Changes in personality and affect have been recognized in multiple sclerosis (MS) for more than a century,
1 and recent investigators delineate three primary affective disorders: depression, pathological laughing/crying, and euphoria.
2–4 Most agree that these disorders may result from either psychological reaction to the stress of MS (depression) or cerebral pathology. An early neuropsychological study
5 distinguished between acute mood disorders and more stable, character-related changes in MS. Regarding the latter, observations suggested an acquired disposition toward irritability or apathy in one-third of patients studied and sexual disinhibition in a smaller number. A weakness in this and other studies
6–10 was the use of semistructured interviews that are subject to interviewer bias and poor reliability, and/or psychometric tests (e.g., Minnesota Multiphasic Personality Inventory) that confound the influence of acute psychiatric disorder (such as depression) with changes in personality traits.
More recently, a consensus has emerged that the “five-factor” theoretical model of personality covers the gamut of traits comprising the most widely recognized personality theories.
11–16 The five-factor model includes the following statistically independent factors or domains: Neuroticism, Extraversion, Openness to Experience, Agreeableness, and Conscientiousness. These specific domains of personality can now be assessed with the revised version of the NEO Personality Inventory (NEO-PI),
12 a standardized, comprehensive, questionnaire-format test with well-established reliability and validity. Although the NEO-PI is commonly used in psychiatric settings, the instrument has rarely been applied to neurological patients.
METHODS
Subjects
Thirty-four patients with laboratory or clinically definite MS
20 were referred for evaluation of cognitive dysfunction or responded to an advertisement for MS patients with emotional problems. In addition to neuropsychological evaluation, patients underwent magnetic resonance imaging (MRI) and neurological examination to derive an Expanded Disability Status Scale (EDSS) rating.
21 Some patients also participated in an experimental trial of a newly developed psychological intervention designed to diminish the frequency of socially aggressive behaviors. The results of the MRI and the psychological study will be presented in separate reports.
Twenty-one patients had a progressive form of MS and 13 had relapsing disease. EDSS scores ranged from 1.0 to 8.5 (mode=3.0). There were 32 Caucasian patients and 2 African Americans. The male/female ratio was 13/21 (62% female).
Fourteen normal volunteers (12 women, 2 men), all Caucasian, matched to the MS group on age and education, were also studied as control subjects.
All participants were seen with an informant who provided collateral information for the history and completed questionnaires pertaining to the primary participant's personality. Among patients, 68% (23) of the informants were spouses, 23% (8) were parents, and 9% (3) were domestic partners or friends. Among control subjects, the informant roles were 83% (12) spouse, 7% (1) parent, 14% (2) domestic partner or friend. The proportion of informants in each category did not differ across groups by chi-square test (χ2=3.3, P=0.50).
Exclusion criteria included history of neurological disease other than MS (or for control subjects, any neurologic disease), drug or alcohol dependence, psychiatric disease other than psychological problems attributable to MS, or clinical MS relapse (or steroid treatment) within 3 weeks prior to participation.
Measures
Depression was quantified by use of the Beck Depression Inventory (BDI).
