Alcohol, tobacco, and other substance use disorders are among the most common medical problems in patients presenting in primary care and specialty mental health settings. In the United States, it is estimated that one in seven adults will have an alcohol or other substance use disorder over the course of his or her lifetime (
1). Alcohol and nicotine disorders are most prevalent. Nearly one-third of U.S. adults drink enough to cause or place them at risk of adverse consequences (
2), whereas 28% of the population aged 12 or older use tobacco products and 9% have used illicit drugs in the past month (
3). Individuals with substance use disorders have very high rates of morbidity, mortality, and functional impairment, as well as significantly higher medical costs associated with their disproportionate use of health care resources (
4–
8). Alcohol and tobacco use are two of the nation's leading causes of death from modifiable factors (
8,
9). Moreover, substance use disorders are common comorbidities among individuals with mood, anxiety, and other mental disorders (
5). Longitudinal studies suggest that individuals with these diagnoses are at an increased risk for the later onset of nicotine, alcohol, and illicit drug dependence (
10).
Despite the availability of effective treatments and preventative interventions (
11–
18), only a minority of patients receive care of any type, and there is generally a 10-year gap between the onset of these disorders and first treatment, according to studies of treatment access in the United States (
8,
19–
21). Systematic assessments of the quality of general medical and specialty mental health care in the United States indicate that patients with substance use problems and disorders receive the poorest overall quality of care compared with that for individuals with other conditions (
22). A major national study of care quality in primary care practices found that only 11% of patients with alcohol dependence received what the study described as indicators of quality care, including assessment of alcohol dependence among binge drinkers and treatment referral for individuals with a diagnosis of alcohol dependence (
22).
Among psychiatric patients treated in routine practice settings in the United States, approximately one-quarter were identified by their treating psychiatrist as having a current substance use disorder (
23); however, the majority of these patients were not reported to be receiving current treatment for these conditions. For example, 91% of patients identified as having nicotine dependence were not receiving any smoking cessation treatments (
24). Similarly, nearly 7 of 10 patients with identified alcohol dependence and 6 of 10 patients with other identified substance use disorders were not receiving treatment for these disorders from their psychiatrist or any other clinician. Although medications to treat other mental health conditions are commonly used by psychiatrists, medications to treat substance use disorders are rarely used in routine psychiatric practice settings (
25). These findings underscore the fact that clinical assessment and treatment of substance use and related disorders represents a tremendous opportunity to improve clinical practice in an area of medicine associated with high morbidity and mortality (
