Loss of Recent Memory After Bilateral Hippocampal Lesions
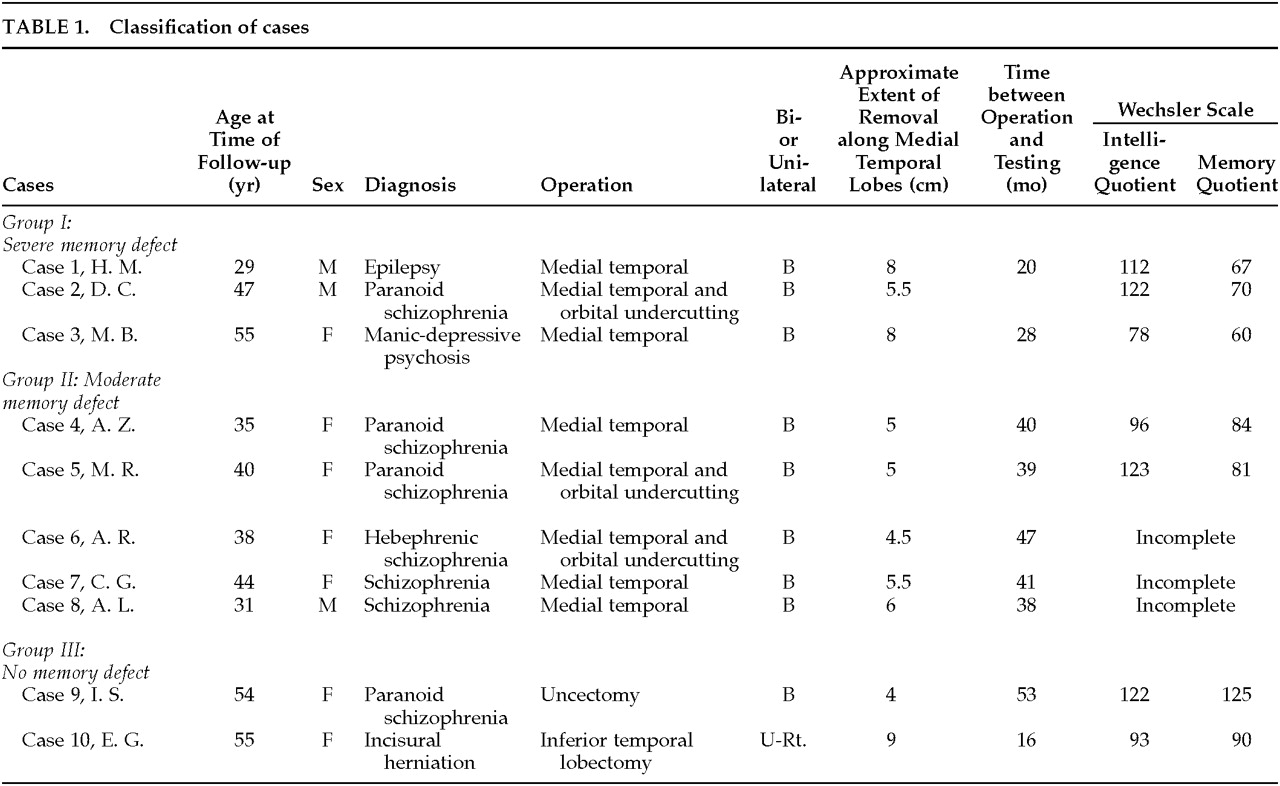
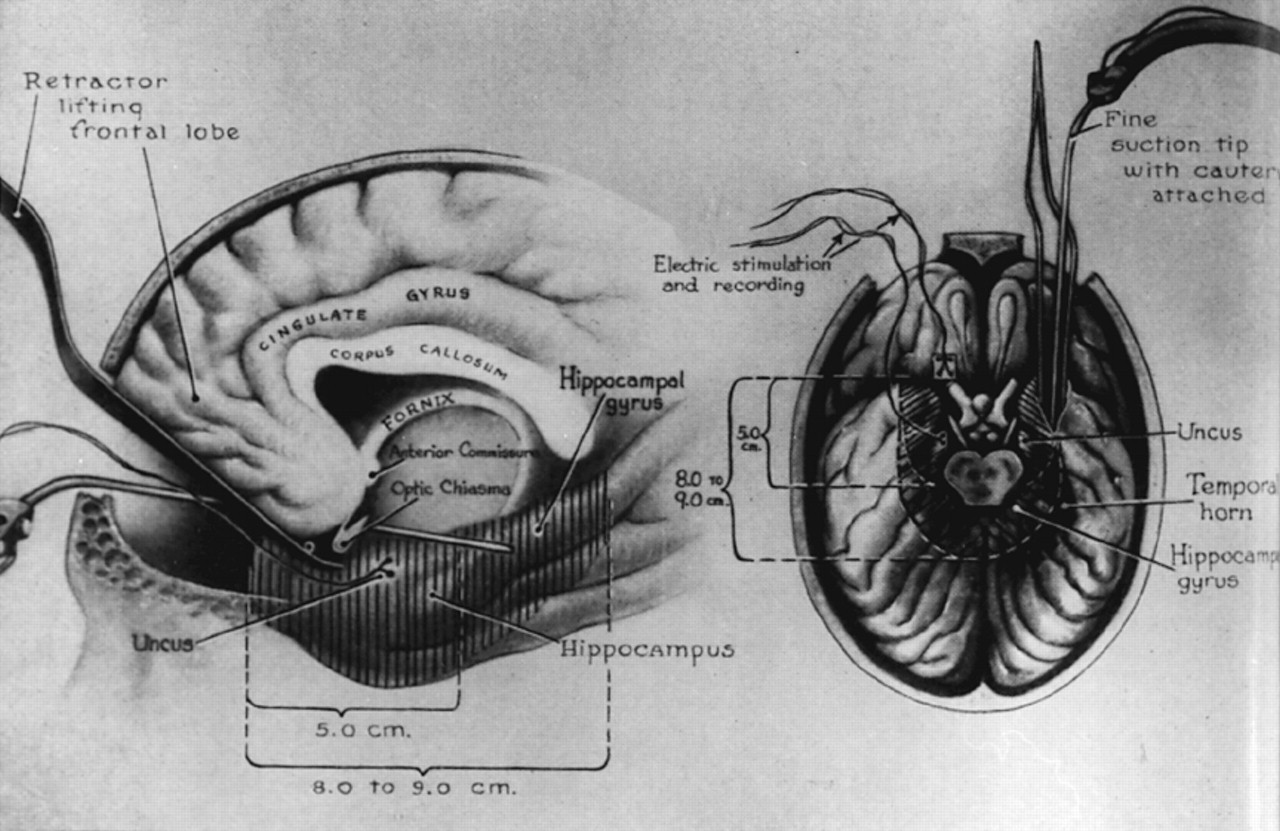
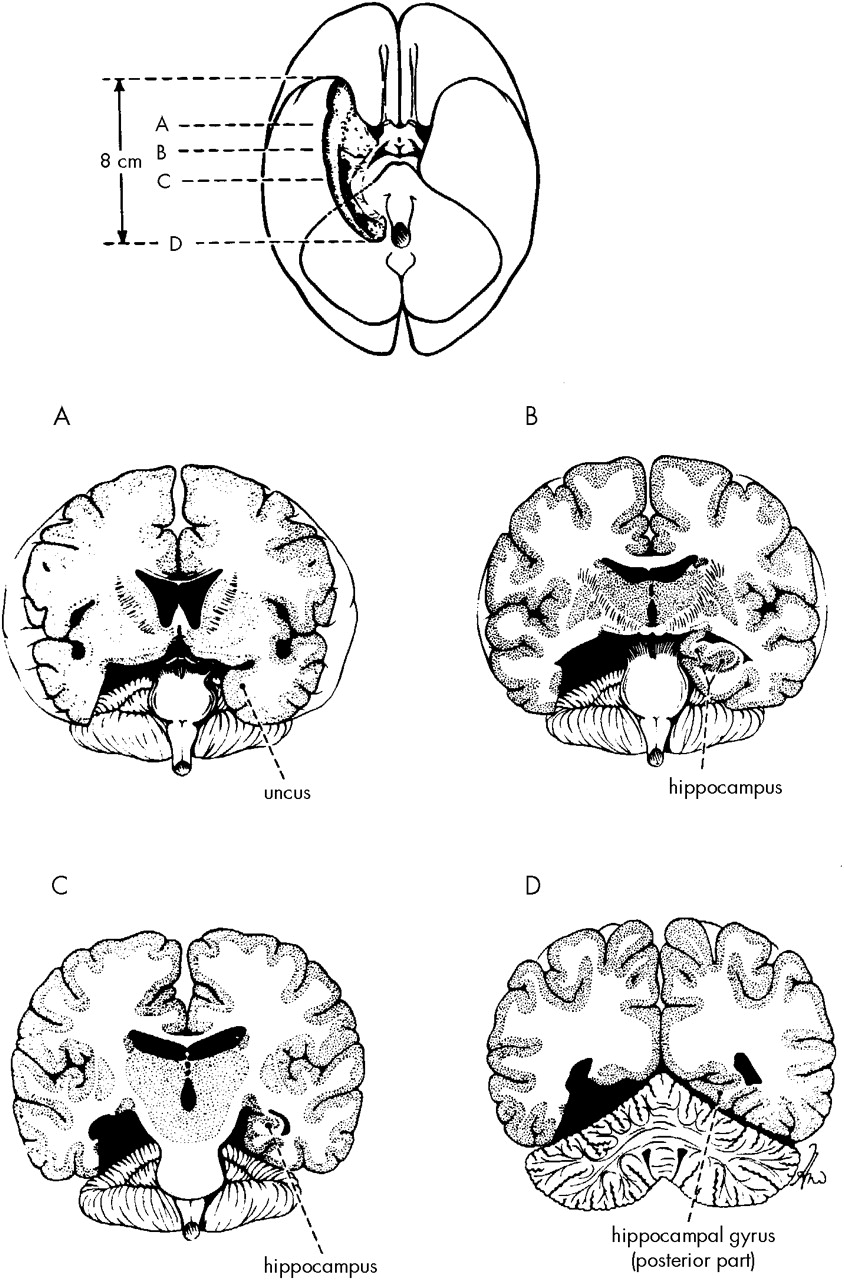
OPERATIONS
RESULTS
GROUP I: SEVERE MEMORY DEFECT
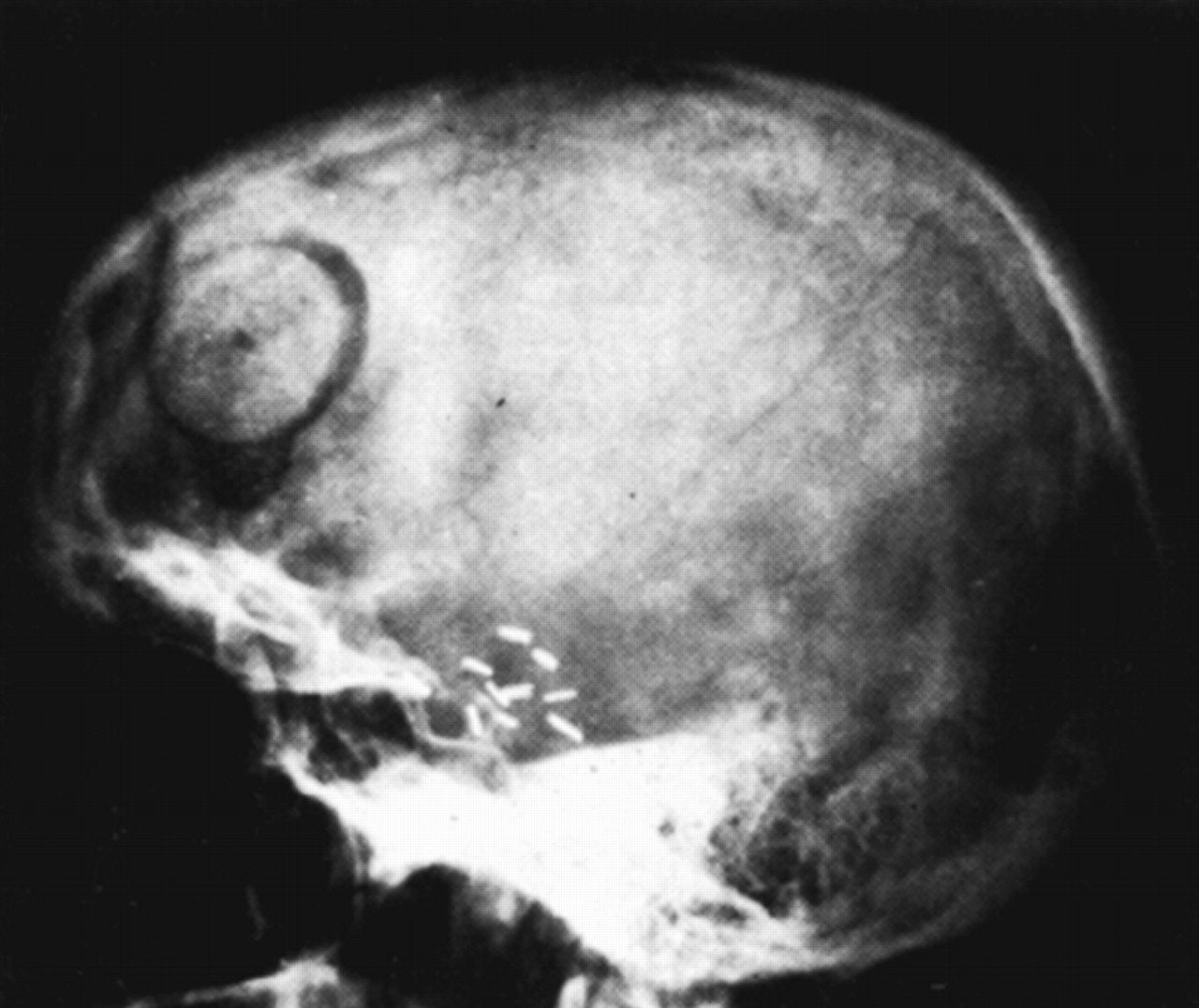
Case 1, H. M. This 29-year-old motor winder, a high school graduate, had had minor seizures since the age of 10 and major seizures since the age of 16. The small attacks lasted about 40 seconds, during which he would be unresponsive, opening his mouth, closing his eyes, and crossing both arms and legs; but he believed that he could “half hear what was going on.” The major seizures occurred without warning and with no lateralizing sign. They were generalized convulsions, with tongue-biting, urinary incontinence, and loss of consciousness followed by prolonged somnolence. Despite heavy and varied anticonvulsant medication the major attacks had increased in frequency and severity through the years until the patient was quite unable to work.The etiology of this patient's attacks is not clear. He was knocked down by a bicycle at the age of 9 and was unconscious for five minutes afterwards, sustaining a laceration of the left supra-orbital region. Later radiological studies, however, including two pneumo-encephalograms, have been completely normal, and the physical examination has always been negative.Electroencephalographic studies have consistently failed to show any localized epileptogenic area. In the examination of August 17, 1953, Dr. T. W. Liberson described diffuse slow activity with a dominant frequency of 6 to 8 per second. A short clinical attack was said to be accompanied by generalized 2 to 3 per second spike-and-wave discharge with a slight asymmetry in the central leads (flattening on the left).Despite the absence of any localizing sign, operation was considered justifiable for the reasons given above. On September 1, 1953, bilateral medial temporal lobe resection was carried out, extending