Over the past 40 years, more than 60 prospective studies have examined the link between established indices of depression and prognosis in individuals with known coronary heart disease (CHD) (
1). Since the first major review articles were published in the late 1990s (
2–
5), there have been more than 100 additional narrative reviews of this literature, as well as numerous meta-analyses examining the role of depression on cardiovascular morbidity and mortality (
6–
11). Despite differences in samples, duration of follow-up, and assessment of depression and depressive symptoms, these studies have demonstrated relatively consistent results.
Depression is ≈3 times more common in patients after an acute myocardial infarction (AMI) than in the general community (
12). Assessments conducted in the hospital indicate that 15% to 20% of patients with myocardial infarction (MI) meet
Diagnostic and Statistical Manual of Mental Disorders (
13) criteria for major depression (duration since admission, no assessment of functional impairment), and an even greater proportion show an elevated level of depressive symptoms (
14–
16). Prevalence rates of depression have been shown to be higher among women in the general population (
17) and among cardiac patients (
18), with recent evidence suggesting that young women may be at particularly high risk for depression after AMI (
19). Prevalence estimates in patients hospitalized for unstable angina, angioplasty, bypass surgery, and valve surgery are similar to those in patients with AMI, with slightly higher levels reported in patients with congestive heart failure (
1–
9). Less is known about the prevalence of depression in outpatient samples; however, available studies suggest that both major depression and elevated depressive symptoms are also considerably higher among people with CHD living in the community as compared with individuals without CHD (
9–
12). A recent study based on National Health Interview Survey data of 30,801 adults found the 12-month prevalence of major depression to be 9.3% in individuals with cardiac disease as compared with 4.8% in those with no comorbid medical illness (
20). Depression prevalence ranged from 7.9% to 17% in those with other chronic medical conditions. The study found that the coexistence of major depression with chronic conditions is associated with more ambulatory care visits, emergency department visits, days spent in bed because of illness, and functional disability.
Major depression and elevated depressive symptoms are associated with worse prognosis in patients with CHD (
10,
21–
25). In fact, most studies that have examined the relationship between increasing depression severity and cardiac events have shown a dose-response relationship, with more severe depression associated with earlier and more severe cardiac events (
10,
22). Not all individual studies have shown a significant link between depression and prognosis after statistical adjustment for measures of cardiac disease severity. Although some argue that this association is entirely explained by cardiac disease severity, most studies show robust links that remain statistically significant after adjustment for other potential confounders (
8,
15,
22,
26–
28). Methodological differences, including sample sizes, sample characteristics, selection of covariates, definition of outcomes, and length of follow-up, may account for the variations across studies (
1,
6–
8,
29,
30). There is general consensus that depression remains associated with at least a doubling in risk of cardiac events over 1 to 2 years after an MI (
1,
6,
7,
9,
21).
Both biological and behavioral mechanisms have been proposed to explain the link between depression and CHD. In comparison with nondepressed individuals, depressed patients with CHD frequently have higher levels of biomarkers found to predict cardiac events or promote atherosclerosis. Although not always consistent, several studies in depressed patients with coronary artery disease have reported reduced heart rate variability (suggesting increased sympathetic activity and/or reduced vagal activity) (
31), evidence of hypothalamic-pituitary-adrenal axis dysfunction (
32), increased plasma platelet factor 4 and β-thromboglobulin (suggesting enhanced platelet activation) (
33,
34), impaired vascular function (
35), and increased C-reactive protein, interleukin-6, intercellular adhesion molecule-1, and fibrinogen levels (suggesting increased innate inflammatory response) (
36,
37). Depression can be highly correlated with other mental disorders (eg, anxiety disorders) that have also been associated with adverse cardiac outcomes (
38,
39). Certain behaviors and social characteristics in depressed patients may also contribute to the development and progression of coronary disease. These include diet, exercise, medication adherence, and tobacco use, as well as social isolation and chronic life stress (
21,
40–
44). Although the specific behavioral and biological processes remain unclear, the alteration of these processes is associated with depressive symptoms, consistently in a direction that increases cardiovascular risk.
