Neurologic disorders are complicated frequently by psychiatric disturbances, especially psychosis, depression, anxiety, and agitation. The frequency with which psychosis occurs ranges from 10% to 50% in patients with Alzheimer's disease and 3% to 30% in patients with Parkinson's disease.
1 Likewise, the coexistence of depression has been extensively studied in such disorders as Alzheimer's dementia, stroke, and Parkinson's disease. However, the frequency of depression in these disorders varies widely. From 0% to 50% of patients with Alzheimer's disease, 20% to 50% of patients following a stroke, and more than 50% of patients with Parkinson's disease will develop a depression syndrome.
1 Anxiety and agitation are often vague and ill defined; consequently, it has been very difficult to determine the frequency of these conditions in populations with concurrent neurologic disease.
Psychosis, depression, and agitation have considerable impact on functional status, independence, and quality of life for both the affected individual and the caregiver. Nutritional status of the person can be affected by the presence of these disorders; withdrawal and inactivity may result in muscle wasting and weakness as well as increased risk of aspiration pneumonia and pulmonary emboli. The excess disability associated with neuropsychiatric illness affects the underlying neurologic condition, resulting in poorer outcomes and increased morbidity and mortality.
The development of neuropsychiatric problems adds to caregiver stress. These psychiatric symptoms are often more overwhelming and disabling for the caregiver than the original problems associated with neurologic impairment. In fact, one study of people with dementia found that the caregiver burden associated with psychiatric disturbances is a stronger predictor of nursing home placement than dementia severity.
2 Consequently, these problems add to the increasing cost of caring for neurologically compromised people.
Management of these conditions varies considerably. Few placebo-controlled trials have been conducted on the treatment of psychosis, depression, anxiety, and agitation in neurologically impaired individuals. This report reviews all available double-blind, placebo-controlled trials of pharmacological interventions for the management of psychosis, depression, anxiety, and agitation in people with underlying neurologic disorders in order to provide a basis for the development of meaningful research initiatives for treatment of psychiatric symptoms in neurologic patients.
METHODS