posteriorly for a distance of 8 cm from the midpoints of the tips of the temporal lobes, with the temporal horns constituting the lateral edges of resection.After operation the patient was drowsy for a few days, but his subsequent recovery was uneventful apart from the grave memory loss already described. There has been no neurological deficit. An electroencephalogram taken one year after operation showed increased spike-and-wave activity which was maximal over the frontal areas and bilaterally synchronous. He continues to have seizures, but these are less incapacitating than before.Psychological Examination. This was performed on April 26, 1955. The memory defect was immediately apparent. The patient gave the date as March, 1953, and his age as 27. Just before coming into the examining room he had been talking to Dr. Karl Pribram, yet he had no recollection of this at all and denied that anyone had spoken to him. In conversation, he reverted constantly to boyhood events and seemed scarcely to realize that he had had an operation.On formal testing the contrast between his good general intelligence and his defective memory was most striking. On the Wechsler-Bellevue Intelligence Scale he achieved a full-scale IQ rating of 112, which compares favorably with the preoperative rating of 104 reported by Dr. Liselotte Fischer in August, 1953, the improvement in arithmetic being particularly striking. An extensive test battery failed to reveal any deficits in perception, abstract thinking, or reasoning ability, and his motivation remained excellent throughout.On the Wechsler Memory Scale (Wechsler, 194519) his immediate recall of stories and drawings fell far below the average level and on the “associate learning” subtest of this scale he obtained zero scores for the hard word associations, low scores for the easy associations, and failed to improve with repeated practice. These findings are reflected in the low memory quotient of 67. Moreover, on all tests we found