Beyond what many believe to be its pathophysiological effect on the heart, depression is associated with decreased adherence to medications (
21,
40,
45,
46) and triple the risk of noncompliance with medical treatment regimens (
47). Depression reduces the chances of successful modifications of other cardiac risk factors (
48) and participation in cardiac rehabilitation (
49,
50) and is associated with higher healthcare utilization and costs (
9,
51,
52) and, not surprisingly, greatly reduced quality of life (
24,
53,
54). Thus whether depression affects cardiac outcomes directly or indirectly, the need to screen and treat-depression is imperative (
55).
ASSESSMENT OF DEPRESSION AND DEPRESSIVE SYMPTOMS
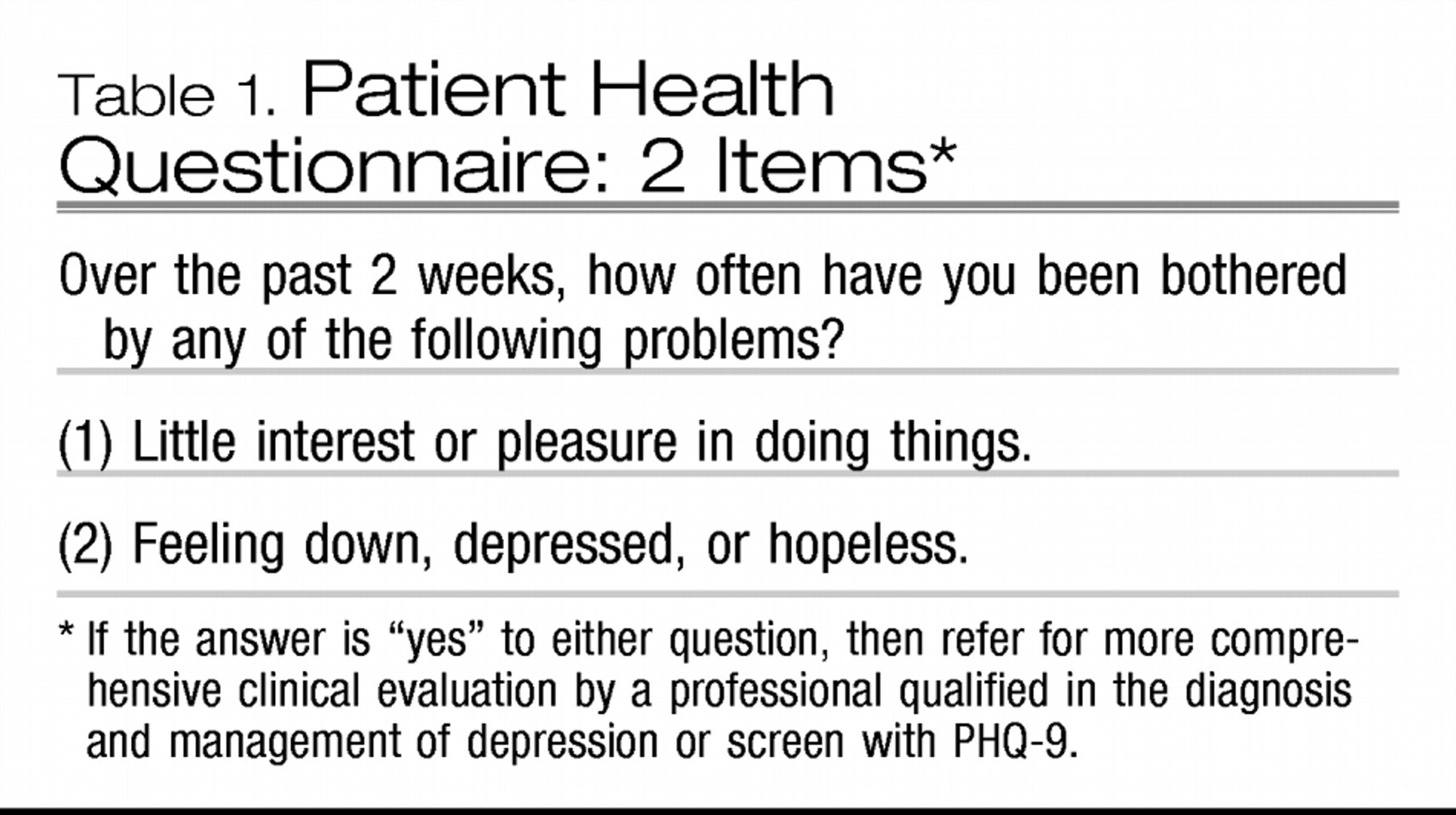
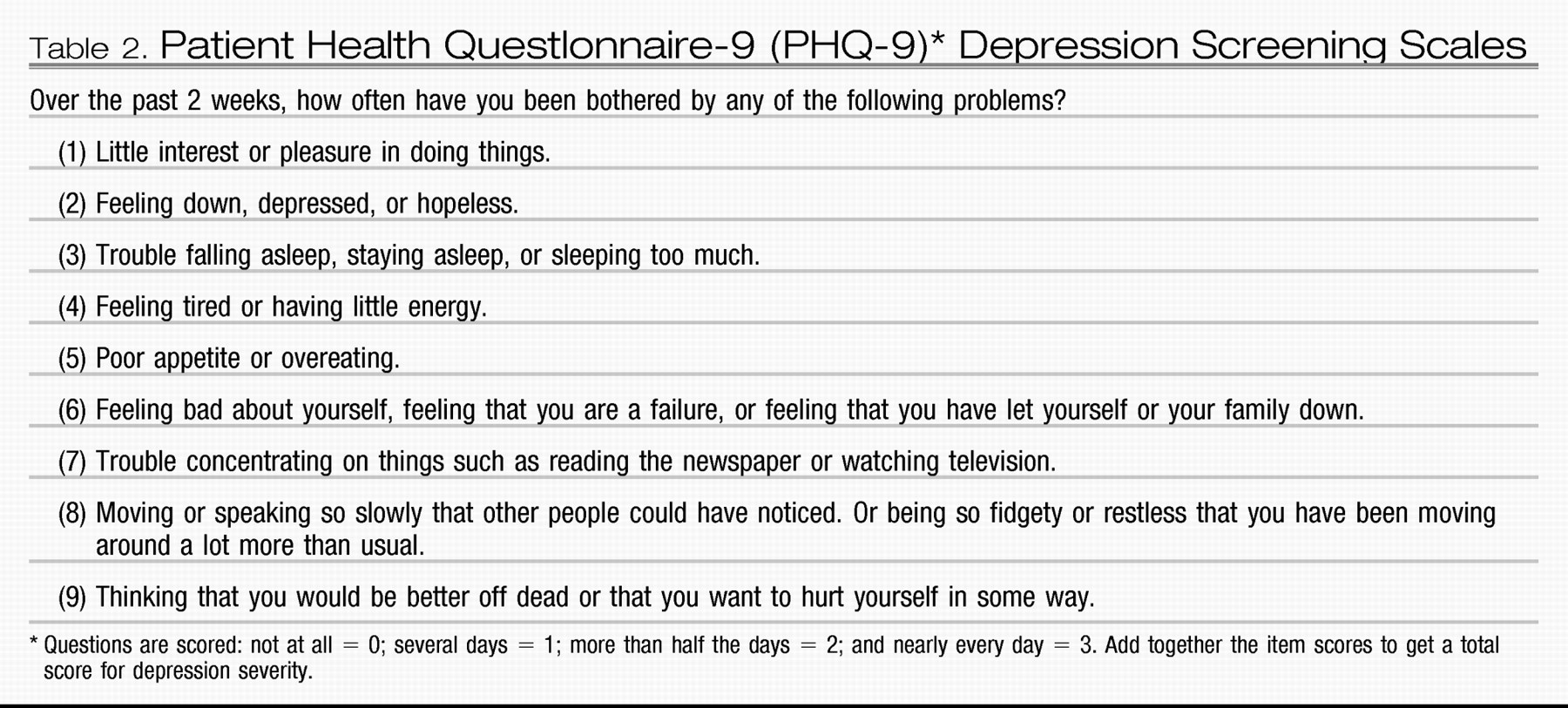
At a minimum, the Patient Health Questionnaire (PHQ-2) (
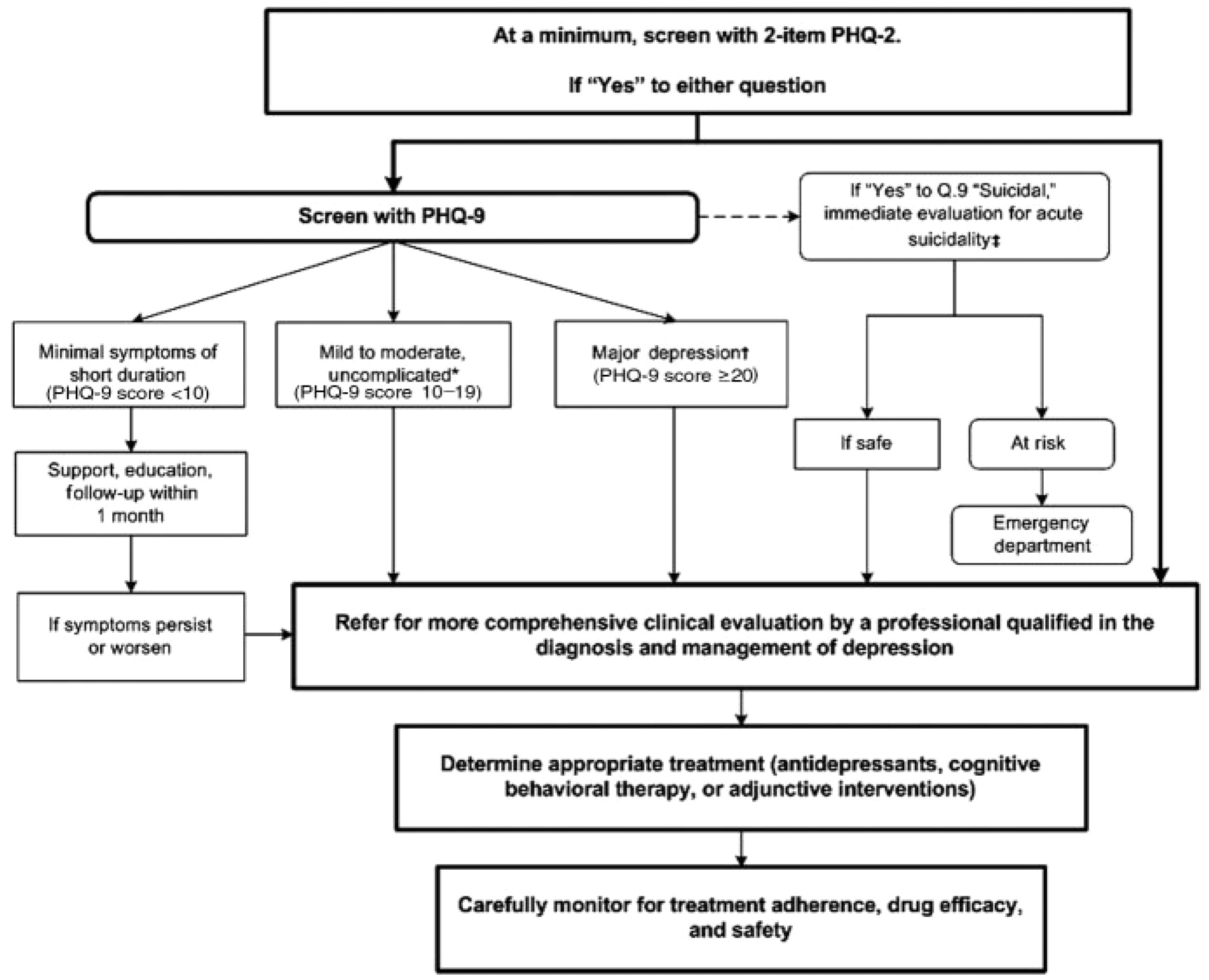
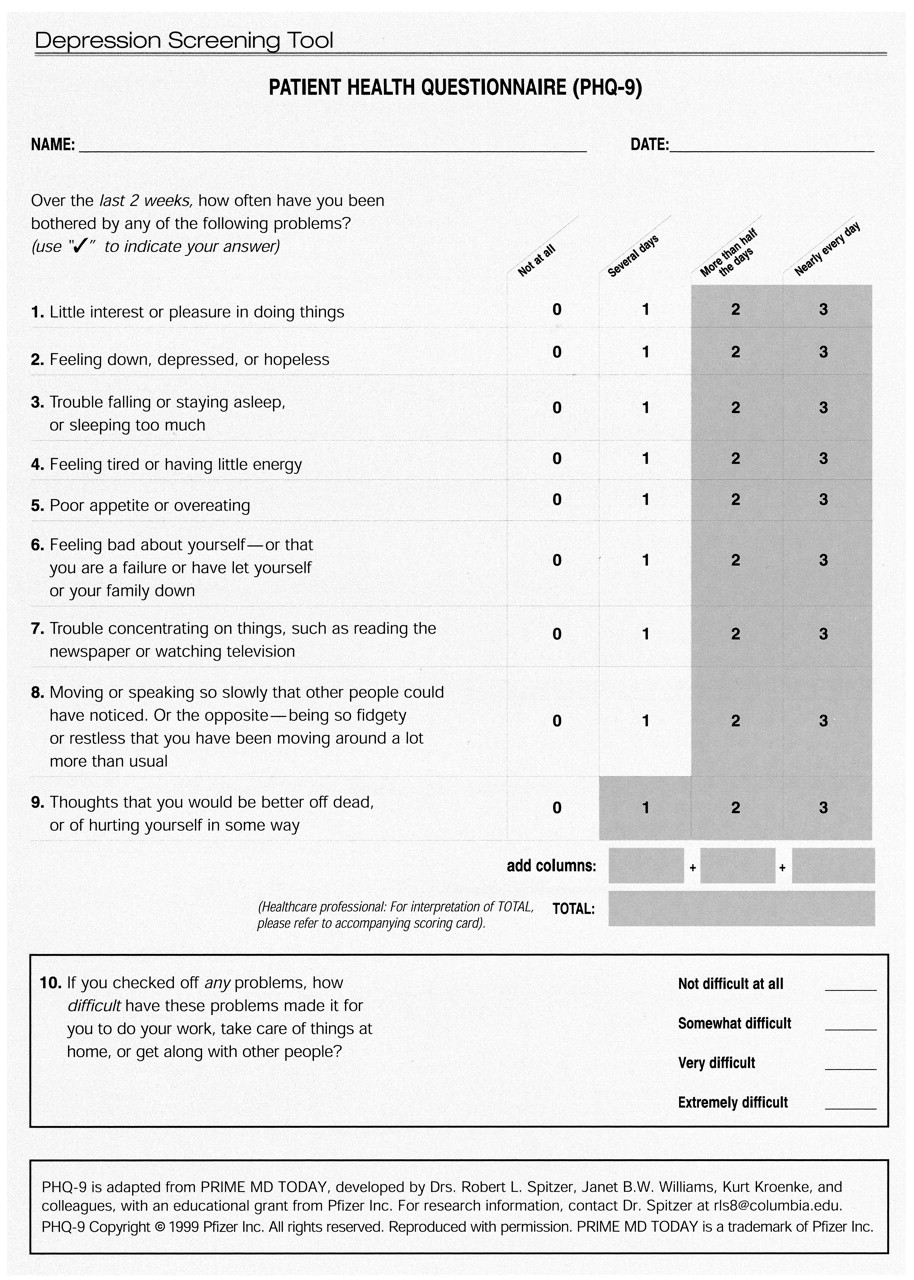
56) provides 2 questions that are recommended for identifying currently depressed patients (
Table 1). If the answer is “yes” to either or both questions, it is recommended that all 9 PHQ items (PHQ-9;
