In 1962, the American Medical Association’s Committee on Medical Aspects of Sports organized a conference addressing head protection in athletes and associated matters in sports medicine.
5 A greater understanding of the need to determine patterns of injury in order to reduce morbidity in the professional and recreational athletic arenas resulted. Although football was the main focus on the American front, emphasis was placed on head protection in other sports arenas elsewhere. In Sweden, for example, the use of hockey helmets became mandatory in 1963. This was subsequent to an insurance survey that found over 100 closed head injuries, including 1 death, 22 mild traumatic brain injuries (MTBIs) and 3 facial fractures as a result of hockey participation.
9Today, multiple sports are associated with concussive events. In excess of 1.5 million people participate in football (i.e. recreational, high school, collegiate, and professional) annually. The estimated annual incidence of MTBI’s in football is 4–20%.
5 A systematic review of the literature from 1985 to 2000 found ice hockey and rugby to have the highest incidence of concussion for high school, college, and amateur athletes, while soccer had the lowest.
10 At the recreational level, female taekwondo participants and male boxers had the highest frequency of concussion.
10 Of the injuries, 6.2% were concussive in a three-year prospective study among intercollegiate athletes.
11 According to a survey of 1,659 children participating in contact sports, 3% suffered concussions.
12 In addition, an epidemiologic study of collegiate and high school football players found that players who sustain one concussion are three times more likely to sustain a second one in the same season.
13Concussion and Postconcussive Syndrome
The term concussion is derived from the Latin word
concutere (to strike together).
14 Another synonymous term,
commotion cerebri, was introduced in the 16
th century by the French military surgeon Pare.
15 Although the symptoms associated with concussion have been recognized for centuries, the term “postconcussion syndrome” was first used in 1934 to describe the “subjective posttraumatic syndrome…due directly to the blow on the head.”
16,17 Symptoms associated with postconcussion syndrome may include persistent headache, irritability, inability to concentrate, memory impairment, generalized fatigue, dizziness, or a generalized loss of well-being. Commonly, the course is self-limited, resolving usually within 6-8 weeks of the incident.
5Most recently, it has been recognized that MTBI may occur as a result of concussion. The Centers for Disease Control and Prevention (CDC) Mild Traumatic Injury Workgroup conceptually defined MTBI as “an injury to the head as a result of blunt trauma or acceleration or deceleration forces that result in one or more of the following conditions: (1) Any period of observed or self-reported transient confusion, disorientation, impaired consciousness, dysfunction of memory around the time of injury, or loss of consciousness lasting less than 30 minutes. (2) Observed signs of neurological or neuropsychological dysfunction, headache, dizziness, irritability, fatigue or poor concentration.”
18 According to the CDC (based on the 1991 National Health Interview Survey), the incidence of athletic TBIs was approximately 300,000, with only 12% of those injuries requiring hospitalization.
19 The remaining 88% most likely include many MTBIs based on currently accepted definitions.
19 It is important to note that this survey included weighted data collected from 46,761 households where the main outcome measure was the occurrence of one or more incidences of head injury with loss of consciousness. As many concussions in athletics do not result in loss of consciousness, actual occurrence of MTBIs in the athletic arena is likely much higher. A survey of high school football players found that only 47.3% of the athletes who sustained a concussion had reported it at the time of injury.
20 The most common reason for not reporting was belief that the injury was not serious enough to need medical attention (66.4%). Other cited reasons include not wanting to leave the game (41%), not recognizing that a concussion had occurred (36.3%), and not wanting to disappoint their teammates (22.1%).
The large numbers of athletic-related MTBIs raise concerns about possible short and long term sequelae of repetitive injury.
9 Dementia Pugilistica in boxers results from repetitive head injury and leads to chronic disability.
5,21 Second Impact Syndrome (SIS)is rare and potentially fatal. SIS occurs when “…an athlete who has sustained an initial head injury, most often a concussion, sustains a second head injury before symptoms associated with the first have fully cleared.”
22,23 SIS may result from increased vascular congestion creating cerebral swelling resulting in transtentorial herniation and subsequent death. There were 35 probable cases of SIS in football between 1980-1993.
5 There are reports of possible SIS in other sports including field hockey and skiing. The existence of SIS is controversial as not all cases fully satisfy diagnostic criteria.
22Post concussive symptoms can also contribute to performance limitations and overall decreased functionality. Athletes who do not exhibit on field mental status changes or report any post concussive symptoms may still be impaired on neuropsychological testing.