22 Cognitive tests, based on previous studies of dementia and MS,
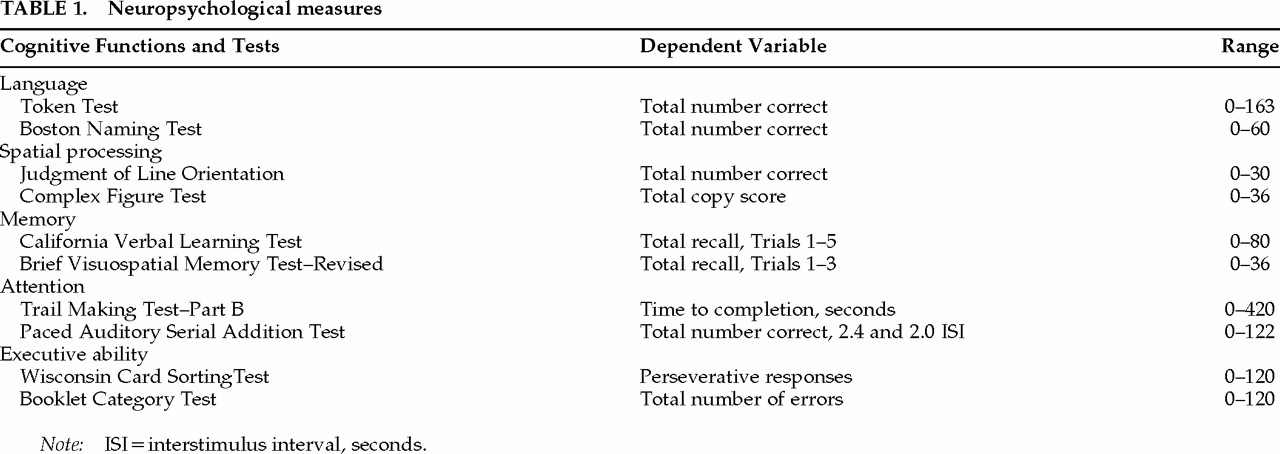
23,24 were reduced to 10 variables for statistical analysis (
Table 1). Language was assessed by the University of Victoria version of the Token Test
25 and the Boston Naming Test.
26 Spatial processing was assessed with the Judgment of Line Orientation Test
27 and the copy administration of the Complex Figure Test.
28 The California Verbal Learning Test
29 and the Brief Visuospatial Memory Test–Revised
30 assessed new learning and memory. Attention and/or rate of processing was examined by the Trail Making Test, Part B,
31 and the Paced Auditory Serial Addition Test.
32 The Wisconsin Card Sorting Test
33 and the Booklet Category Test
34 were employed to measure higher executive ability.
Interpersonal empathy was assessed with a 15-item, adapted version of the Hogan Empathy Scale (HES).
35 Higher scores indicate a greater degree of empathy in social situations. Personality was further evaluated with the revised NEO Personality Inventory (NEO-PI),
12 including the five domain scores as follows: Neuroticism, Extraversion, Openness, Agreeableness, Conscientiousness. In accordance with the five-factor model, Neuroticism refers to the degree of emotional responsiveness and proclivity for negative affect. Extraversion refers to dependence upon external stimulation for arousal; that is, extroverts are outgoing and sensation seeking. Openness reflects one's desire for new knowledge, ideas, and experiences. Agreeableness is the desire for socialization, honesty, and altruism in relationships. Conscientiousness is the proclivity to be well organized and deliberate. Domain subscale scores (six for each domain) were also examined in some analyses, as described below. The raw scores derived from the NEO-PI were converted to T-scores (mean=50, SD=10), with higher scores indicating a stronger endorsement of each personality trait. All informants for MS patients and control subjects completed these tests without assistance. Some MS patients had questions read to them to avoid fatigue.
Discrepancy scores were calculated for the HES and each NEO-PI domain score. In each case, differences between self and informant report were calculated and the absolute value of the difference recorded. Absolute differences in raw scores were employed for the HES, and differences in T-scores were employed for the NEO-PI.
Procedure
All participants underwent an initial structured telephone screening interview, emphasizing DSM-IV
36 criteria for psychiatric disorders. Mood and substance-related disorders were covered in detail to rule out previously untreated disease. After screening, participants underwent neuropsychological and neurological examinations. (Control subjects completed only the personality and neuropsychological tests.) Neuropsychological testing was performed by a trained technician supervised by a board-certified clinical neuropsychologist. All participants provided signed, Institutional Research Board–approved, informed consent.