4–
8).
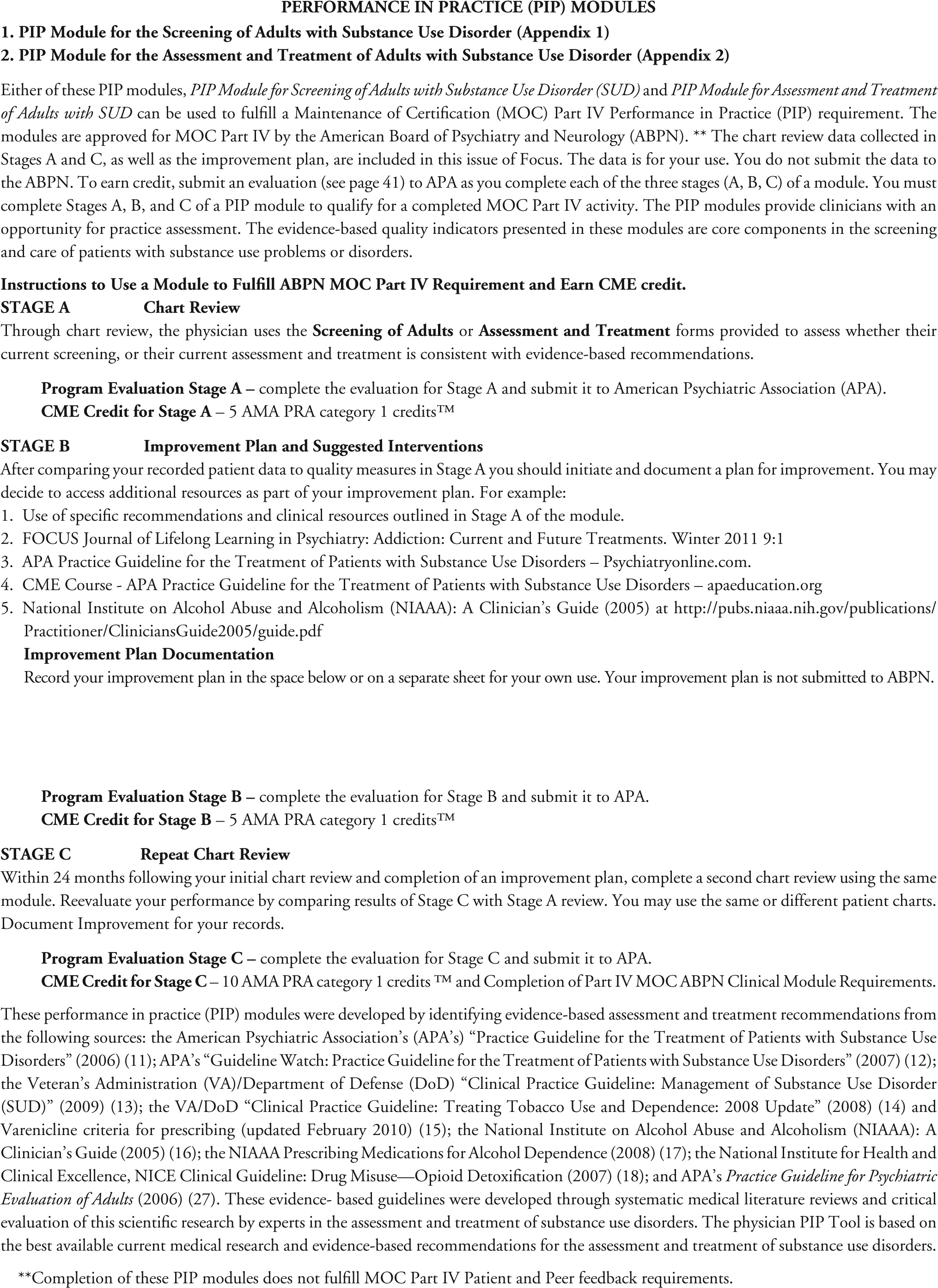
The American Board of Medical Specialties (ABMS) and the American Board of Psychiatry and Neurology (ABPN) are now moving to implement multifaceted
Maintenance of Certification (MOC) requirements to enhance quality of patient care and assess and verify the competence of physicians over time (
26). Beginning in 2013, for those applying for 2014 MOC examinations, a practice assessment component of maintenance of certification will require physicians to compare their care for five or more patients with “… published best practices, practice guidelines or peer-based standards of care and develop a plan to improve effectiveness and efficiency of his or her clinical activities” (
26). Because the assessment and treatment of substance use disorders reflects a clinical area of great opportunity to improve clinical practices and ameliorate the immense burden of disease and suffering associated with these conditions, these
Performance in Practice: Physician Practice Assessment Tools for the Screening, Assessment, and Treatment of Adults with Substance Use Disorder were developed to meet the new ABMS and ABPN MOC requirements.
These performance in practice (PIP) tools were developed by first identifying evidence-based assessment and treatment recommendations from the following sources: the American Psychiatric Association's (APA's) “Practice Guideline for the Treatment of Patients with Substance Use Disorders” (2006) (
11); APA's “Guideline Watch: Practice Guideline for the Treatment of Patients with Substance Use Disorders” (2007) (
12); the Veteran's Administration (VA)/Department of Defense (DoD) “Clinical Practice Guideline: Management of Substance Use Disorder (SUD)” (2009) (
13); U.S. Department of Health and Human Services “Clinical Practice Guideline: Treating Tobacco Use and Dependence: 2008 Update” (2008) (
14) and Varenicline criteria for prescribing (updated February 2010) (
15); the National Institute on Alcohol Abuse and Alcoholism (NIAAA): A Clinician's Guide (2005) (
16); the NIAAA Prescribing Medications for Alcohol Dependence (2008) (
17); the National Institute for Health and Clinical Excellence, NICE Clinical Guideline: Drug Misuse—Opioid Detoxification (2007) (
18); and APA's
Practice Guideline for Psychiatric Evaluation of Adults (2006) (
27). These evidence-based guidelines were developed through systematic medical literature reviews and critical evaluation of the scientific research by experts in the assessment and treatment of substance use disorders. Consequently, the physician PIP Tools presented here are based on the best available current medical research and evidence-based recommendations for the assessment and treatment of substance use disorders.
These
Performance in Practice: Physician Practice Assessment Tools for the Screening, Assessment, and Treatment of Adults with Substance Use Disorder are specifically intended to do the following:
1.
Provide simple assessment tools for physicians to examine the care provided to systematically selected adult patients to assess whether the clinician's current patient assessment and treatment practices for alcohol, tobacco, opiate and other substance use disorders are consistent with the latest evidence-based recommendations.