24 A National Collegiate Athletic Association (NCAA) Concussion Study found that college football players with a history of concussion are likely to have future concussive injuries with a seven to ten day window of increased susceptibility. Repetitive concussions may be associated with slower recovery of neurological function.
9 Another study found a prolonged course of recovery in high school as compared to college athletes. Significant memory impairment was present up to 7 days after injury in high school athletes but for only 1 day in college athletes.
25,26 Thus, the age of the athlete must be considered when addressing MTBI management.
Concussion is characterized by a disturbance in neural function that can be profound, causing brief loss of consciousness. Early studies utilizing animal models of concussion indicated that loss of consciousness occurred when the head was unrestrained and hit by an angular acceleration/deceleration process.
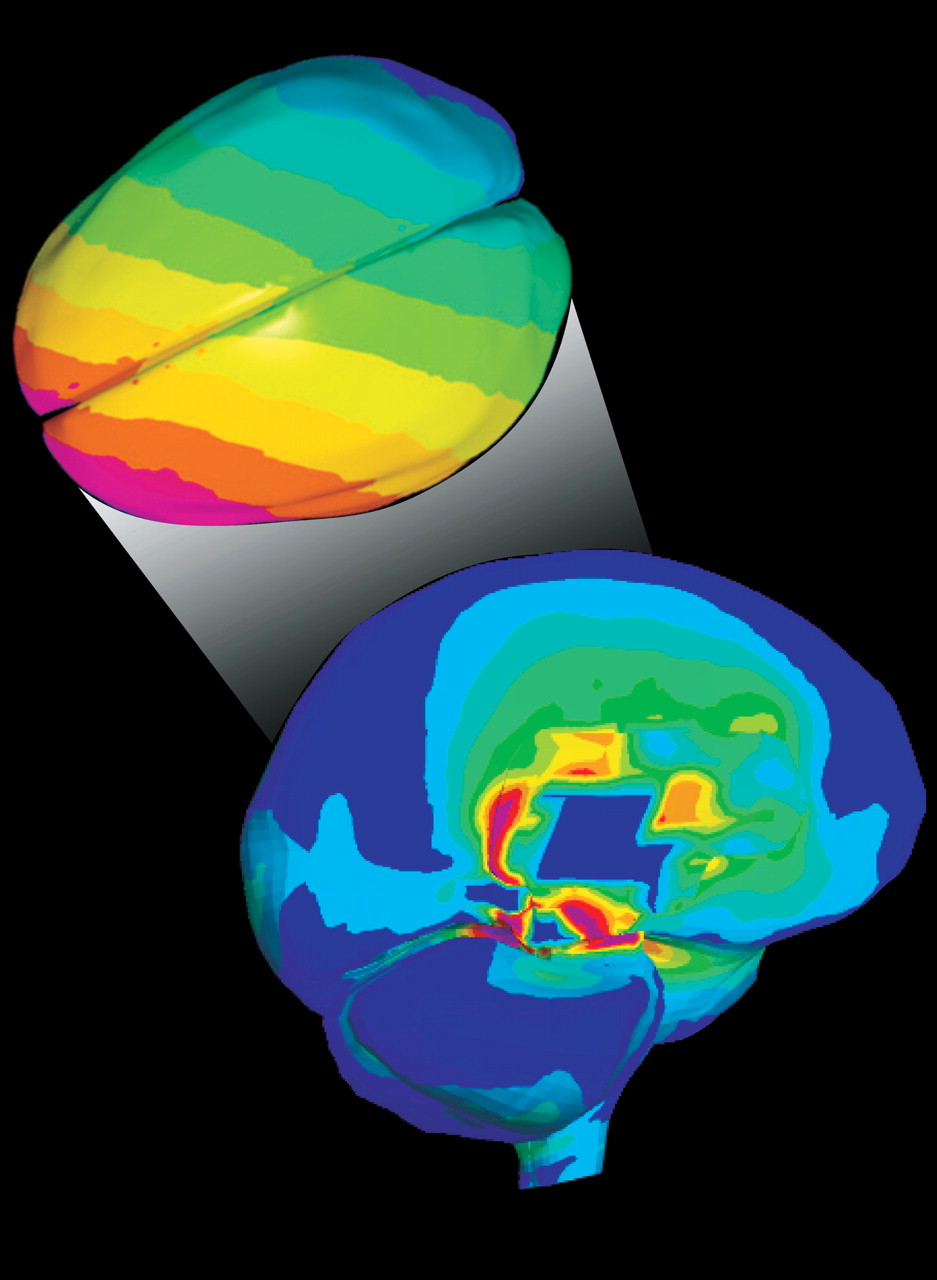
27 Recently, finite element (FE) modeling based on professional football head-to-head field collisions has found that rotational acceleration produced maximum shear stress (
Cover and
Figure 1).