Statistical Analyses
First, group means were compared by Student's t (cognitive and informant-reported personality) and paired-sample t-tests (patient vs. informant reports), which were considered reliable only where P<0.01 to control for Type I error. Dependent measures included the cognitive measures; BDI; HES; the primary NEO-PI scale scores for Neuroticism, Extraversion, Openness, Agreeableness, and Conscientiousness; and self/informant discrepancies for the HES and NEO-PI.
Second, linear regression analyses (forward selection, entrance criterion of 0.05, exit criterion of 0.10) were performed to identify cognitive variables that predict abnormal HES and NEO-PI ratings. EDSS and BDI were entered into each regression analysis first (block 1), to control for the influence of physical disability and depression in estimating the association between cognition (block 2) and each personality domain (dependent variable). These analyses included NEO-PI subscales within each primary scale, but the Openness domain was excluded because this scale did not discriminate patients and control subjects in the first analysis.
Third, a similar regression analytic strategy was used to examine the association between cognitive impairment and self/informant discrepancy scores. Only those personality measures in which the self and informant report values differed significantly were examined (HES, NEO-PI Conscientiousness). Because the specific content within personality domains was considered unimportant in evaluating the relationship between discrepancy scores and cognition, these analyses did not include NEO-PI subscale scores.
RESULTS
Comparisons of Patients and Control Subjects
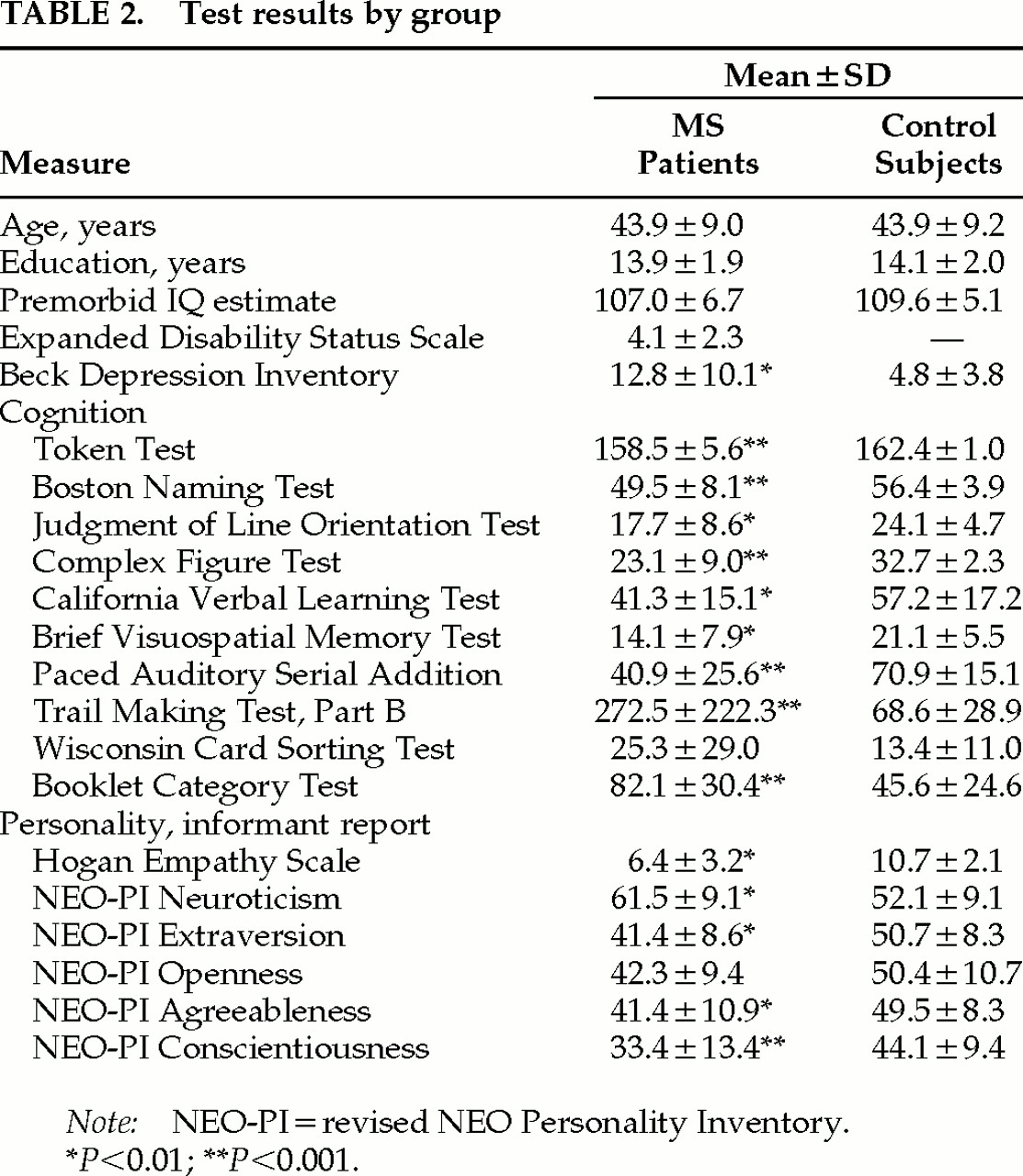
Although the groups were well matched on age, education, and estimated premorbid IQ (
Table 2),
37 MS patients performed more poorly than control subjects on nearly every cognitive test. MS patients were more depressed on the BDI (
P<0.01).
MS patients were rated lower on the HES, as well as on NEO-PI Extraversion (P<0.01), Agreeableness (P<0.01), and Conscientiousness (P<0.01). Patients were rated significantly higher on Neuroticism (P<0.01).