2.
Offer valuable clinical resources (including easily accessible sources for brief screening, assessment, and treatment interventions) and key evidence-based recommendations for clinicians to use if they identify areas in which additional knowledge or modifications to clinical practices may help improve clinical assessment and treatment practices.
3.
Provide a brief, practical, easy-to-use tool that in the future may be used to meet the new ABMS and ABPN maintenance of certification requirements for assessments of clinical practice with the aim of enhancing the quality of patient care.
The
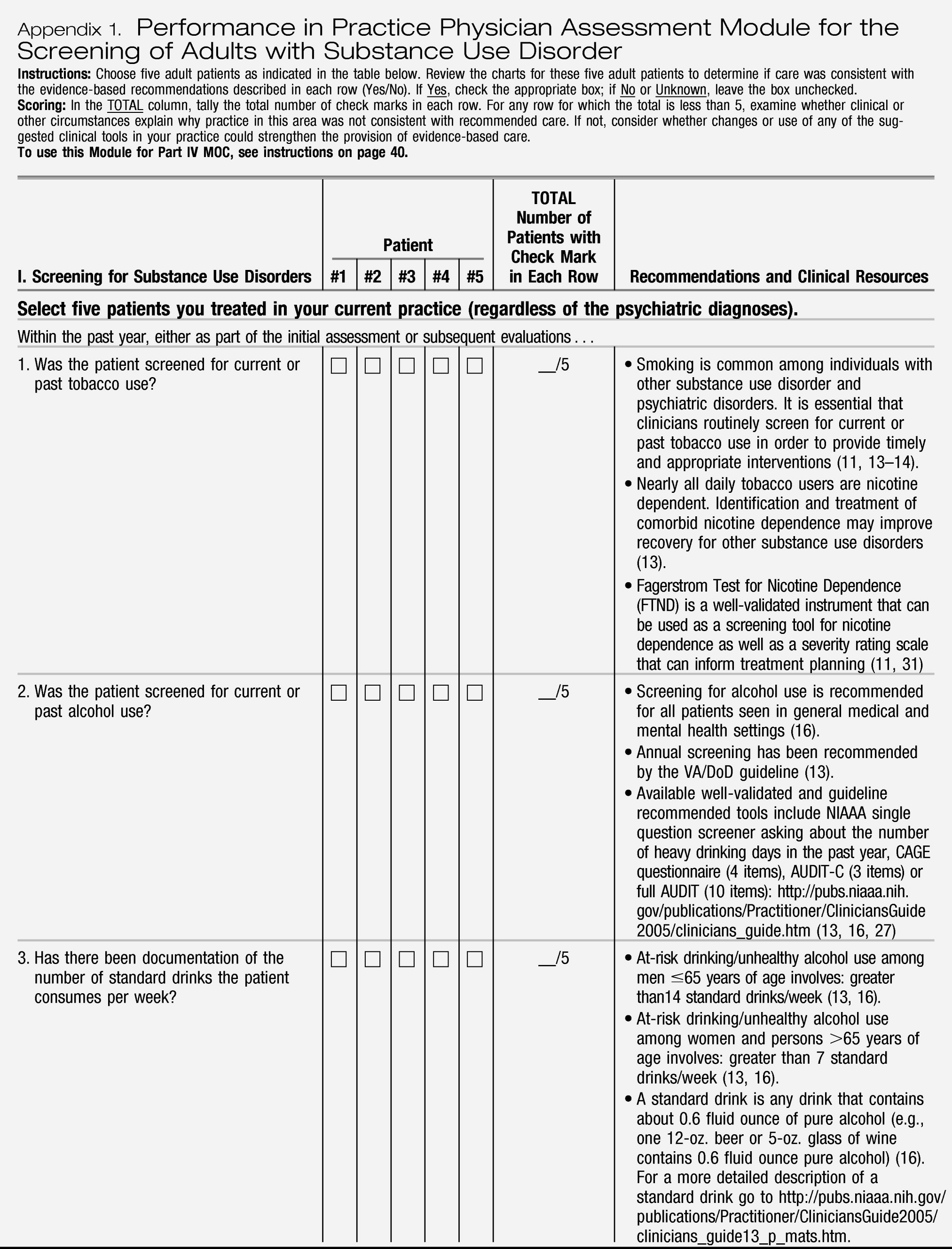
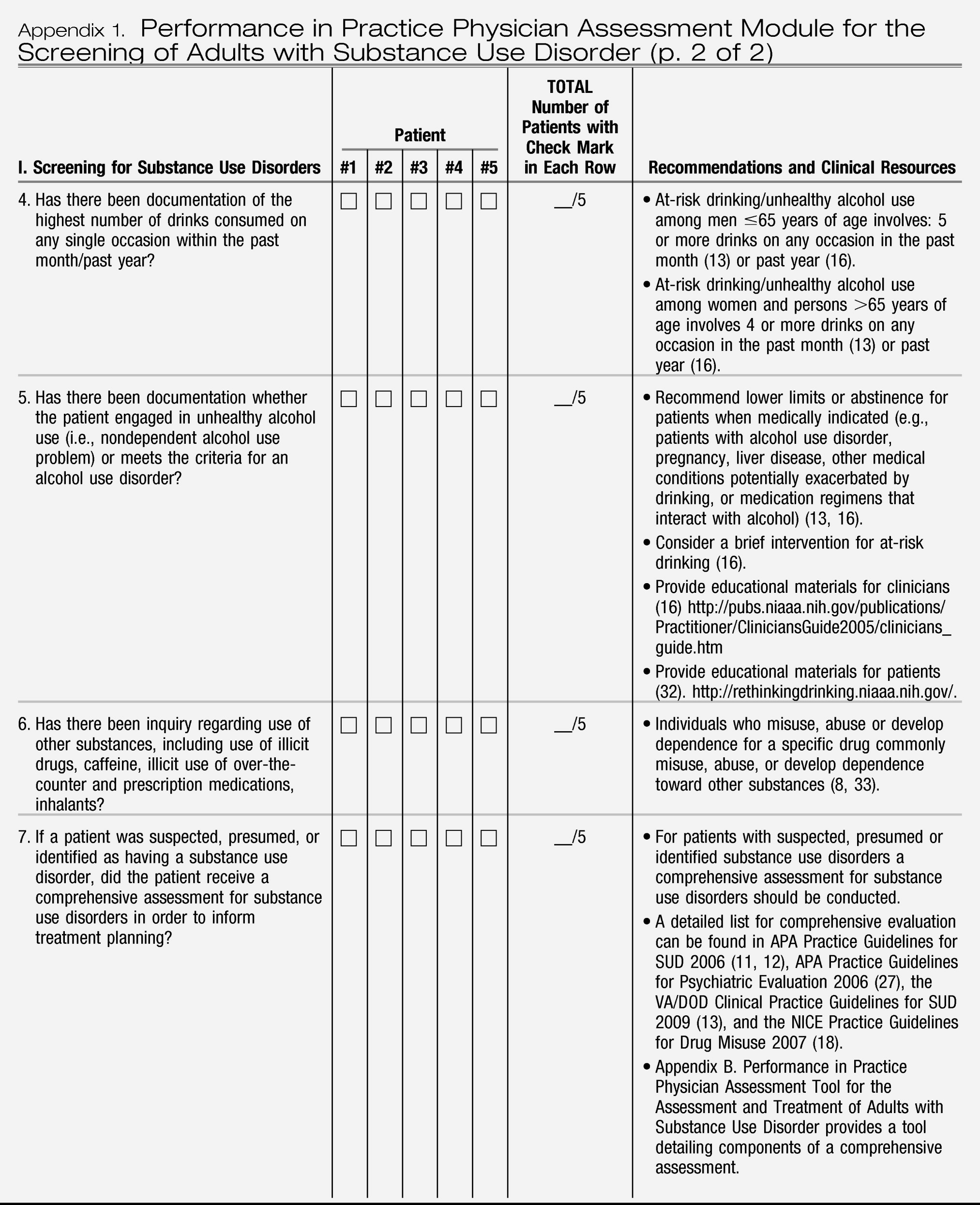
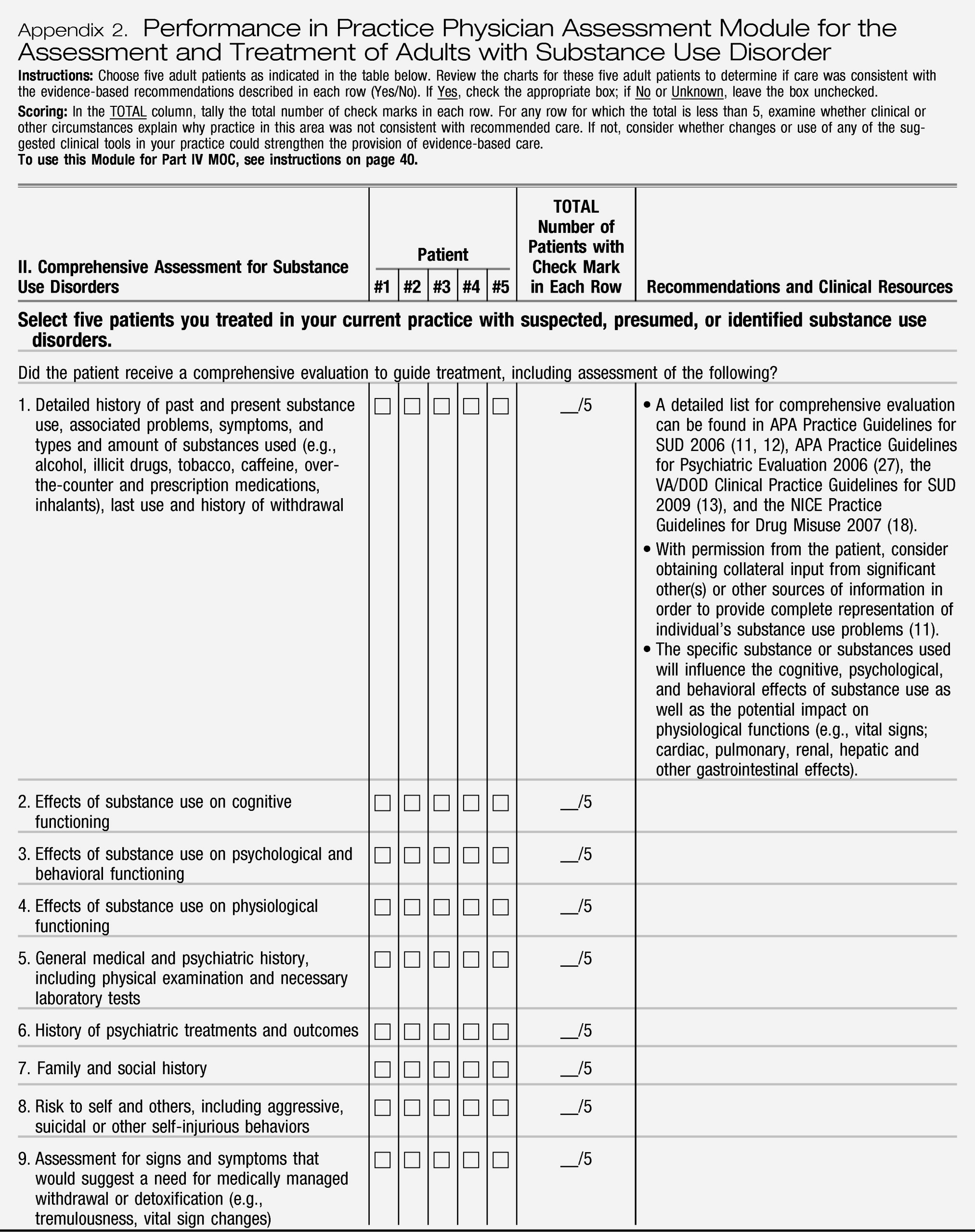
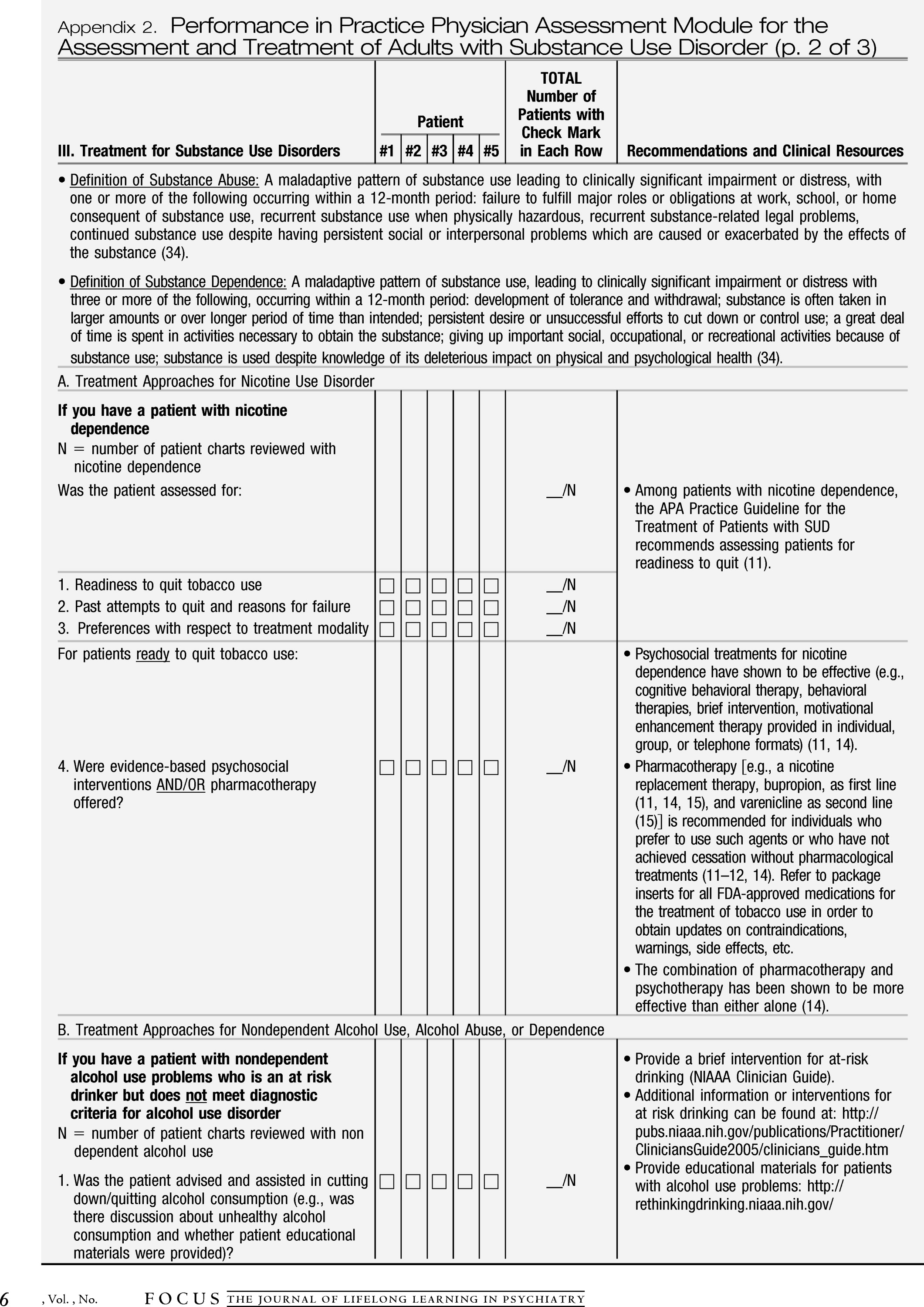
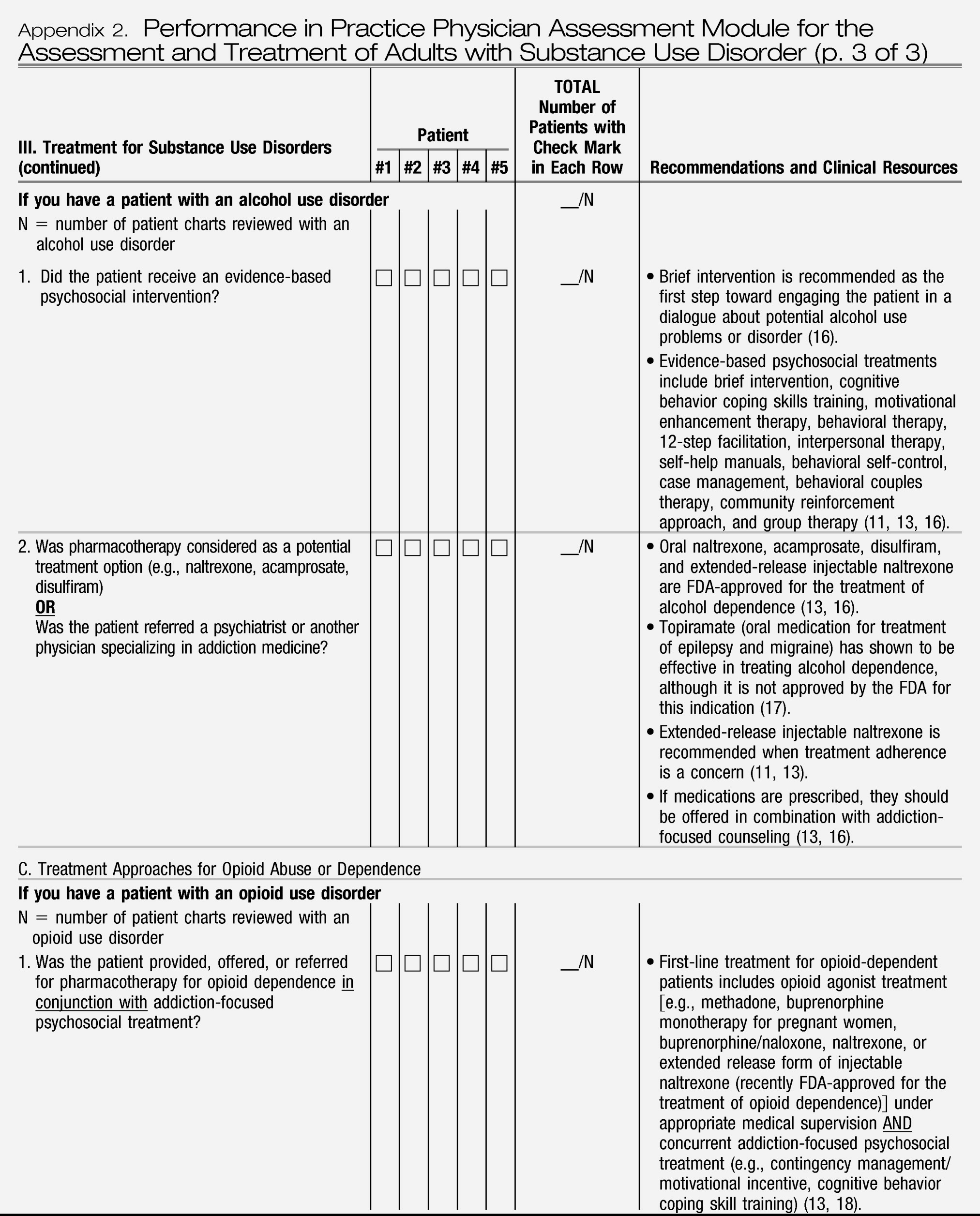
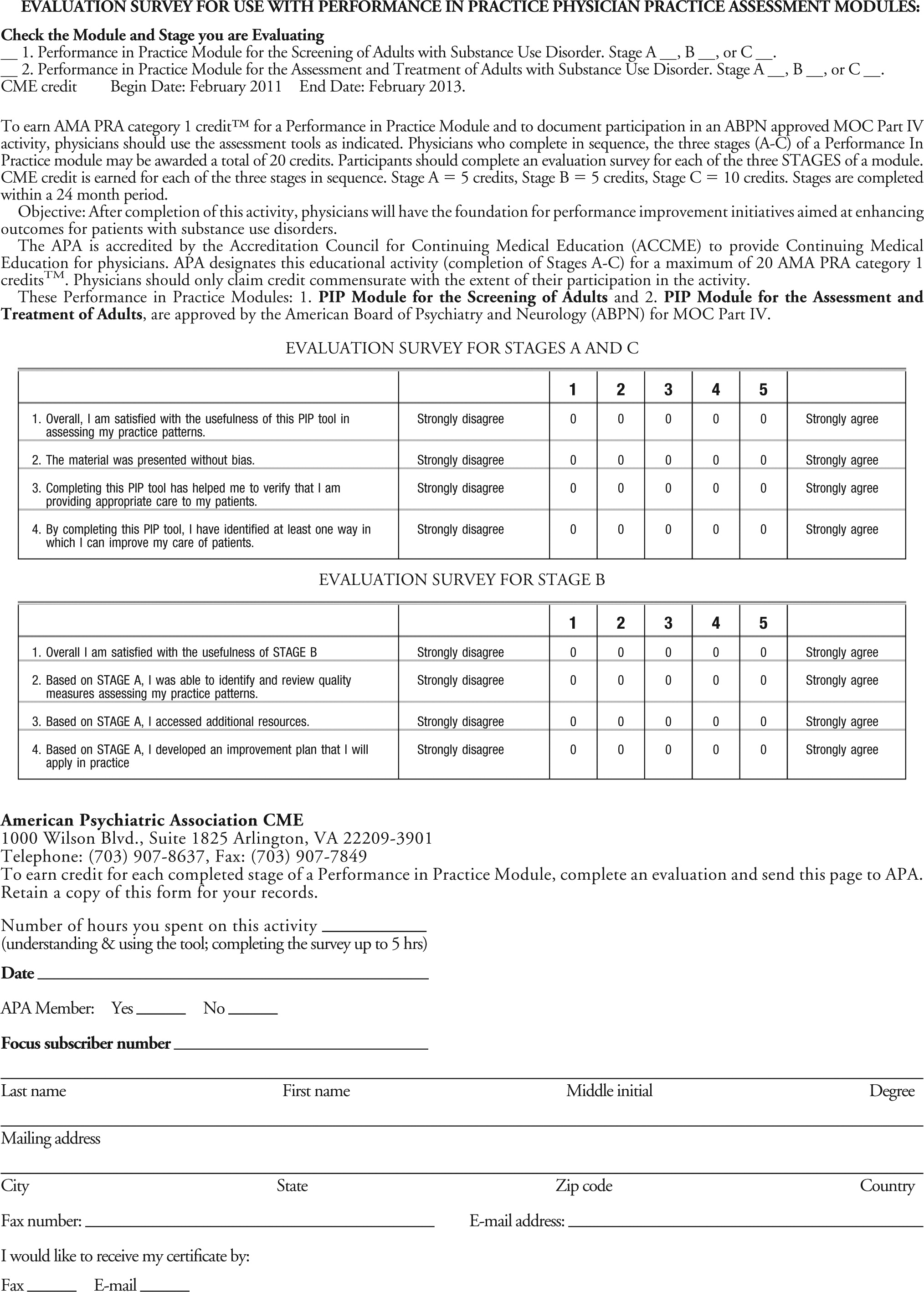