We conducted an extensive review of the existing literature on treatment studies published from January 1966 to March 1998. This review included articles published in English indexed in medline, Psychinfo, and embase/Excerpta Medica. The papers of interest were double-blind placebo-controlled pharmacologic treatment trials for psychosis, depression, anxiety, or agitation in patients with underlying neurologic diseases. The neurologic disorders included, but were not limited to, dementia (of any type), Parkinson's disease, stroke, epilepsy, multiple sclerosis, Huntington's disease, human immunodeficiency virus (HIV)–related central nervous system (CNS) disease, mental retardation, brain injury, and CNS disease.
Search strategies for each psychiatric condition were individually designed for optimal capture of references pertaining to the specific target condition of psychosis, depression, anxiety, or agitation. A uniform strategy of using the same terms was employed between searches to retrieve references pertaining to specific neurological diseases. Because of differences in computerized literature database indexing and search strategies, different techniques can elicit different reference retrieval patterns. Articles are not always uniformly indexed within a specific database, nor between different databases. Despite this limitation, we detected and reviewed between 300 and 1,500 citations for each of the four psychiatric conditions identified.
RESULTS
Psychosis
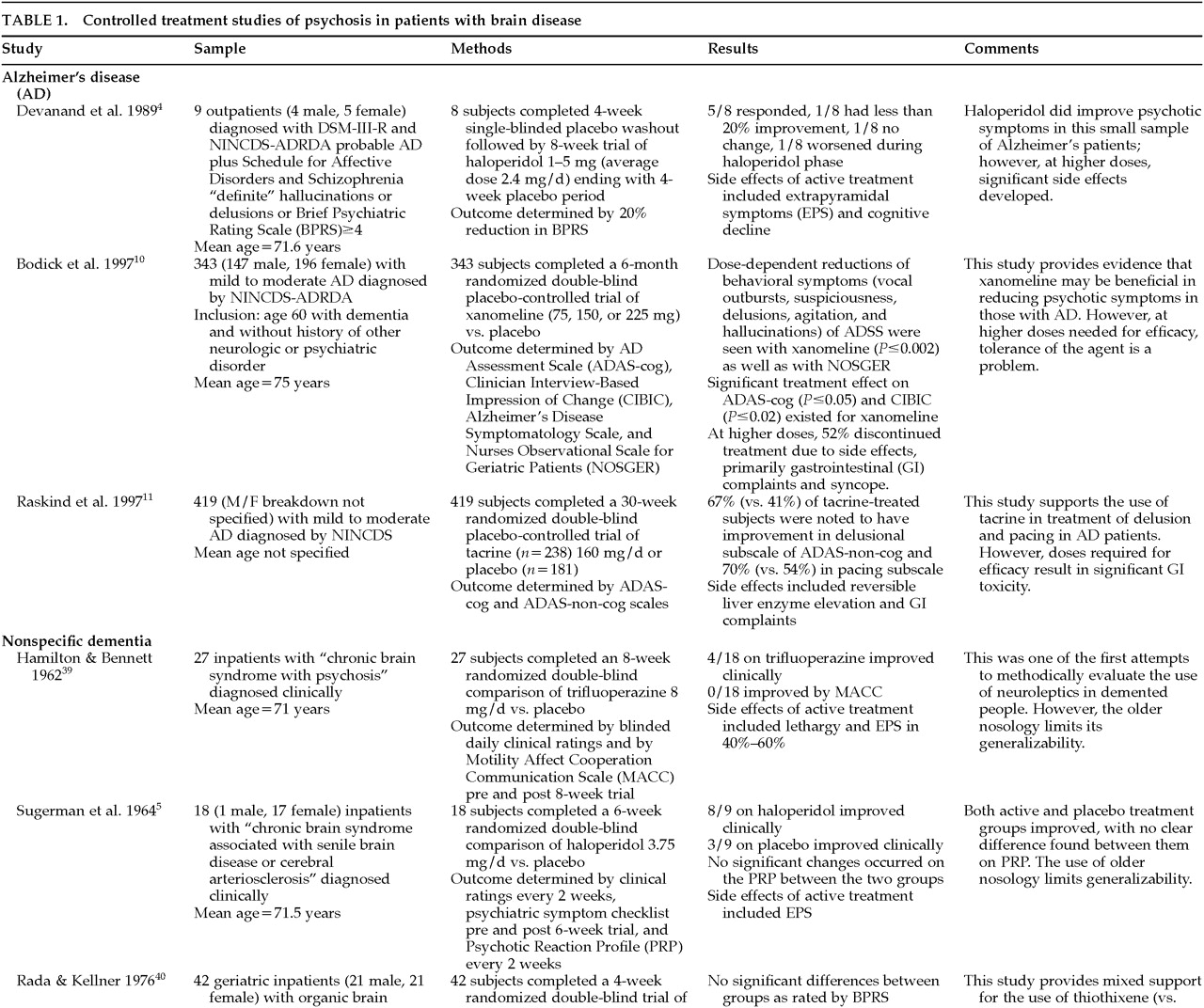
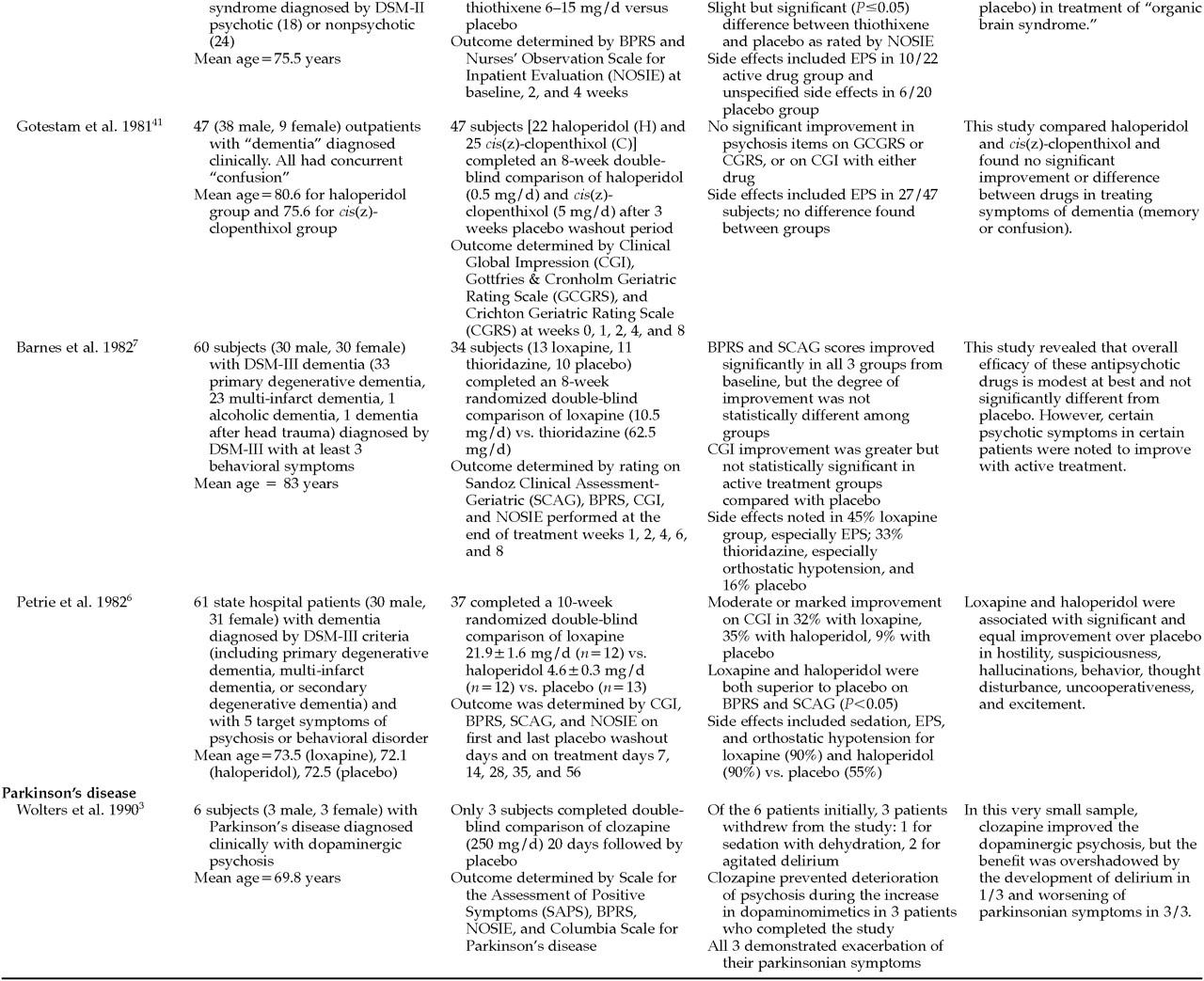
Ten studies examining the treatment of psychosis in patients with brain disease met the inclusion criteria for this study (
Table 1A and
Table 1B). Nine studies evaluated the use of pharmacologic agents in people with dementia. The remaining study
3 evaluated the use of clozapine in drug-induced psychosis in patients with Parkinson's disease being treated with dopamine agonists.
Neuroleptics including haloperidol
4–6 and thioridazine
7 have been shown to be superior to placebo in treating various psychotic symptoms in demented people. However, many of the older studies lack clear diagnostic criteria in determining their patient population. This limits the generalizability of the conclusions. Of trials reporting degrees of improvement, many reported only a modest advantage of active agent over placebo. Side effects were common, especially extrapyramidal symptoms, and were often more problematic than the original psychotic symptoms. Agitation, “noisiness,” “restiveness,” “overactivity,” and incontinence have worsened sometimes in subjects being treated with neuroleptics.