There were no significant differences between self and informant reports among control subjects, but MS patients generated higher self-ratings in comparison to those of informants on the HES (P<0.01). Patients also rated themselves significantly higher in Conscientiousness (P<0.001).
Cognitive Predictors of Abnormal Personality
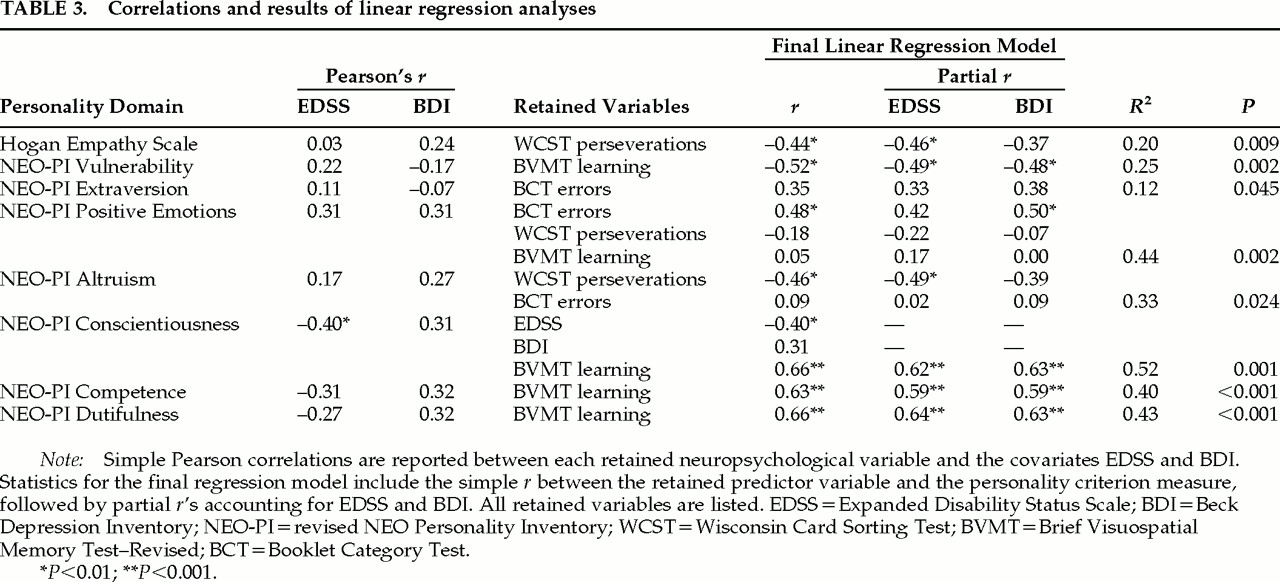
Linear regression analyses were performed to identify neuropsychological variables that predict abnormal personality ratings by informant report (
Table 3). EDSS was significantly correlated with Conscientiousness (
r=−0.40), but there were no other reliable correlations between EDSS or BDI and the informant-report personality indices. When EDSS and BDI were controlled in subsequent regression analyses, significant relationships emerged between personality and tests of executive function (Wisconsin Card Sorting Test perseverative responses, Booklet Category Test errors) and visual learning (Brief Visuospatial Memory Test recall). Executive tasks were significant predictors in regression models for low ratings on HES and Altruism, and elevated ratings on Positive Emotions. Impaired learning significantly predicted increased Vulnerability, and low ratings within the Conscientiousness domain (Competence, Dutifulness). EDSS and BDI were retained in only one final regression model (Conscientiousness), and in this case, visual learning was the strongest predictor.
The strength of association between neuropsychological and personality measures can be shown by way of partial correlations (
Table 3), which control for the influence of EDSS and BDI. These partial
r's were statistically reliable for HES, Vulnerability, Positive Emotions, Altruism, Conscientiousness, Competence, and Dutifulness.
Cognitive Predictors of Self/Informant Disagreements
Both Wisconsin Card Sorting Test perseverations and Complex Figure Test copy scores were retained in the final model predicting mean discrepancy score on HES (R2=0.29, P=0.011). Perseverations, the highest-loading predictor, was associated with greater patient/informant disagreement. The partial correlation between perseverations and HES discrepancy, controlling for EDSS, was marginally significant (r=0.39, P<0.05), and the partial r controlling for BDI was not reliable.
