V isual hallucinations are common symptoms associated with significant morbidity in Parkinson's disease.
1 Often, they are assumed to be symptomatic of treatment with dopaminergic medications; however, it is known that hallucinations predate and occur off such medication, suggesting predisposing factors,
1 –
3 such as lower cognitive scores and disease severity.
3 In fact, studies have not found a relationship between antiparkinson medication dose or duration and visual hallucinations in Parkinson's disease.
3,
4 In addition, a growing body of research has suggested an association between the visual system and visual hallucinations. Visual hallucinations in Parkinson's disease are associated with lower visual acuity
3 and visual deficits of color discrimination and contrast sensitivity.
5 Retinal dopamine is deficient in Parkinson's disease and has been linked to abnormal visual processing.
6 Similarly, visual hallucinations have been associated with a visual system dysfunction in Alzheimer's disease and ophthalmologic disorders.
3 In addition to retinal dysfunction, there is evidence for visual cortical dysfunction in Parkinson's disease. A positron emission tomography (PET) imaging study revealed significant metabolic deficits in the visual association cortex and primary visual cortex in Parkinson's disease.
7 To our knowledge, no one has examined whether visual hallucinations are associated with visual cortex abnormality in Parkinson's disease.
In this preliminary study, Parkinson's disease patients with and without visual hallucinations were compared by functional magnetic resonance imaging (fMRI) during visual tasks to examine visual system function.
METHOD
Using international research criteria,
8 neurologists specializing in movement disorders diagnosed and assessed six right-handed patients with strictly defined idiopathic Parkinson's disease. None of them had prior psychiatric illness, but three had visual hallucinations, as defined in prior studies,
3,
7 and three had no visual hallucinations. Hallucinations had to occur at least weekly and be “complex formed” hallucinations, not flashes of light or simple geometric shapes. Hallucinations believed to have other causes, such as delirium and other psychiatric disorders, were excluded. Patients were matched according to gender (all male), age (within 3 years), visual acuity (20/20 [SD=10]), neurological disease severity as measured by the Unified Parkinson's Disease Rating Scale (UPDRS) (10-point range),
9 depression score as measured by the Geriatric Depression Scale (GDS) (3-point range),
10 and cognition using the Telephone Interview for Cognitive Status (TICS).
11 The GDS is a 30-question scale, validated in elderly and medically ill patients, where a score of 11 or above indicates possible depression. Cognition was tested using the TICS
3,
11 because it does not depend on motor or visual capability, both of which were hypothesized as being compromised in Parkinson's disease. The TICS correlates highly with the Folstein Mini-Mental State Examination (MMSE), and is scored from 0 to 41, with scores of 29 or less indicating dementia.
For hallucinators, mean age was 69.7 years (SD=8.7, range=60–77); visual acuity of “best eye:” 20/26.7 (SD=5.8, range=20/20–30); UPDRS: 35.0 (SD=2.6, range=24–53); cognitive score (TICS): 31.7 (SD=2.1, range=27–34); and GDS: 11.0 (SD=2.6, range=4–14). Nonhallucinators' mean age was 66.0 years (SD=2.7, range=63–74) (p=0.53); visual acuity 20/ 23.3 (SD=5.7), range=20/20–30 (p=0.52); UPDRS 32.6 (SD=3.5), range=29–42 (p=0.41); TICS 34.3 (SD=2.1), range=30–37 (p=0.19); and GDS of 6.0 (SD=4.6), range=2–11 (p=0.20). After complete description of the study to the subjects, written informed consent was obtained.
The six subjects underwent a visual task designed to activate primary visual and visual association cortex. Visual stimuli were presented using video goggles. Subjects attended to colored geometric shapes moving in random directions across a black background (activated state) alternating with a white stationary crosshair on a black background (baseline state), each in seven 21-second blocks. Images were acquired on a 1.5T Siemens scanner. A three-dimensional high-resolution T1 weighted image was acquired to aid in anatomical localization and was partitioned into 100 contiguous 1.5 mm thick sagittal 256 x 256 voxel slices with an inplane voxel size of 1mm × 1mm. Functional sequences consisted of a series of 84 sets of 25 to 27 contiguous axial slices, of a gradient echo-planar sequence (TR=3.05 seconds, TE=48 msec, FOV=335 mm, flip angle=90, readout bandwidth =2080Hz/pixel). The images were reconstructed into 128 x 128 voxel matrix with an inplane voxel size of 2.62 mm x 2.62 mm.
We performed an image analysis with the AFNI software.
12 The images were motion corrected and normalized to stereotaxic coordinates. Significantly activated function sites were determined using the correlation method described by Bandettini.