Performance in Practice: Physician Practice Assessment Tools for the Screening, Assessment, and Treatment of Adults with Substance Use Disorders presented in Appendices 1 and 2 are designed to facilitate retrospective chart review and allow physicians to evaluate their capacity to provide screening and comprehensive assessment and to allow physicians to evaluate their provision of evidence-based treatments for patients with selected substance use disorders. To this end, the PIP tools include three sections related to 1) screening of all patients for use of tobacco, alcohol, and other substances. 2) review of the core components of a comprehensive clinical evaluation for those whose screening results are positive, and 3) provision of treatment for nicotine, alcohol, and opioid use disorders for clinicians who wish to assess their practice alongside current evidence-based treatment recommendations. Each of the sections attempts to highlight aspects of care that have significant public health implications or for which gaps in guideline adherence are common (e.g., screening all patients for use of tobacco, alcohol, and other substances). The last column of the tools provides guideline-supported recommendations and clinical resources to assist in practice improvement efforts. Quality improvement opportunities that arise from using the tools can generally be managed by individual psychiatrists and applied as a part of their routine practice, rather than by relying on other health care system resources.
The PIP clinical tools have been designed to be relevant across clinical settings (e.g., inpatient and outpatient), straightforward to complete, and usable in a pen-and-paper format to aid adoption. In addition to its value as a practice-assessment tool, this form could be also used for retrospective peer-review initiatives. Although the ABPN MOC program requires review of at least five patients as part