that once he had turned to a new task the nature of the preceding one could no longer be recalled, nor the test recognized if repeated.In summary, this patient appears to have a complete loss of memory for events subsequent to bilateral medial temporal lobe resection 19 months before, together with a partial retrograde amnesia for the three years leading up to his operation; but early memories are seemingly normal and there is no impairment of personality or general intelligence.
Case 2, D. C. This 47-year-old doctor was a paranoid schizophrenic with a four-year history of violent, combative behavior. Before his illness he had been practicing medicine in Chicago, but he had always shown paranoid trends and for this reason had had difficulty completing his medical training. His breakdown followed the loss of a lawsuit in 1950, at which time he made a homicidal attack on his wife which led to his admission to hospital. Since then both insulin and electroshock therapy had been tried without benefit and the prognosis was considered extremely poor. On May 13, 1954, at the request of Dr. Frederick Gibbs and Dr. John Kendrick, a bilateral medial temporal lobe resection combined with orbital undercutting was carried out at Manteno State Hospital (W. B. S., with the assistance of Dr. John Kendrick). The posterior limit of the removal was 5 cm from the sphenoid ridge, or roughly 5.5 cm from the tips of the temporal lobes, with the inferior horns of the ventricles forming the lateral edges of resection. Recording from depth electrodes at the time of operation showed spiking from the medial temporal regions bilaterally with some spread to the orbital surfaces of both frontal lobes, but after the removal had been completed a normal electroencephalographic record was obtained from the borders of the excision.Postoperative recovery was uneventful and there has been no neurological deficit. Since operation the patient has been outwardly friendly and tractable with no return