8 Consequently, the efficacy of neuroleptics in reducing psychotic symptoms does not always translate into improvements in patients' functional capacity.
9Although “atypical” neuroleptics are being treated as equal or superior to “traditional” neuroleptics with fewer side effects, only one placebo-controlled trial
3 was found. In this study, clozapine was used in patients with Parkinson's disease and psychosis. Half the subjects withdrew from the study because of significant side effects, and the other half exhibited a worsening of their parkinsonian symptoms.
Novel approaches to treating psychotic symptoms, making use of a knowledge of the pathophysiology of the underlying neurologic disorders, have been reported. Two recent studies
10,11 have studied muscarinic receptor agonists and cholinesterase inhibitors, respectively, in the treatment of psychiatric disturbances in patients with Alzheimer's disease. Unfortunately, the doses necessary to produce benefit also produced significant side effects, thereby limiting their clinical utility.
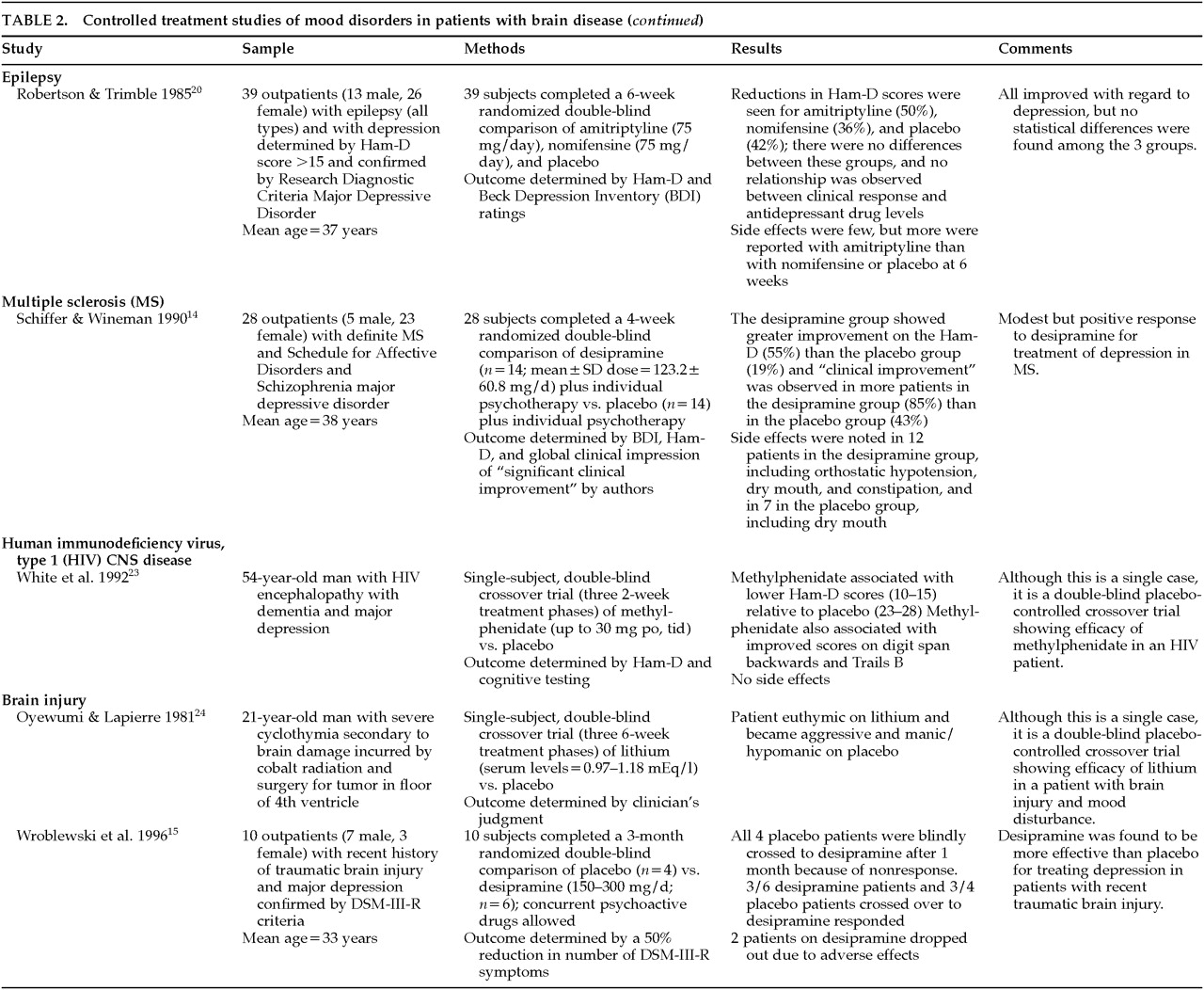
Depression
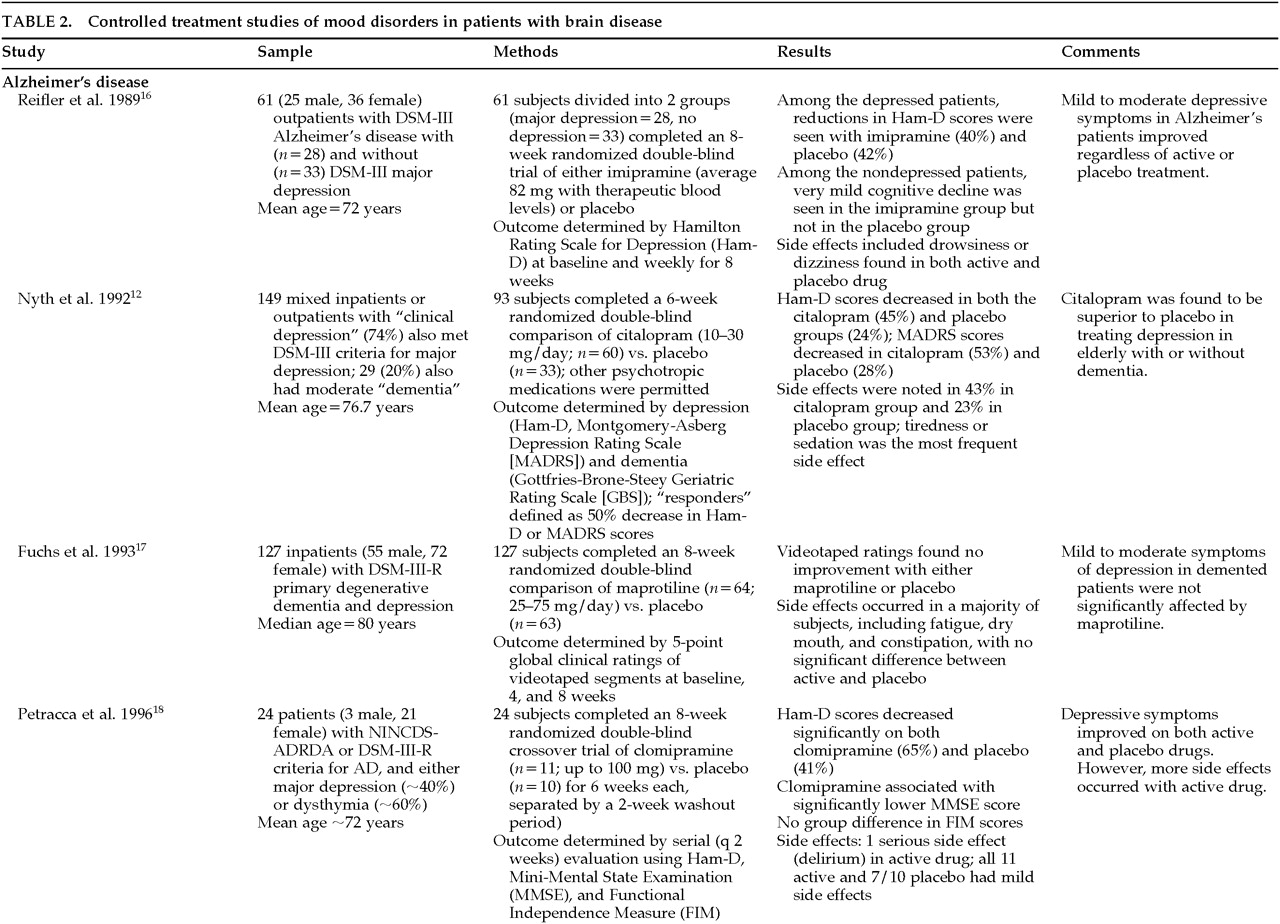
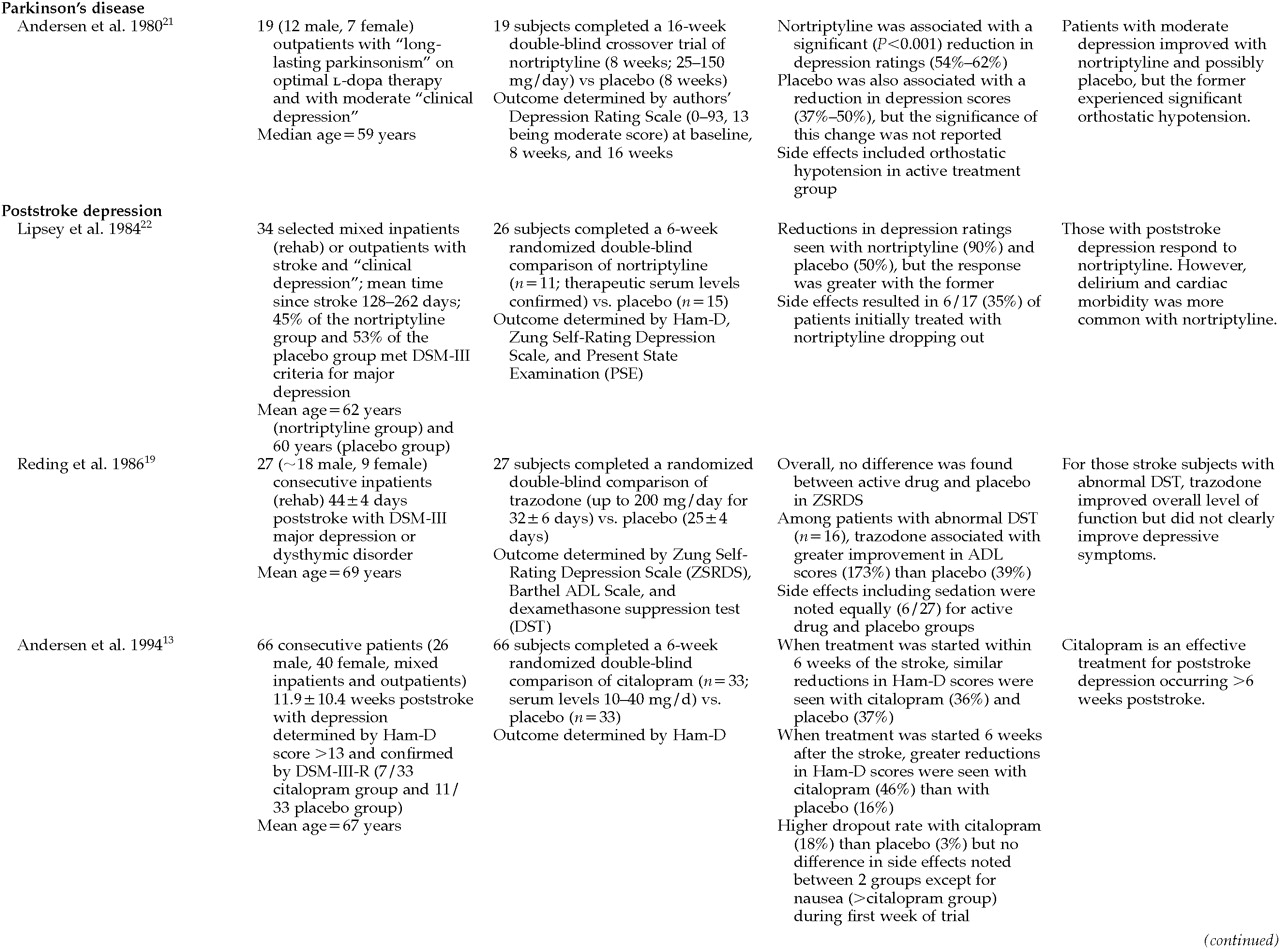
Thirteen studies were found on the treatment of mood disorders (depression) in individuals with brain diseases that met the inclusion criteria (
Table 2A,
Table 2B, and
Table 2C). Although depression is commonly found in patients with neurologic disorders, the treatment trial for any one group was very small, making it difficult to endorse any one approach to treating depression in these populations.