28 No significant relationship was found between translational acceleration and sheer stress. This theoretical analysis is supported by multiple sports studies. A six year investigation of National Football League players demonstrated that the most susceptible to concussion were quarterbacks, wide receivers and defensive secondaries who received a facemask impact at an oblique angle.
29 Concussion in hockey is commonly associated with an eccentric blow to the head, a strike to the face or jaw, or a hit directed to the chin.
30 In taekwondo, concussion is primarily due to a round-house kick (i.e. angular kick) to the temporal region of the head.
31 Additional proposed biomechanical mechanisms of injury include: sudden movement of the head about the axis of the neck severely stressing the craniospinal junction; hemisphere movement causing stretch of brainstem neurons; rotational loading causing violent impact between the skull and brain; propagation of intracranial pressure waves deforming brain tissue and depressing skull bone.
32Several theories of concussion have been developed to explain the immediate loss of consciousness.
27 Reticular theory is based on the premise that a concussive blow temporarily paralyzes the brainstem reticular formation. Centripetal hypothesis attributes concussion to mechanically induced strains disrupting brain function. Activation of cholinergic neurons resulting in suppression of behavioral responses is central to pontine cholinergic system theory. Convulsive hypothesis attributes concussion to generalized neuronal firing. This theory is supported by the sequence of cerebral hyperexcitability followed by a longer period of depression acutely after head injury.
32–34A neurochemical cascade develops immediately following biomechanical insult to the brain, bringing a multitude of cellular changes.
32 Disruption of neuronal membranes and axonal stretching leads to an increase in extracellular potassium and subsequent depolarization and release of excitatory neurotransmitters. This has been termed “neurotransmitter storm.” Thereafter, neuronal suppression occurs diffusely throughout the brain, activating membrane pumps and increasing glucose utilization. Increased lactate production follows. The resultant accumulation may leave neurons more susceptible to further injury.
32 Cerebral blood flow also decreases. N-methyl-D-asparate (NMDA) receptors are activated. There is an influx of calcium into the cell with accumulation in the mitochondria. This impairs oxidative metabolism, leading to energy failure and the possibility of microtubule breakdown. Other neurochemical changes may include: a decrease in gamma-aminobutyric acid (GABA) and other inhibitory neurotransmitters, possibly lowering the seizure threshold; decreased magnesium leading to impaired energy production and neurologic deficits; and loss of forebrain cholinergic neurons resulting in impaired neurotransmission with possible learning and memory difficulties.
32Neuropsychological Testing
Neuropsychological testing is increasingly used in initial assessment of concussion, both on and off the field. In the late 1980’s, The University of Virginia completed the first large scale research study on MTBI in athletes.
35 Neuropsychological testing was utilized to assess cognitive function prior to and following concussion. The Pittsburg Steelers began using neuropsychological testing in the 1990’s to determine return to play decisions. It is now used in other areas of professional athletics, including ice hockey and auto racing.
36 Neuropsychological batteries are also utilized for assessment of short and long term post concussive symptoms. Several return to play guidelines have been developed, based on the degree of symptomatology experienced by the athlete. These guidelines have slight differences in their definitions of grades of concussion and recommendations. At present, all are based on expert opinion rather than prospective studies.
15,37–39 Ideally, baseline testing is obtained at the beginning of the season. At the time of injury, testing is repeated. The choice of specific neuropsychological tests varies, but a battery is chosen to assess cognitive skills including immediate and delayed recall, orientation, verbal memory, attention span, word fluency, visual scanning and coordination.
36 Methods of testing range from sideline assessment to computer based inventories (e.g. Immediate Post Concussion Assessment and Cognitive Testing (ImPACT)).
40Imaging
Imaging of diffuse axonal injury was recently reviewed.
41 In brief, computed tomography (CT) is the initial method of choice to evaluate and exclude hemorrhage. T2 weighted magnetic resonance imaging (MRI), particularly fluid attenuated inversion recovery (FLAIR) MRI, is more sensitive to traumatic lesions.
42,43 Gradient echo MRI is better at detecting hemorrhagic change. However, studies have not been able to correlate abnormal findings on MRI with either post concussive symptoms or long term outcome.