of his former aggressive behavior, although the paranoid thought content persists; he is considered markedly improved. But he too shows a profound memory disturbance. At Manteno State Hospital he was described as “confused,” because since the operation he had been unable to find his way to bed and seemed no longer to recognize the hospital staff. However, no psychological examination was made there, and on November 29, 1955, he was transferred to Galesburg State Research Institute where he was interviewed by one of us (B. M.) on January 12, 1956.Psychological Findings. This patient presented exactly the same pattern of memory loss as H. M. He was courteous and cooperative throughout the examination, and the full-scale Wechsler IQ rating of 122 showed him to be still of superior intellect. Yet he had no idea where he was, explaining that naturally the surroundings were quite unfamiliar because he had only arrived there for the first time the night before. (In fact, he had been there six weeks.) He was unable to learn either the name of the hospital or the name of the examiner, despite being told them repeatedly. Each time he received the information as something new, and a moment later would deny having heard it. At the examiner's request he drew a dog and an elephant, yet half an hour later did not even recognize them as his own drawings. On the formal tests of the Wechsler Memory Scale his immediate recall of stories and drawings was poor, and the memory quotient of 70 is in sharp contrast to the IQ level. As with H. M., once a new task was introduced there was total amnesia for the preceding one; in his own words, the change of topic confused him. This man did not know that he had had a brain operation and did not recall being at Manteno State Hospital, although he had spent six months there before the operation as well as six months postoperatively. Yet he could give minute details of his early life and medical training (accurately, as far as we could tell).