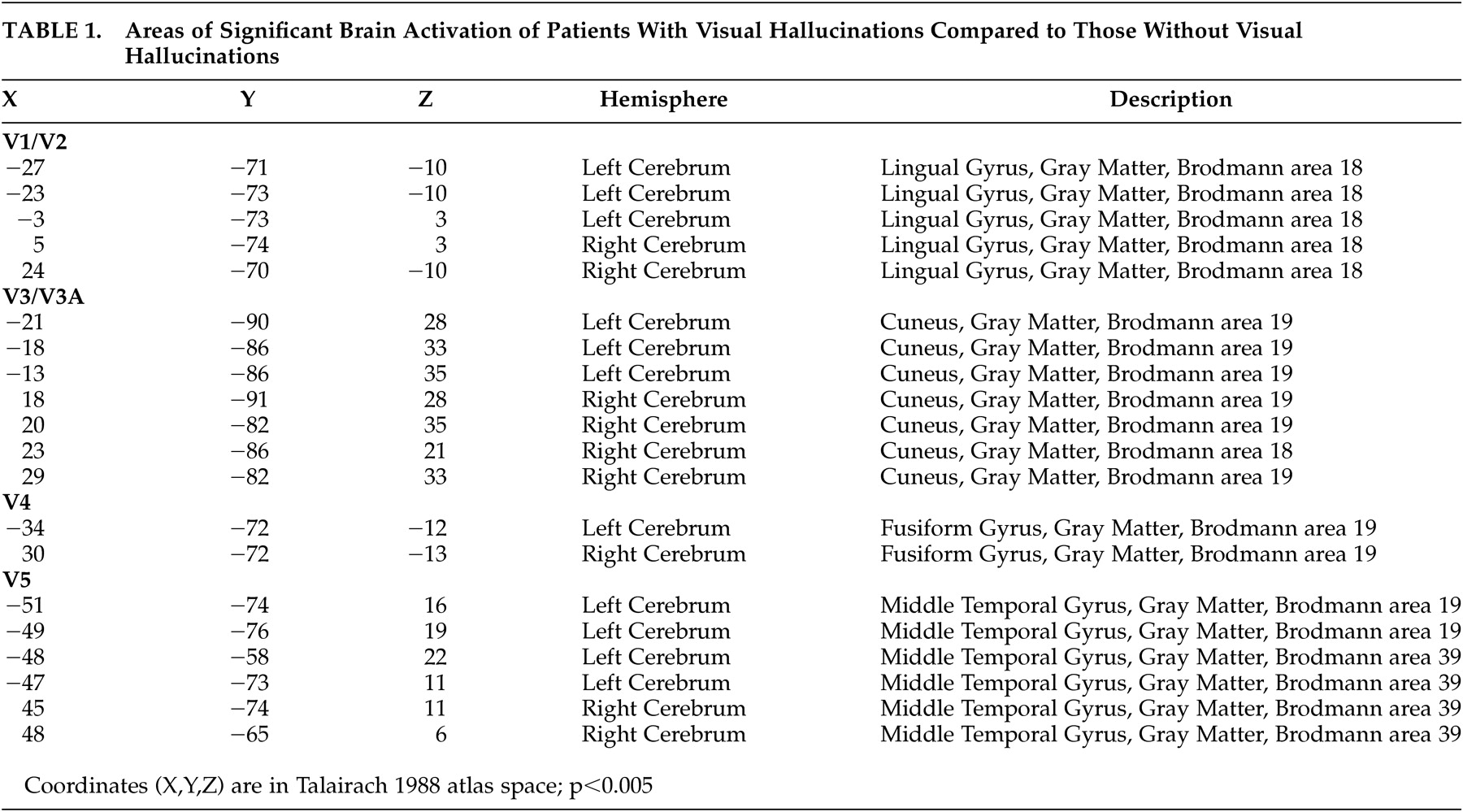
13 The groups were compared using analysis of variance (ANOVA). The resulting statistical map showed the Brodmann areas with significantly different activations between groups.
DISCUSSION
This preliminary study offers fMRI evidence that visual system function differs in Parkinson's disease patients who have visual hallucinations and Parkinson's disease patients who do not. The visual tasks revealed different patterns of activation of visual cortex between the groups. It is interesting that visual association cortex was significantly activated in hallucinators. The visual association cortex has been postulated to be involved in visual hallucinations in Alzheimer's disease, cortical infarctions, and epilepsy, and electrical stimulation of the visual association cortex (Brodmann area 19) causes complex visual hallucinations.
14 The mechanism of the cortical abnormality in Parkinson's disease is unknown, but it has been postulated that retinal/afferent abnormalities may alter the function of the visual cortex.
6,
15 It is possible that retinal dopamine deficiency causes reduced signals to the primary visual cortex, consistent with the reduced activation of the primary visual cortex in hallucinators in our study. This reduced activity of the primary visual cortex may, in turn, induce “release hallucinations” from the visual association cortex—visual memories that normally are suppressed when visual input is sufficient.
5,
15 Thus, the visual association cortex would demonstrate increased activity due to insufficient suppression from the retina and primary visual cortex, consistent with the activation pattern in this study.
This study is the first to suggest an association between the abnormality of the visual cortex, retinal function, and visual hallucinations in Parkinson's disease. It is limited by the small sample size and thus offers only preliminary evidence. However, the study is strengthened by the strict criteria used to define and match the subjects. Further study is needed to investigate the relation between the visual system and visual hallucinations in Parkinson's disease, which may increase knowledge regarding the neural mechanisms of visual hallucinations in Parkinson's disease and other disorders.