Table 2) be asked (
57). The PHQ-9 is a brief depression screening instrument (Appendix) (
66). Most patients are able to complete it without assistance in 5 minutes or less. It yields both a provisional depression diagnosis and a severity score that can be used for treatment selection and monitoring. The PHQ-9 has been shown to have reasonable sensitivity and specificity for patients with CHD (
58–
60). For patients with mild symptoms, follow-up during a subsequent visit is advised. In patients with high depression scores, a physician or nurse should review the answers with the patient. Other assessment tools and their use for research purposes have been discussed elsewhere (
61). Any of these tools can provide a useful initial assessment, but it must be recognized that depressive symptoms may present within the context of a complex medical condition. This current science advisory builds on the approach developed by the MacArthur Initiative on Depression and Primary Care (
62–
64), which provides empirically supported tools and procedures for the recognition and treatment of depression in primary care settings for depression screening and care guidelines for cardiologists (
65–
66). However, patients with screening scores that indicate a high probability of depression (PHQ-9 score of 10 or higher) should be referred for a more comprehensive clinical evaluation by a professional qualified to evaluate and determine a suitable individualized treatment plan (
Figure). Patients who meet the threshold for a more comprehensive clinical evaluation should be evaluated for the presence of other mental disorders (eg, anxiety) that have also been shown to be associated with adverse outcomes in cardiac patients (
38–
39).
Cardiologists should take depression into account in the management of CHD, regardless of whether they treat the depression or refer the patient to a healthcare provider who is qualified in the assessment and treatment of depression, which often may be the patient's primary care provider (
65). Current evidence indicates that only approximately half of cardiovascular physicians report that they treat depression in their patients, and not all patients who are recognized as depressed are teated (