Case 3, M. B. This 55-year-old manic depressive woman, a former clerical worker, was admitted to Connecticut State Hospital on December 27, 1951, at which time she was described as anxious, irritable, argumentative, and restless, but well-orientated in all spheres. Her recent memory was normal, in that she knew how long she had been living in Connecticut and could give the date of her hospital admission and the exact times of various clinic appointments. On December 18, 1952, a radical bilateral medial temporal lobe resection was carried out, with the posterior limit of removal 8 cm from the temporal tips. Postoperatively she was stuporous and confused for one week, but then recovered rapidly and without neurological deficit. She has become neater and more even-tempered and is held to be greatly improved. However, psychological testing by Mr. I. Borganz in November, 1953, revealed a grave impairment of recent memory; she gave the year as 1950 and appeared to recall nothing of the events of the last three years. Yet her verbal intelligence proved to be normal.She was examined briefly by B. M. in April, 1955, at which time she showed a global loss of recent memory similar to that of H. M. and D. C. She had been brought to the examining room from another building, but had already forgotten this; nor could she describe any other part of the hospital although she had been living there continuously for nearly three and a half years. On the Wechsler Memory Scale her immediate recall of stories and drawings was inaccurate and fragmentary, and delayed recall was impossible for her even with prompting; when the material was presented again she failed to recognize it. Her conversation centered around her early life and she was unable to give any information about the years of her hospital stay. Vocabulary, attention span, and comprehension were normal, thus confirming Mr. Borganz' findings.
GROUP II: MODERATELY SEVERE MEMORY DEFECT
Case 4, A. Z. This 35-year-old woman, a paranoid schizophrenic, had been in Connecticut State Hospital for three years and extensive electroshock therapy had been tried without lasting benefit. She was described as tense, assaultative, and sexually preocccupied. On November 29, 1951, bilateral medial temporal lobe resection was carried out under local anesthesia, the posterior limit of the removal being approximately 5 cm from the tips of the temporal lobes. During subpial resection of the right hippocampal cortex the surgeon inadvertently went through the arachnoid and injured by suction a portion of the right peduncle, geniculate, or hypothalamic region with immediate development of deep coma. The injury was visualized by extra-arachnoid inspection. Postoperatively the patient remained in stupor for 72 hours and exhibited a left spastic hemiplegia, contracted fixed pupils, strabismus, and lateral nystagmus of the right eye; vital signs remained constant and within normal limits. She slowly recovered the use of the left arm and leg and her lethargy gradually disappeared. By the seventh postoperative day she could walk without support and pupillary responses had returned to normal. The only residual neurological deficit has been a left homonymous hemianopia. Of particular interest was the dramatic postoperative improvement in her psychotic state with an early complete remission of her delusions, anxiety, and paranoid behavior. At the same time she showed a retrograde amnesia for the entire period of her illness.This patient was discharged from the hospital nine months after operation and is now able to earn her living as a domestic worker. However, she complains that her memory is poor, and psychological examination (April 27, 1995) three and a half years postoperatively confirms this. But the deficit is less striking than in the three cases reported above. This patient, for example, was able to give the address of the house where she worked although she had been there only two days, and she could even describe the furnishings in some detail although she had not yet learned the name of her employer. She was also able to give an accurate, though sketchy, description of a doctor who had spoken to her briefly that morning and whom she had never seen before. However, she could recall very little of the conversation.Formal testing at this time showed her intelligence to lie within the average range with no impairment of attention or concentration. The Wechsler-Bellevue IQ rating was 96. On the Wechsler Memory Scale her immediate recall of stories was normal, but passing from one story to the next was enough to make her unable to recall the first one, though a few fragments could be recovered with judicious prompting. She showed the same rapid forgetting on the “visual retention” subtest, indicating that the memory impairment was not specific to verbal material. Finally, she was conspicuously unsuccessful on the “associate learning” subtest, failing to master a single unfamiliar word association. This examination as a whole provides clear evidence of an impairment of recent memory.
Case 5, M. R. This 40-year-old woman, a paranoid schizophrenic with superimposed alcoholism, had been a patient at Norwich State Hospital for 11 years, receiving extensive electroshock therapy. Bilateral medial temporal lobe resection combined with orbital undercutting was carried out on January 17, 1952, the posterior extent of removal being roughly 5 cm from the temporal tips. The patient has shown complete remission of psychotic symptoms and was discharged from the hospital on September 16, 1954, to the care of her family.Psychological Examination. This was performed on April 29, 1955. Tests showed this woman to be of superior intelligence, with a full-scale IQ of rating of 123 on the Wechsler Scale. However, she complained of poor memory, adding that she could remember faces and “the things that are important,” but that, to her great embarrassment, she forgot many ordinary daily happenings. Upon questioning she gave the year correctly but did not know the month or the day. She knew that she had had an operation in 1952 but did not recognize the surgeon (W. B. S.) nor recall his name. Formal testing revealed the same pattern of memory disturbance as A. Z. had shown, and the memory quotient of 81 compares most unfavorably with the high IQ rating. In conversation, she reverted constantly to discussion of her work during the years of depression and showed little knowledge of recent events.