Only three studies with more than 10 subjects reported significant improvement in active drug over placebo in the treatment of depression in neurologically ill people. These included the use of citalopram in patients with depression and Alzheimer's disease
12 and with poststroke depression,
13 and use of desipramine in patients with depression and multiple sclerosis.
14 In a very small study of 10 patients, desipramine appeared to be superior to placebo in treating depression in brain-injured subjects; however, 2 of the subjects on active treatment dropped out.
15Nearly half of the trials reported that active treatment was no better than placebo. These studies examined the use of imipramine,
16 maprotiline,
17 or clomipramine
18 for depression in patients with Alzheimer's disease, trazodone
19 for patients with poststroke depression, and amitriptyline or nomifensine
20 in patients with depression and epilepsy. Beneficial effects of nortriptyline in patients with Parkinson's disease
21 were complicated by significant problems with orthostatic hypotension. Likewise, delirium and cardiovascular morbidity occurred in patients taking nortriptyline for poststroke depression.
22Two single-subject reports were found that used double-blind, placebo-controlled methodology. Methyl[chphenidate was found to be superior to placebo in treating depressive symptoms in a person with HIV disease,
23 and lithium was superior to placebo in treating depressive symptoms in subjects with “mood swings” following radiation and surgery for treatment of CNS tumor.
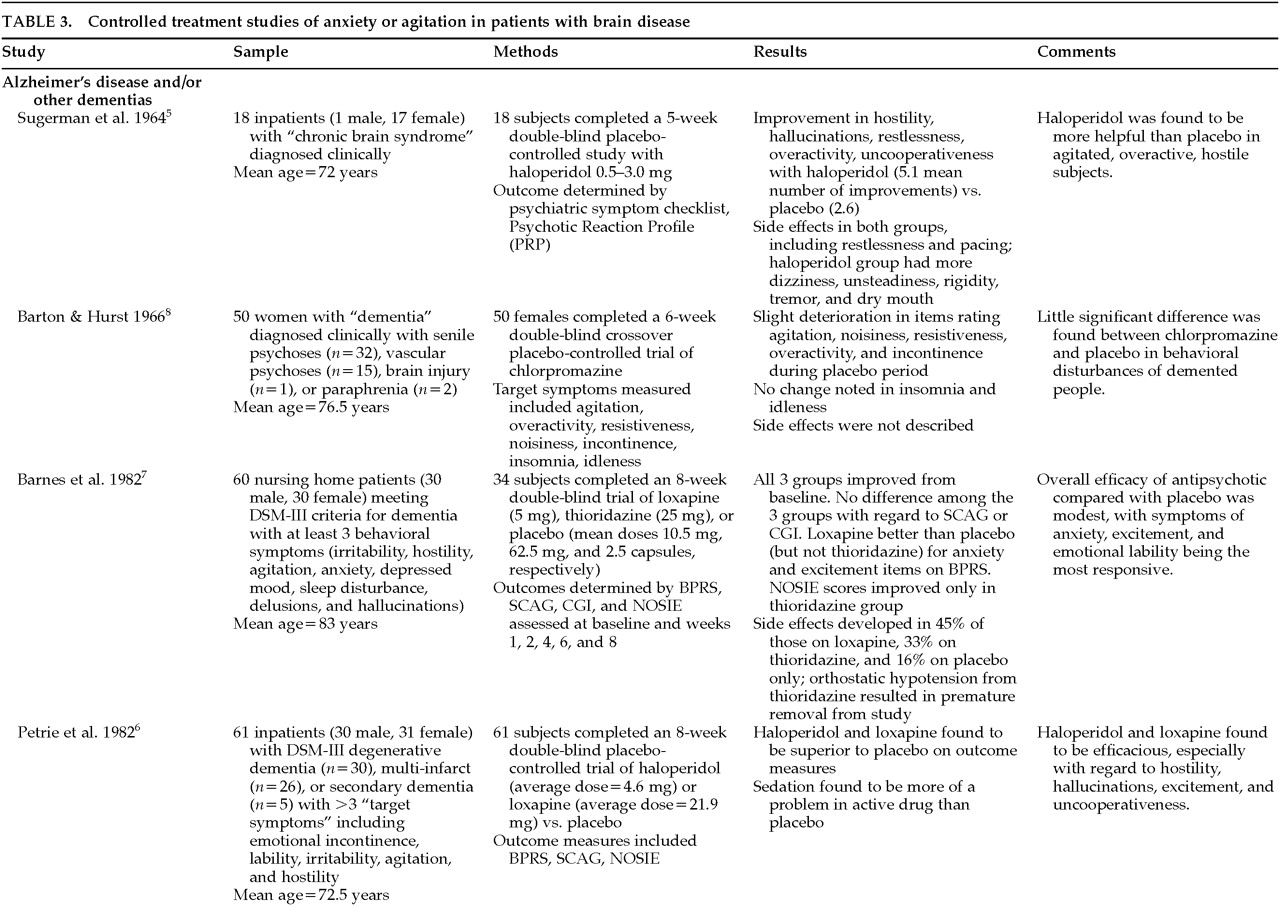