42 Diffusion weighted imaging (DWI) has been shown to identify shearing injuries not evident on T2/FLAIR or gradient echo sequences, thus making it valuable in evaluating closed head injuries.
44 Diffusion tensor imaging (DTI) examines the integrity of the white matter tracts by measuring the degree and direction of water diffusion, providing a potential marker for white matter injury.
45,46Studies utilizing positron emission tomography (PET) and single-photon emission computed tomography (SPECT) have demonstrated frontal and/or temporal hypometabolism following MTBI at rest and during working memory tasks.
47,48 This has been hypothesized to correlate with decreased memory function. Several recent studies have assessed the potential of functional MRI (fMRI) to provide more thorough assessment following concussion. fMRI provides information regarding neural function during task performance and is noninvasive.
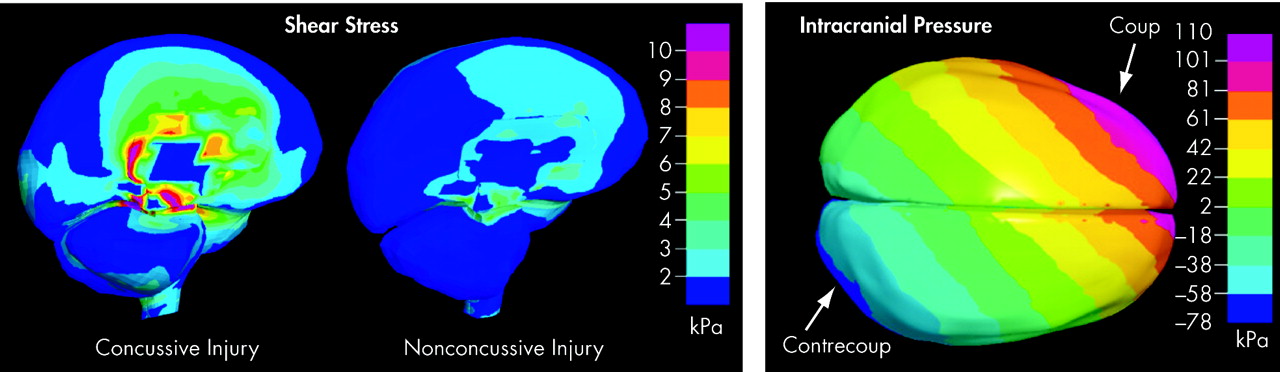
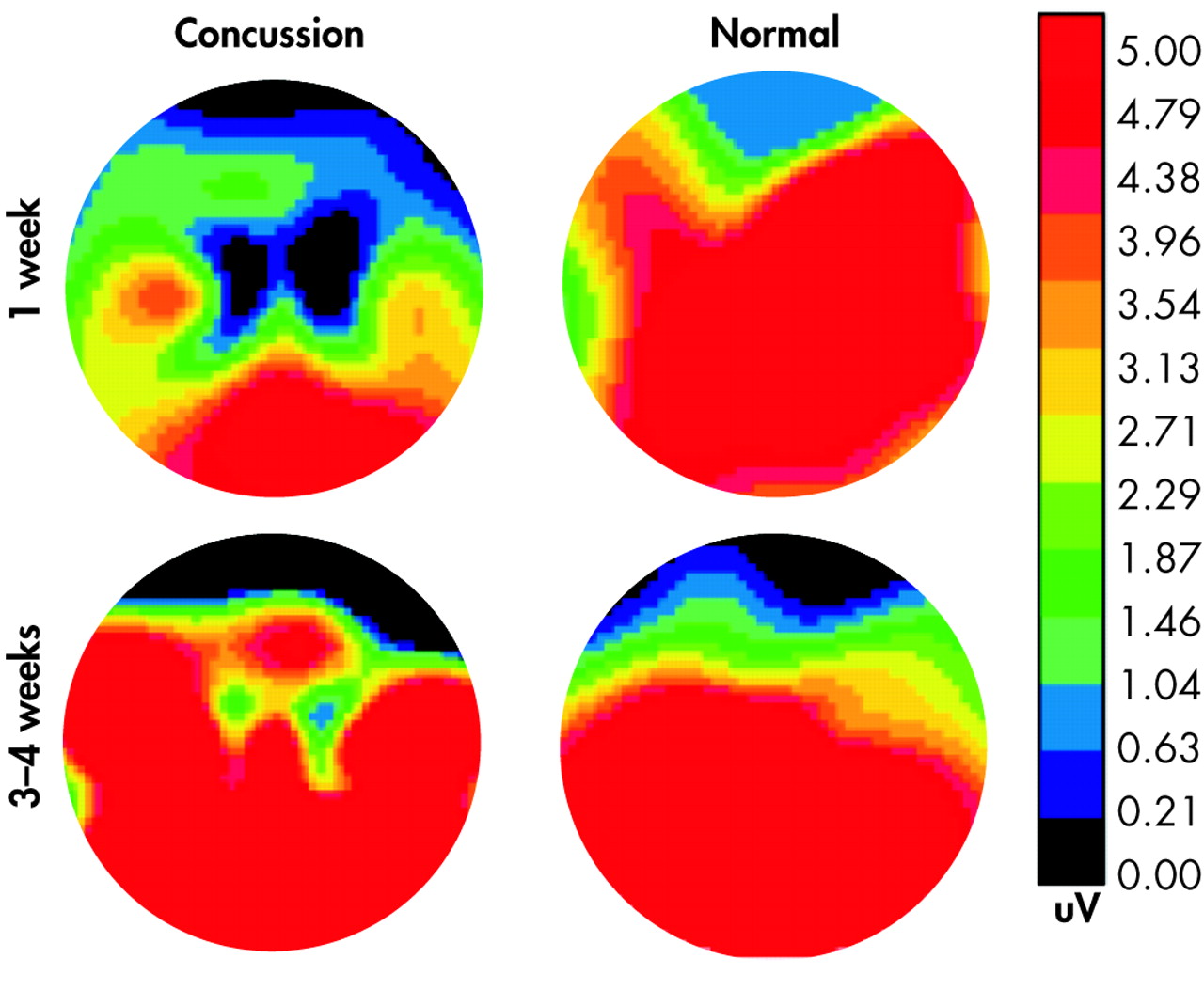
1–3 Tasks can be tailored to obtain information regarding specific neurological functions. A small prospective study of college football players compared individual brain activation patterns prior to and following concussive injury.
1 Brain activation was more widespread following concussion compared to both pre-injury levels and uninjured subjects during the performance of various memory and sensorimotor tasks (
Figure 2). Performance was unchanged compared to baseline measures. The motor sequencing tasks were the most sensitive to concussion. The authors note that these results are consistent with cognitive-load induced recruitment of neural resources. Another fMRI study evaluated working memory in adult athletes who had sustained a concussion (1-14 months prior to study) and were experiencing post concussive symptoms.
2 Athletes with concussions had less task-related activation in the mid-dorsolateral prefrontal cortex (important for working memory) than comparison subjects (
