES
Information & Authors
Information
Published In
History
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).