In the model predicting NEO-PI Conscientiousness disagreements, only the Wisconsin Card Sorting Test was retained (R2=0.31, P=0.001). Although EDSS and BDI were not retained in the model, lower BDI scores (r=−0.28) and higher EDSS scores (r=0.31) were modestly associated with greater patient/informant disagreement (R2=0.24, P=0.003). Partial correlations between perseverations and Conscientiousness discrepancy scores, controlling for EDSS (r=−0.57, P<0.01) and BDI (r=0.54, R<0.015), were both reliable.
DISCUSSION
We report evidence of abnormal personality traits in MS that are similar to those previously described in patients with probable Alzheimer's disease,
17–19 using a comprehensive test of personality that encompasses the full spectrum of traits widely recognized in the psychological literature.
11–16 Compared with normal control subjects, cognitively impaired MS patients were more neurotic and were less empathic, agreeable, and conscientious. In other words, they were judged by friends and relatives as emotionally overreactive, more irritable, and more tense than normal. They were also considered less outgoing, deliberate, and appreciative of the thoughts and feelings of others. Similar traits were found previously in Alzheimer's disease by using the NEO-PI, suggesting that our data may be demonstrating a more general dementia personality profile.
17–19 Further research that includes patient control samples will be needed before conclusions can be made regarding the specificity of these personality findings to MS.
This is the first study to compare patient self-reports and informant reports in MS using the same validated personality instrument. Some of our patients acknowledged personality changes on the NEO-PI and HES tests, but they more often overestimated their capacity for empathy and conscientiousness. Thus, our MS patients had little insight into their maladaptive behavior patterns and personality traits. Previous NEO-PI research demonstrated that self and informant reports yielded similar data, even in severely depressed samples.