67). Some physicians are reluctant to treat depression in patients with CHD because they believe that depression after an acute cardiac event is a “normal” reaction to a stressful life event that will remit when the acute event stabilizes and the individual resumes customary activities. However, in many cases, depression may occur before and continue after an acute cardiac event (
68). Although there is currently no direct evidence that screening for depression leads to improved outcomes in cardiovascular populations, depression has been linked with increased morbidity and mortality, poorer risk-factor modification, lower rates of cardiac rehabilitation, and reduced quality of life. Therefore, it is important to assess depression in cardiac patients with the goal of targeting those most in need of treatment and support services.
DEPRESSION TREATMENT
Treatment options include antidepressant drugs, cognitive behavioral therapy, and physical activity such as aerobic exercise and cardiac rehabilitation.
Antidepressant drugs
Although antidepressant use has been associated with both increased and decreased cardiac risk in some epidemiological studies (
69), randomized clinical trials have demonstrated that 2 selective serotonin reuptake inhibitor (SSRI) antidepressants, sertraline and citalopram, are safe for patients with CHD and effective for moderate, severe, or recurrent depression (
70,
71). Nonrandomizcd, post hoc analysis of the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) study revealed that patients treated with an SSRI, whether assigned to receive cognitive behavioral therapy or usual care, had a 42% reduction in death or recurrent MI as compared with the depressed patients not receiving an antidepressant (
72). Given that SSRI treatment soon after AMI appears safe, is relatively inexpensive, and may be effective for post-AMI depression, it seems appropriate to screen and treat depression. Not only does treatment improve mood and quality of life, but studies have shown that depression interferes with compliance, and treatment of depressive symptoms may improve medication adherence in patients after AMI (
73).