Case 6, A. R. This 38-year-old woman had been in hospital for five years with a diagnosis of hebephrenic schizophrenia. Before operation she was said to be noisy, combative, and suspicious, and electroshock therapy had caused only transient improvement in this condition. On May 31, 1951, bilateral medial temporal lobe resection combined with orbital undercutting was carried out, the posterior limit of removal being slightly less than 5 cm from the bisected tips of the temporal lobes. After operation the patient gradually became quieter and more cooperative and on September 29, 1952, she was discharged to her home. There have been no neurological sequelae.Psychological Examination. This was performed in April, 1955. Examination revealed a hyperactive woman, too excited and talkative for prolonged testing. She showed a restricted span of attention but scores on verbal intelligence tests were within the dull normal range. Moreover, she appeared to recall some recent happenings quite well. Thus, she knew that her daughter had caught a 7 o'clock train to New York City that morning to buy a dress for a wedding the following Saturday. She could also describe the clothes worn by the secretary who had shown her into the office. However, on formal testing some impairment of recent memory was seen, although unlike the other patients in this group she did succeed on some of the difficult items of the “associate learning” test. As with A. Z. and M. R., the deficit appeared most clearly on tests of delayed recall after a brief interval filled with some other activity. Thus, on the “logical memory” test she gave an adequate version of each story immediately after hearing it, but passing from one story to the next caused her to forget the first almost completely; similar results were obtained for the recall of drawings. We conclude that this patient has a memory impairment identical in type to that of the other patients in this group, but somewhat milder. It is interesting that she had a relatively small excision.
Case 7, C. G. This 44-year-old schizophrenic woman had been in the hospital for 20 years without showing any improvement in her psychosis. On November 19, 1951, bilateral medial temporal lobe resection was carried out under local anesthesia, the posterior limit of removal being 5.5 cm from the tips of the temporal lobes. There was temporary loss of consciousness during the resection but the patient was fully conscious at the end of the procedure and postoperative recovery was uneventful. There has been no neurological deficit. She is considered to be in better contact than before but more forgetful.This patient was examined at Norwich State Hospital in April, 1955, and although she was too distractible for prolonged testing, it was possible to show that she remembered some recent events. For example, she knew that she had been working in the hospital beauty parlor for the past week and that she had been washing towels that morning. Yet formal memory testing revealed the same deficit as that shown by A. Z. and M. R., though less extensive data were obtained in this case.
Case 8, A. L. This 31-year-old schizophrenic man had been a patient at Norwich State Hospital since October, 1950. He had first become ill in August, 1950, demonstrating a catatonic type of schizophrenia with auditory and visual hallucinations. On January 31, 1952, bilateral medial temporal lobe resection combined with orbital undercutting was carried out, the removal extending posteriorly for a distance of 6 cm along the mesial surface of the temporal lobes. Recovery was uneventful and no neurological deficit ensued. The patient has been more tractable since the operation but he is still subject to delusions and hallucinations. He is said to have a memory defect. When interviewed by B. M. in April, 1955, he was found to be too out of contact for extensive formal testing. However, he was able to recall the examiner's name and place of origin 10 minutes after hearing them for the first time, and this despite the fact that the interval had been occupied with other tasks. He could also recognize objects which had been shown to him earlier in the interview, selecting them correctly from others which he had not seen before. But his immediate recall of drawings and stories was faulty and these were forgotten completely once his attention was directed to a new topic.In this patient we stress the negative findings: despite his evident psychosis he did not show the severe memory loss typical of the patients in Group I. Yet the brief psychological examination and the hospital record both indicate some impairment of recent memory, though no reliable quantitative studies could be made.