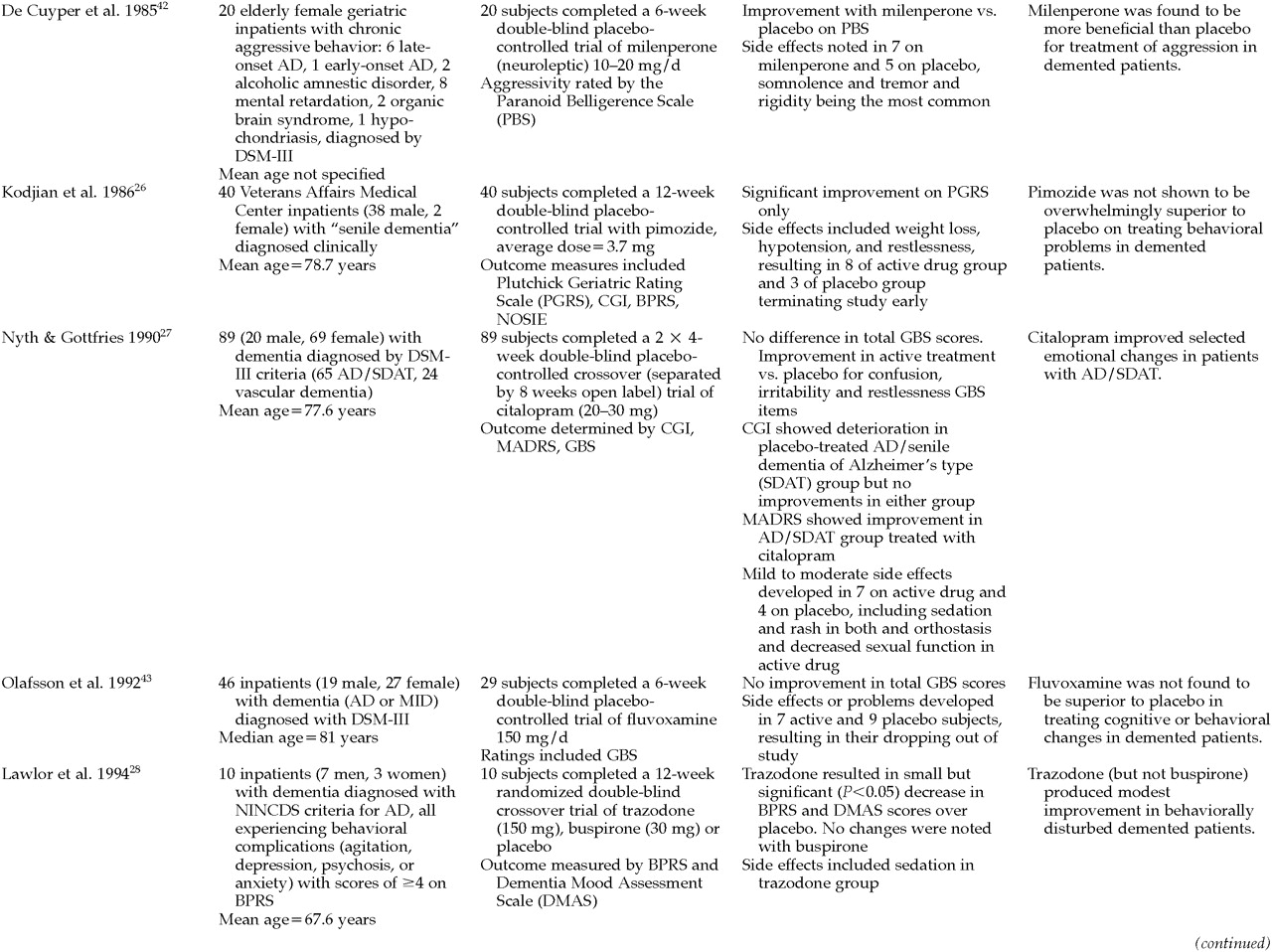
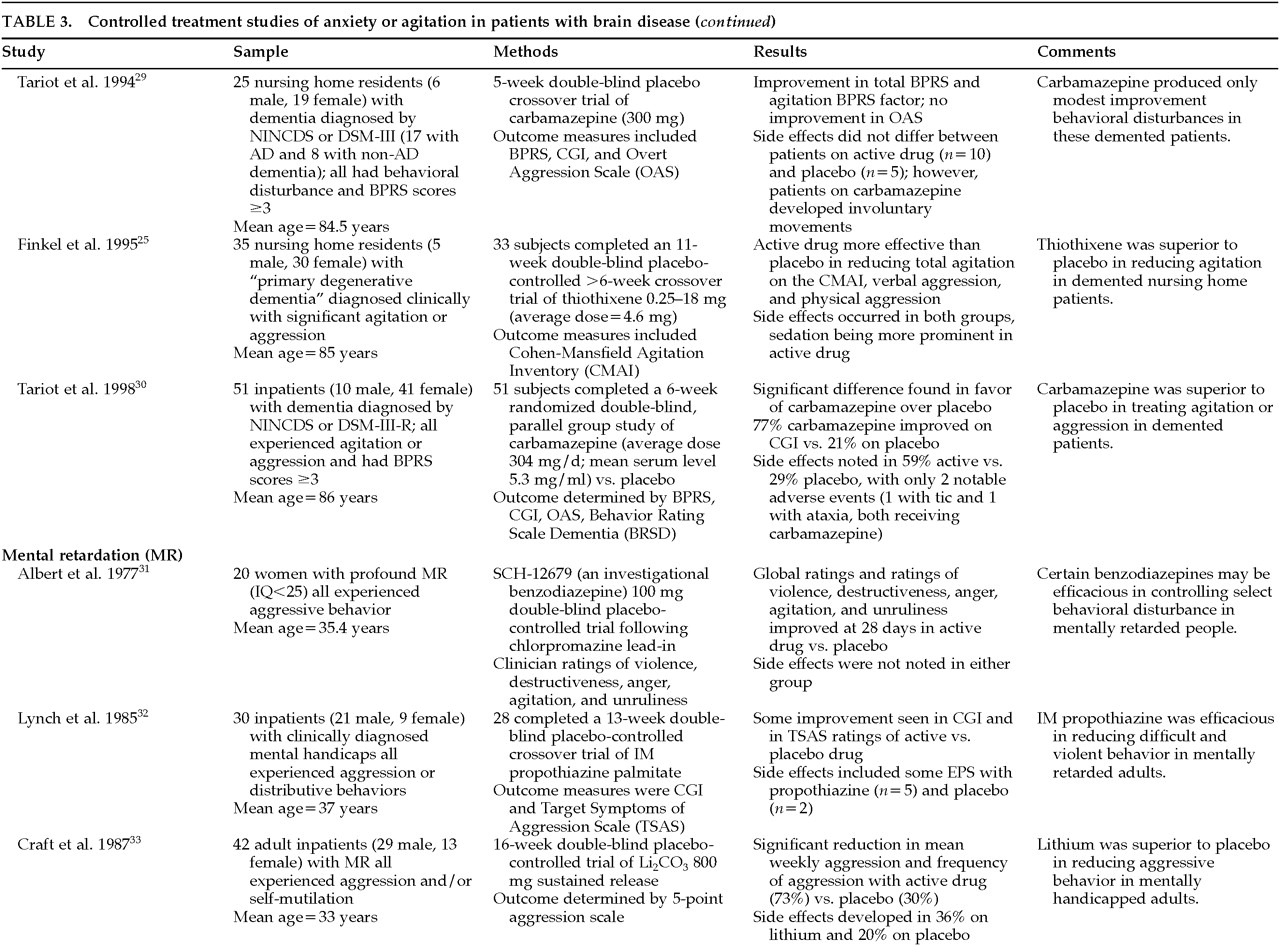
24Anxiety and Agitation
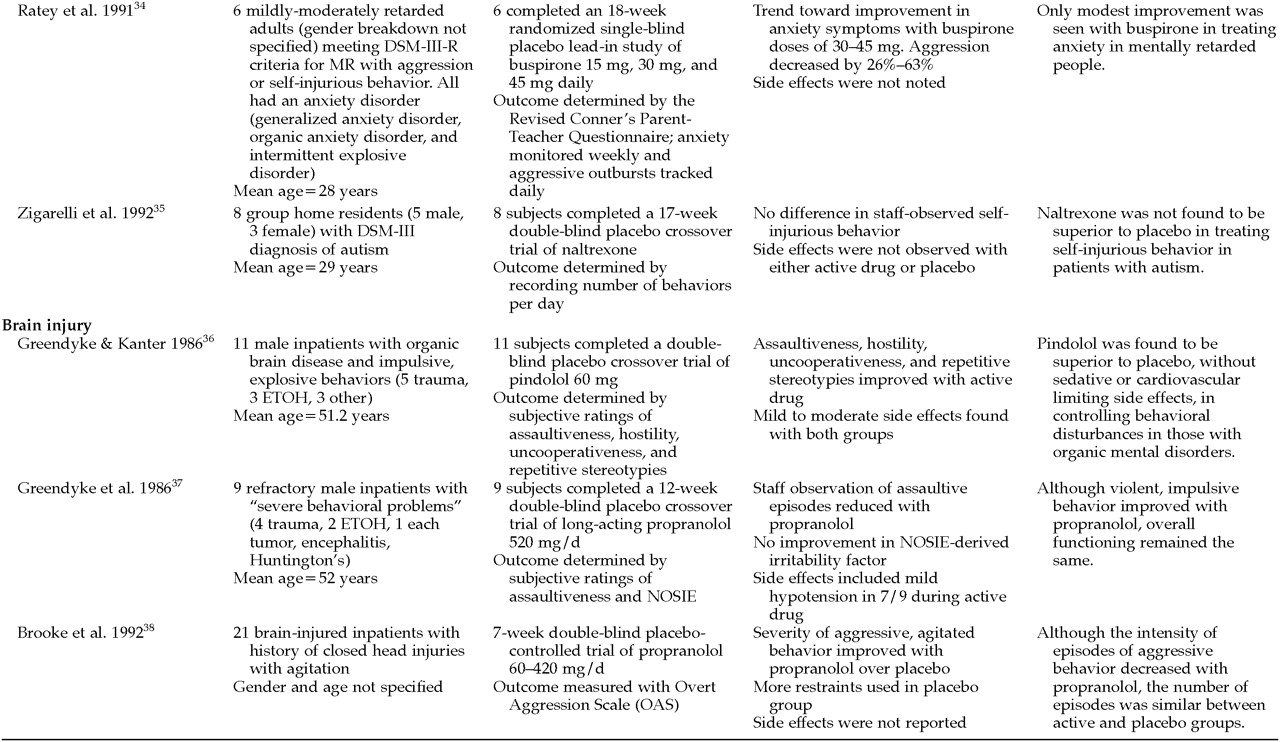
Twenty studies of the treatment of anxiety and agitation in patients with brain disease met criteria for inclusion in the study (
Table 3A,
Table 3B,
Table 3C, and
Table 3D). The symptoms of “anxiety and agitation” are not well defined, and uniform measures to assess change and ultimate outcome are lacking. Therefore, it is difficult to generalize the findings of these studies in this category. Because of this heterogeneity, a variety of agents, including antipsychotics, antidepressants, mood stabilizers, anxiolytics, beta-blockers, and naltrexone have been studied in the treatment of “anxiety and agitation” in the neurologically ill.