Figure 2). There was an inverse correlation between right dorsolateral prefrontal cortex activation and severity of symptoms. None of the symptomatic athletes had evidence of axonal injury on structural MRI. Thus, functional impairment may be present in the absence of abnormalities on clinical imaging. In addition, concussed athletes had widespread activations in areas not activated in comparison subjects. In one subject, a follow-up study showed that resolution of symptoms was accompanied by normalization of the activation pattern. Finally, less than normal activation was found in dorsolateral prefrontal cortex in a task requiring response inhibition (
Figure 2).
3 These studies provide the framework for the possible clinical utility of fMRI in concussive injury in athletes.
Standard electroencephalographic (EEG) techniques have had limited value in the assessment of MTBI.
49,50 One study utilized EEG patterns in isolation and during postural tasks in comparison subjects versus asymptomatic athletes post-injury (mean of 89.4 days) to evaluate any residual effects of concussion on global cortical function.
51 The authors reported an overall decrease in EEG power in all bandwidths studied, an effect most prominent during standing postures. This suggests a possible explanation for the reduced functional capabilities, such as postural instability, observed in athletes subsequent to concussive injury.
52,53Studies utilizing Evoked Potentials (EP) and Event-Related Potentials (ERP) in the evaluation of MTBI have shown more promising results. Both EP and ERP represent the averaged EEG signal in response to a given stimulus. EPs are thought to represent processing in the primary sensory pathways, whereas ERPs are associated with cognitive processes. EP studies have consistently found the cortical waveform to be briefly extinguished immediately after concussion in animal models.
54 The brainstem auditory evoked potential (BAEP) has been primarily utilized as it is a marker of brainstem function. There have been reports of change in BAEP latency subsequent to concussion, as well as studies that report no change.
50,54 Thus, to date, results are mixed.