Sertraline and citalopram are the first-line antidepressant drugs for patients with CHD. Patients with recurrent depression who previously tolerated and responded well to another antidepressant may resume taking that agent instead, unless it is now contraindicated. For example, tricyclic antidepressants and monoamine oxidase inhibitors are contraindicated for many patients with heart disease because of their cardiotoxic side effects (
74). If pharmacological treatment is initiated, patients should be observed closely for the first 2 months and regularly thereafter to monitor suicidal risk, ensure medication compliance, and detect and manage adverse effects. Approximately 15% to 25% of patients stop their antidepressants during the first 6 months of treatment because of adverse effects or lack of efficacy (
14–
75). Therefore, potential drug interactions or adverse effects should be closely monitored.
COGNITIVE BEHAVIORAL THERAPY
Cognitive behavioral therapy can benefit depression in cardiac patients (
76). It may be an alternative for cardiac patients who cannot tolerate antidepressants or who may prefer a nonpharmacological or counseling approach to treatment. Also, many patients with moderate to severe depression may respond better to the combination of an antidepressant and psychotherapy than to either treatment alone. Referral to a qualified psychotherapist is necessary. In ENRICHD, a randomized controlled trial, at least 12 to 16 sessions of cognitive behavioral therapy over 12 weeks were advocated to achieve remission of moderate to severe depression (
77,
78). In clinical practice, the duration and frequency can be customized by the treating therapist to meet the individual needs of the patient; some patients may prefer and do well with a less intensive regimen.
PHYSICAL ACTIVITY/EXERCISE
Aerobic exercise (
79) and cardiac rehabilitation
80) can reduce depressive symptoms in addition to improving cardiovascular fitness. Although depression may be a barrier to participation in cardiac rehabilitation and exercise programs, cardiologists can help depressed patients overcome this barrier by providing encouragement and follow-up contacts. They should also enlist the help of spouses, partners, or family to improve adherence. The prescription of exercise would need to be individually assessed based on cardiac status and exercise capacity of the individual (
81).
The depression guidelines for the primary care population have documented that treatment with appropriate pharmacological agents versus behavioral interventions are similarly effective; the combination of both has the benefit of lower relapse rates (
63,
64). There is no evidence that treatments for depression are differentially effective in cardiac versus other patients. There is as yet no direct evidence showing that treatment of depression improves cardiac outcomes; patients may remain at increased risk for major cardiac events and mortality even when treated for depression (
72). Evidence suggests that depressed patients who are not responsive to treatment for depression may be at greater risk for adverse cardiac events (
82). Aggressive cardiologic care may help mitigate this increased risk. Depressed patients may also require additional clinical management to ensure compliance with cardiac treatment regimens and to promote lifestyle behavior change.
SUMMARY
In summary, the high prevalence of depression in patients with CHD supports a strategy of increased awareness and screening for depression in patients with CHD. Specifically, we recommend the following:
•.
Routine screening for depression in patients with CHD in various settings, including the hospital, physician's office, clinic, and cardiac rehabilitation center. The opportunity to screen for and treat depression in cardiac patients should not be missed, as effective depression treatment may improve health outcomes.
•.
Patients with positive screening results should be evaluated by a professional qualified in the diagnosis and management of depression.
•.
Patients with cardiac disease who are under treatment for depression should be carefully monitored for adherence to their medical care, drug efficacy, and safety with respect to their cardiovascular as well as mental health. Monitoring mental health may include, but is not limited to, the assessment of patients receiving antidepressants for possible worsening of depression or suicidality, especially during initial treatment when doses may be adjusted, changed, or discontinued. Monitoring cardiovascular health may include, but is not limited to, more frequent office visits, ECGs, or assessment of blood levels of medications on the basis of the individual needs and circumstances of the patient.
•.
Coordination of care between healthcare providers is essential in patients with combined medical and mental health diagnoses.
For Writing Group Disclosures refer to original article.
ACKNOWLEDGMENTS
The authors thank Drs. Kenneth E. Freedland and Robert M. Carney for their valuable contributions to the manuscript.