Antipsychotics were the most frequently studied agents for treating anxiety and agitation in individuals with dementia. Haloperidol, loxapine, and thiothixene appear to be efficacious for some symptoms.
5–7,25 However, chlorpromazine,
8 thioridazine,
7 and pimozide
26 were reported to be no more efficacious than placebo. Citalopram
27 and trazodone
28 were similar to placebo. Carbamazepine treatment gave mixed results.
29,30In those with mental retardation, anxiety and agitation appear to respond to an investigational benzodiazepine,
31 an experimental antipsychotic,
32 and lithium.
33 Buspirone produced minimal effects,
34 and naltrexone was no better than placebo.
35 Only beta-blockers, pindolol,
36 and propranolol
37,38 have been studied in brain-injured people. Although both agents produced some benefit, propranolol appears to have only limited usefulness because of its significant side effects.
DISCUSSION
Very few randomized double-blind placebo-controlled pharmacological trials are available to guide the clinician when treating psychosis, depression, or anxiety-agitation in the context of a neurological disorder. Randomized placebo-controlled studies are essential to advance our understanding of the treatment of neuropsychiatric disorders in patients with neurologic disease.
Many of the existing double-blind studies show a surprisingly robust placebo effect. This finding suggests that anecdotal observations of improvement following administration of specific agents will frequently be documenting a placebo-related effect rather than necessarily establishing a specific biochemical or pharmacologic effect. Treatment effects size also tends to vary among patients with neurological illnesses of different severities or in different stages, and the effect size may not be predictable on the basis of small samples or open-label studies. Side effects may be more common in neurologically ill patients than in patients with psychiatric disturbances without an associated neurologic disease, and treatment of a larger number of patients with active agents and placebo will help establish the spectrum of potential side effects.
Neuropsychiatric disturbances with neurologic illness may respond substantially differently from the same type of psychiatric disorder in patients without neurologic illness. For example, the cholinergic deficiency in Alzheimer's disease may alter the effect of standard or novel antipsychotics in the treatment of psychosis in this disease. Similarly, serotonergic abnormalities that follow cerebrovascular insult may alter the response to selective serotonin reuptake inhibitors for the treatment of depression. Thus, randomized, controlled studies should be conducted in patients with clearly defined neurologic illness to establish the utility of psychotropic medications in these special populations.
Conducting double-blind placebo-controlled studies in patients with neuropsychiatric disorders and neurological illnesses poses difficult challenges. Patients frequently have comorbid conditions (e.g., hypertension, cardiac or renal disease) that may complicate participation in blinded trials. Neurologically ill patients often require treatment with medications that may interact with the study agent (antihypertensives, dopaminergic agents for Parkinson's disease, or cholinergic agents for Alzheimer's disease). The application of diagnostic criteria (e.g., for depression) derived from populations of patients without neurological illness may be difficult, and current standard assessment and outcome tools are often inadequate in detecting changes that affect a patient's functional status and quality of life.
Despite these challenges, there must be a standardization of diagnostic inclusion and exclusion criteria and agreement on the rating scales and primary outcome measures to be used. In order to estimate the sample size necessary to determine a treatment effect, the placebo response rate must be determined for the psychiatric problem in each disorder. It is not wise to lump together patients with different neurological disorders who have the same psychiatric symptoms. The measurement of side effects in these vulnerable populations is just as important as the determination of the reduction in psychiatric symptoms. Attaining results that are meaningful to clinicians will require conducting class-to-class comparisons of medication, such as high-potency versus atypical neuroleptics for the treatment of psychosis in dementia, in addition to comparisons with placebo.
The population of neurologically ill patients with specific neuropsychiatric syndromes is relatively small, requiring expensive multicenter investigations to establish reasonable sample sizes. The relatively small size of the populations in question also makes conducting such studies of less financial interest to pharmaceutical companies seeking large markets. However, a number of large-scale industry-sponsored controlled trials are already under way for psychiatric symptoms in neurological patients. Some disorders, such as psychosis in dementia, involve large patient groups, which are attractive for pharmaceutical companies to study. These multicenter trials require a large sample size to demonstrate a treatment effect. For example, one placebo-controlled trial of a neuroleptic for the treatment of psychosis in dementia will require a sample of 360 patients to reach statistical significance. These trials are expensive to conduct, but they are essential for providing the scientific foundation to move the field of neuropsychiatry forward.
The American Neuropsychiatric Association and its members can play an important role in fostering controlled treatment trials for neuropsychiatric conditions. These efforts might include the following:
1.
Developing a consensus position on the most effective outcome measures in various disorders.
2.
Developing research consortia for studies in specific populations, such as the Huntington's Study Group.
3.
Working with the pharmaceutical industry and self-help/advocacy groups to design and implement these trials.
4.
Working with third-party payers to include a neuropsychiatric assessment as part of the critical pathway in neurological and psychiatric patients.
5.
Developing methods of assessing the fiscal impact of behavioral disorders in neurological patients.
6.
Using small-scale studies such as N-of-1 designs with blinded raters to establish preliminary information for treatment of some disorders.
In conclusion, people afflicted with neurologic disorders frequently develop secondary behavioral disturbances, many of which are psychiatric disorders. These disturbances result in considerable disability, caregiver stress, and financial burden. It is imperative to assess interventions—such as the use of newer psychotropic medication and the use of augmenting strategies—that may be beneficial in relieving the suffering of those with neurologic disease who are experiencing psychiatric problems.