Case 9, I. S. This 54-year-old woman had a 20-year history of paranoid schizophrenia, with auditory hallucinations and marked emotional lability. She had attempted suicide on several occasions. On November 16, 1950, six months after admission to a state hospital, a bilateral medial temporal lobectomy was carried out under local anesthesia with sectioning of the tips of the temporal lobes and subpial suction removal of the medial portion, extending back 4 cm to include the uncus and amygdala. Thus this was a conservative bilateral removal, sparing the hippocampal region. The operation was complicated by accidental damage to the midbrain from the electrocautery, causing the patient to give a convulsive twitch which was followed by coma and extensive rigidity. After operation she was somnolent for a time with continuing rigidity, more marked on the left side than on the right. Vital signs were normal. She required traction to prevent flexure spasm contractures. There was slow improvement over the ensuing two months, with some residual clumsiness and spasticity of gait. For a time the patient's mental state was worse than before operation, but within three months she had improved markedly, with increased gentleness, diminished auditory hallucinations, and no depression. She ultimately showed the best result of all the cases in this series and was discharged from the hospital five months after operation.This patient was reexamined on May 11, 1956. She shows a complete remission of her former psychotic behavior and is living at home with her husband and leading a normal social life. Her hallucinations have ceased. Upon neurological examination she shows some 25% residual deficit, manifested chiefly by spastic incoordination of gait and similar but less marked incoordination of the arms. The deep leg reflexes are increased to near clonus, but there is no Babinski sign. Arm reflexes are moderately increased and abdominal reflexes absent. Smell is completely lost but all other sense modalities are intact and