38 Such data support the idea that acute psychiatric symptoms can be differentiated from trait measures of personality and that the NEO-PI yields valid results in psychiatric patients. Our current findings, in contrast, suggest that NEO-PI
self-reports are confounded with dementia. We would note that the validity of
informant reports in cognitively impaired samples has not been well studied. It is possible that family members may develop biases pertaining to patient behavior during the course of a debilitating illness such as MS or Alzheimer's disease.
As questionnaire measures, the NEO-PI and HES involve the capacity for language (reading, language comprehension), and thus dementia could confound their interpretation. However, we believe that the discrepancies between patient and informant ratings were not due to test-taking artifacts for several reasons. First, language is relatively preserved in MS, and the test questions were read to patients (or they were otherwise assisted) when necessary. Second, patient/informant discrepancies were apparent only in the areas of empathy and conscientiousness, suggesting that these disagreements were due to poor self-awareness. If the lack of agreement were due to testing artifact, discrepancies would likely appear in all personality domains. The presence of discrepancies only in empathy and conscientiousness suggests that patients have greater difficulty recognizing their errors and handicaps in these areas, in contrast to changes involving sadness, confidence, and other aspects of neuroticism and extraversion.
The generalizability of our findings might be questioned because our patients responded to advertisements regarding the presence of “emotional problems.” On the other hand, depression is quite common in MS,
39–41 and recent prevalence estimates place the MS patient's lifetime risk for depression, conservatively defined by structured psychiatric interview, at roughly 50%.
42 Furthermore, the mean BDI obtained in our sample is similar to that reported in other clinical MS samples.
43 Thus, although our sample may have been more psychiatrically impaired than a random, community-based sample, the results can be generalized to other clinic samples. As expected, correlations between high BDI and EDSS scores and abnormal personality ratings were significant, or approached significance. However, the association between defects in personality and cognitive impairment remained after controlling for these factors statistically.
Limitations in our methodology prevent us from reaching definite conclusions regarding the acquisition of this syndrome. The hypothesis that the disorder is acquired is supported only indirectly by the concordance between our objective findings and previous case reports of acquired euphoria
3,4 and its reported correlations with cognitive dysfunction. A stronger method would involve examining a random sample of recently diagnosed cases and performing repeat exams at designated intervals that would allow for the development of the disorder (e.g., 5 to 10 years).
Our findings differ from those in previous studies of the NEO-PI and cognition in Alzheimer's disease patients,
17–19 where there was no correlation between cognitive function and personality change. The lack of correlation in these studies might be due to limited sensitivity of the Folstein Mini-Mental State Examination, which was the only measure of cognitive function employed. It is also possible that dementia and personality traits simply overlap to a greater degree in MS than in Alzheimer-type dementia.
Although euphoria is usually regarded as a primary affective disorder in MS,
5 it may be more accurately construed as a change in trait or character that includes rapid vacillations in mood (including anger, dysphoria, and euphoria), unrealistic optimism, denial, and/or inappropriate social behavior.
3,41 Our findings are consistent with this view of euphoria in that our patients were rated as being quite low in empathy and conscientiousness and high in neuroticism. The association between these traits and cognitive dysfunction supports the idea that the personality changes are neurogenic.
We identified three commonly used neuropsychological tests that predict the presence of these abnormal personality traits (Wisconsin Card Sorting Test, Booklet Category Test, Brief Visuospatial Memory Test). Viewed collectively, these measures appear to involve executive abilities such as freedom from perseveration, conceptualization, visual working memory, and new learning. This executive aspect of neuropsychological function was associated in particular with reduced empathy and altruism, as well as elevation in positive mood states such as optimism and humor—traits that are often included in descriptions of pathological euphoria.
3 These same measures were correlated with reduced conscientiousness on the NEO-PI, although impaired visual learning accounted for the most variance in this domain. Overall, these significant associations between personality and executive ability suggest that this disorder may be caused by frontal lobe dysfunction, a possibility we are now investigating by MRI measurements of MS patients with this syndrome.