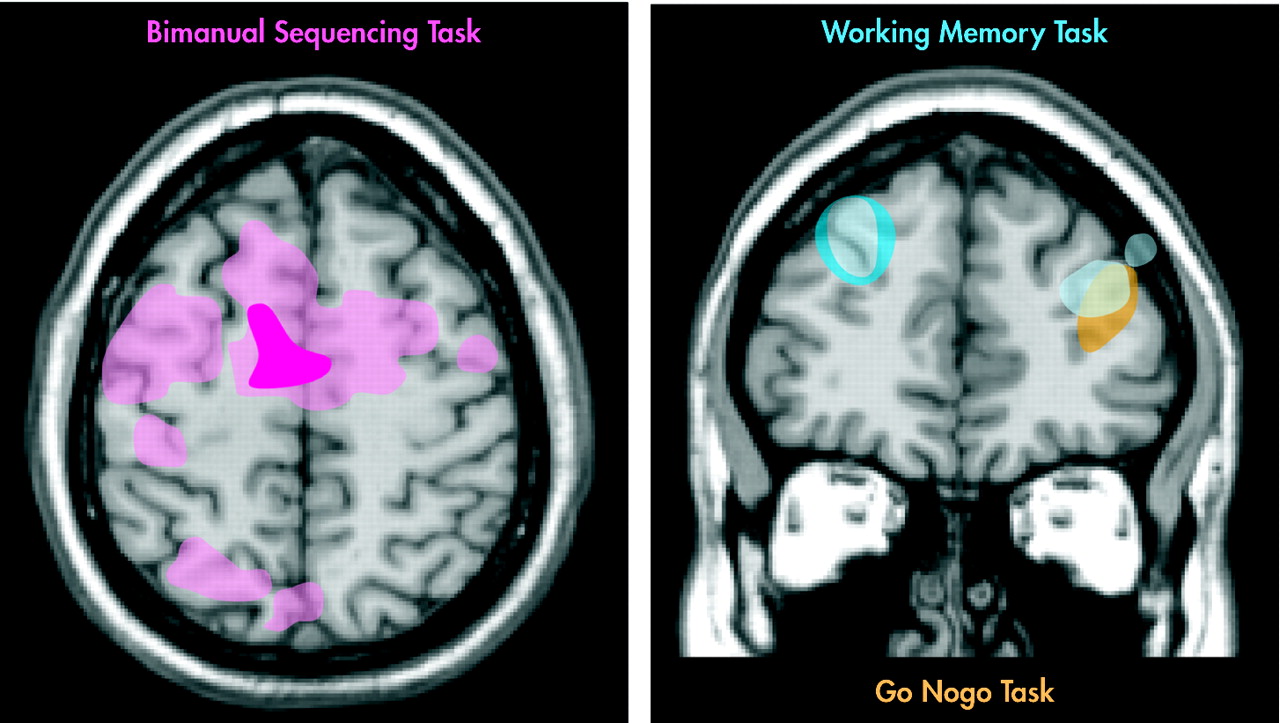
ERP’s may be more useful. One study examined ERPs evoked following MTBI in college athletes.
4 Concussed athletes demonstrated a significant decrease in the waveform around 300msec (P300) which was related to the severity of post-concussive symptoms (
Figure 3). Another study compared the effects of concussion on attention and ERPs in athletes based on their symptomatology.
55 Longer reaction times were exhibited by symptomatic athletes compared to asymptomatic ones. In addition, there was an inverse relationship between severity of postconcussion symptoms and P300 amplitude. This effect was not influenced by the length of time since injury. This suggests that concussive symptomatology affects attentional capacities. As ERPs are resistant to practice effects, this approach is promising as a possible diagnostic tool in MTBI.
A relatively new approach to evaluation of MTBI is Magnetic Source Imaging (MSI). MSI integrates anatomic data from MRI with electrophysiology data from Magnetoencephalography (MEG).
56 MEG measures the neuromagnetic field of the dendrites organized parallel to the skull surface (as compared to EEG that measures the potential gradients of dendrites perpendicular to the skull surface). It allows tracking of real-time brain activity without distortions by differences in conductivity between the brain, skull and scalp.
57 One study compared MRI and resting EEG with resting MSI in post concussive subjects versus comparison subjects.
56 Results indicated that MSI detected more patients with post concussive symptoms than either EEG or MRI alone. All patients with abnormal EEG or MRI also had abnormal MSI. To date, there are no published studies evaluating MTBI with MSI in athletes.