other cranial nerves normal.Psychological Findings. The patient was examined psychologically in April, 1955. From the standpoint of memory, this patient presents a complete contrast to the cases reported above, obtaining excellent scores for both immediate and delayed recall of stories, drawings, and word associations, and describing accurately episodes from the relatively early postoperative period. The memory quotient of 125 is consistent with the IQ level of 122, and both would be classed as superior. This is so despite prolonged psychosis, intensive electroshock therapy, and brainstem damage of undetermined extent.
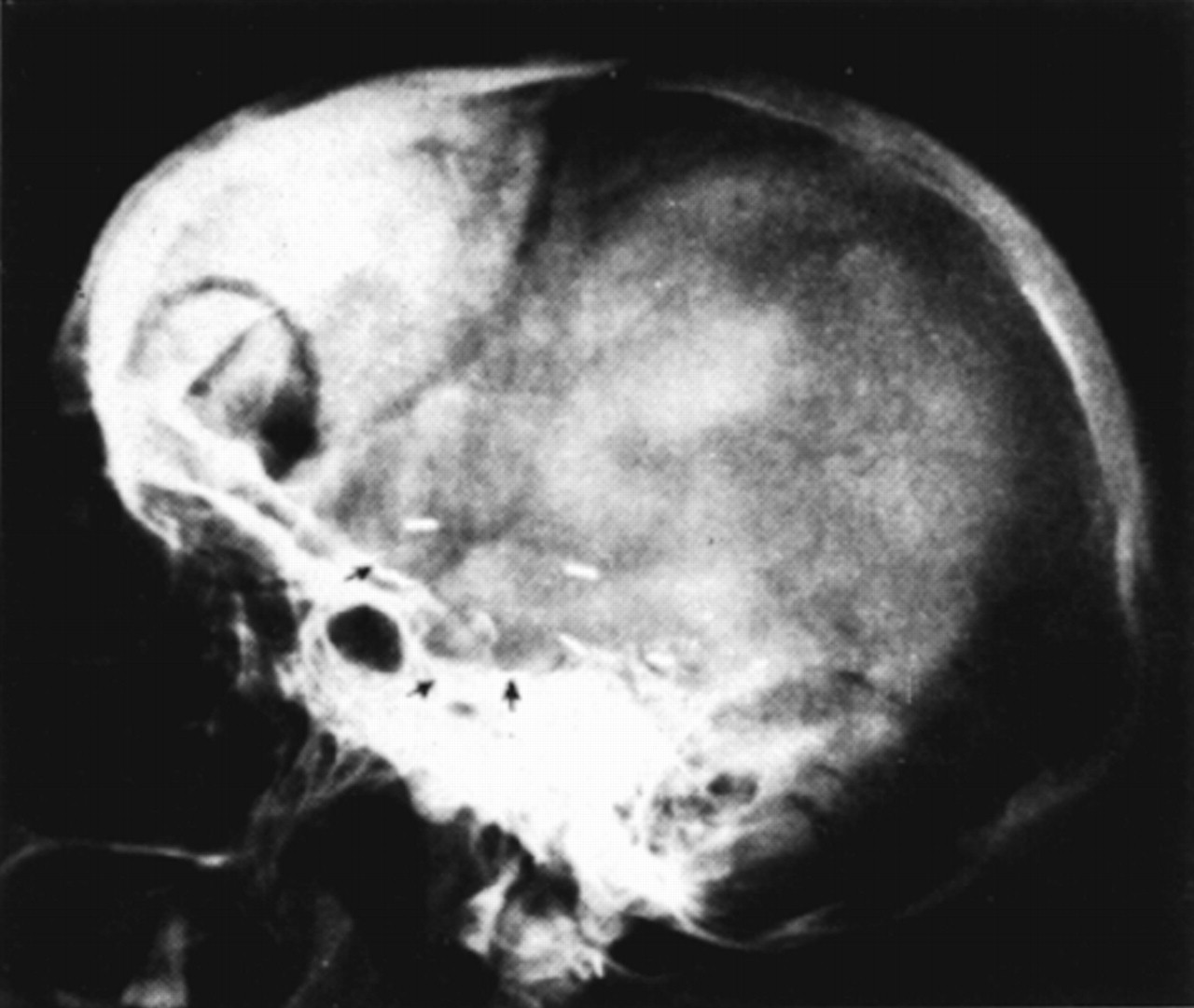
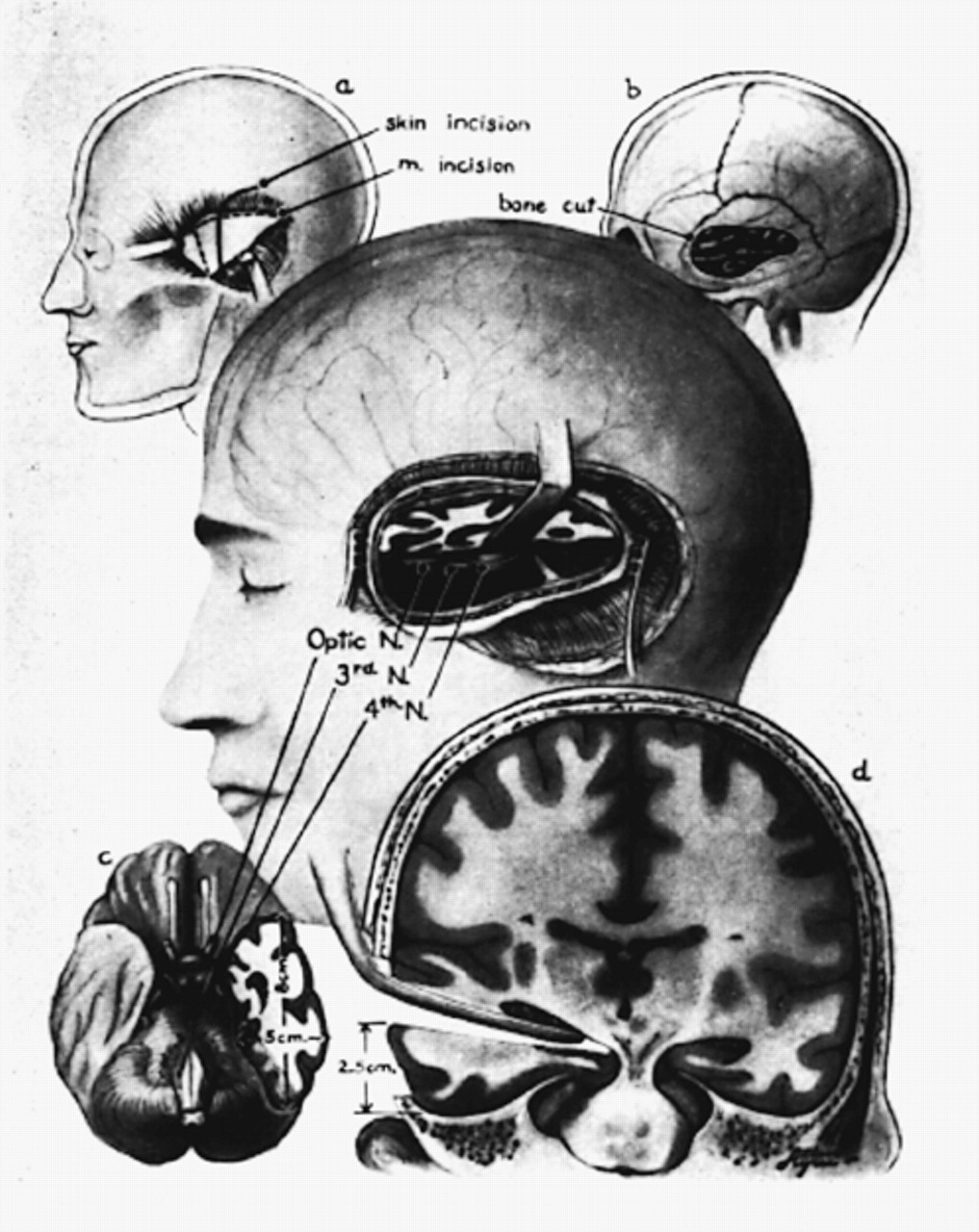
Case 10, E. G. This 55-year-old woman developed malignant edema after removal of a huge, saddle-type meningioma from the right sphenoid ridge; the pupils were dilated, she lost consciousness, and vital signs began to fail. A diagnosis of incisural hippocampal herniation was made, and, as a life-saving measure, unilateral nondominant inferior temporal lobectomy was carried out, with deliberate resection of the hippocampus and hippocampal gyrus to a distance of 9 cm from the tip of the temporal lobe. (The operative procedure is illustrated in Figure 5.) Vital signs improved immediately and consciousness gradually returned, but for a few weeks the patient showed a disturbance of recent memory resembling that seen in our bilateral cases. However, follow-up studies in April, 1955, 16 months after operation, showed no residual memory loss. Both immediate and delayed recall were normal and the memory quotient of 90 was completely consistent with the IQ level of 93. Neurological examination at this time showed a left homonymous visual field defect with macular sparing but no other deficit.
DISCUSSION
SUMMARY
References
Information & Authors
Information
Published In
History
Authors
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBGet Access
Login options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).