of each PIP unit, it is important to note that larger samples will provide more accurate estimates of quality of care within a practice.
After using the PIP tool to assess the pattern of care provided to patients, the physician should determine whether specific aspects of care need to be improved. Through such practice assessment, the physician may determine that deviations from the quality indicators are clinically appropriate and justified or he or she may choose to acquire new knowledge and modify his or her practice to improve quality. For example, if patients in the physician's current psychiatric caseload are not screened for tobacco or alcohol use, then an area for improvement could involve implementation of systematic screening for alcohol and tobacco use, which are common among patients with any psychiatric disorders.
It is important to note that although these tools are intended to highlight current evidence-based assessment and treatment recommendations for patients with or at risk for developing substance use disorders, justifiable variations from recommended care are expected. Assessment and treatment recommendations provided in the practice guidelines are generally intended to be relevant to the majority of individuals (
28,
29). However, patients vary widely in their clinical presentations, presence of comorbid physical and psychiatric conditions, response to treatment, and other factors that may influence clinical decision making. In addition, practice guidelines and quality indicators are often derived from findings of efficacy and effectiveness trials in which stringent enrollment criteria are used; thus individuals in clinical trials often differ in important ways from those seen in routine clinical practice (
30). To this end, divergence from evidence-based recommendations can be anticipated. Finally, the PIP tools need to be updated regularly to keep pace with the growing scientific base for the assessment and treatment of substance use disorders.
The PIP tools presented in Appendices 1 and 2 provide clinicians with an opportunity for practice assessment in preparation for the new 2014 ABPN MOC program requirements. Because the evidence-based quality indicators presented here are considered core components in the care of patients with substance use problems or disorders, use of this tool can serve as a foundation in developing a systematic approach to practice improvement for the assessment and treatment of patients with substance use disorders.
Acknowledgments
This work was generously funded by a grant from the American Psychiatric Foundation. Authors would like to thank John A. Renner, Jr., MD, Chair, APA's Council on Addiction Psychiatry, for his review and thoughtful feedback on this manuscript.