A lthough long-term follow-up studies indicate that obsessive-compulsive disorder (OCD) is often a chronic condition with a fluctuating course, very little research has been devoted to the highly disabled subgroup of OCD patients who appear to be treatment refractory. Even though there is no formal consensus on what constitutes a valid operational definition for the term “treatment refractory,”
1 approximately 10%–30% of patients with OCD fail to respond to standard psychopharmacologic and cognitive behavior interventions.
2 –
4 Skoog and Skoog
4 conducted the longest prospective study on OCD, a 40-year follow-up of 144 patients with OCD from approximately 1950 until 1990. This naturalistic study showed that among a large group of patients, most of whom had not received any treatment for OCD, a majority (83%, n=120) were clinically improved at follow-up; one-fifth had full remission and two-thirds continued with subclinical or clinical symptoms. A study by Jenike et al.
5 that followed patients with “refractory” OCD reported on 33 patients who had received cingulotomies for OCD over a 25-year period. At follow-up, approximately 30% of the patients appeared to have benefited substantially from the procedure. However, this study was limited in that it was retrospective regarding the selection of subjects, and that the majority of patients did not receive preoperative treatment that today would be considered optimal therapy for OCD. In contrast, there are two studies that prospectively examined the long-term outcome associated with cingulotomy in patients with treatment refractory OCD. In one study examining 44 treatment refractory patients with OCD who underwent one or more cingulotomies, at mean follow-up of 32 months, 14 patients met criteria for treatment response (32%) and six were partial responders (14%).
6 In the other study, 17 patients with refractory OCD treated with bilateral anterior cingulotomy were followed for up to 24 months postsurgery. The overall mean improvement in the Yale-Brown Obsessive Compulsive Scale (Y-BOCS) score relative to presurgical baseline was 48%, and 8 of the patients met criteria for treatment response (47%).
7As an alternative to neurosurgery, investigators have explored other treatment options for treatment refractory patients, such as intravenous clomipramine. In a placebo-controlled study, Fallon et al.
8 demonstrated that intravenous clomipramine was superior to intravenous placebo for 54 patients who were previously refractory to oral clomipramine.
To examine the long-term outcome of patients identified as having treatment refractory OCD, a follow-up study of patients treated with intravenous clomipramine at the New York State Psychiatric Institute was conducted. The following questions were addressed: What percentage of patients continued to have diagnosable OCD at follow-up, and what was the range of severity of symptoms? Are any clinical variables associated with long-term outcome?
METHODS
Participants
Between 1988 and 1995, 59 patients with a DSM-III-R diagnosis of OCD and a history of inadequate response to oral clomipramine received 14 infusions of IV clomipramine. Of the 59 patients, 54 had participated in the placebo-controlled study,
8 and five had received IV clomipramine as part of an open-label treatment study. All patients signed informed consents for this follow-up study and for the initial treatment studies that had been approved by the New York State Psychiatric Institute Institutional Review Board.
Participants entering the IV clomipramine treatment studies had to meet the following criteria: 18 to 55 years of age and a poor response to prior treatment with oral clomipramine. Poor response to an adequate treatment trial was defined as no improvement or only a partial improvement, based on patient self-report, or an inability to tolerate oral clomipramine’s side effects. An adequate clomipramine trial was defined as at least 8 weeks in duration with at least 2 weeks at a dosage of 200 mg/day or more. Of the 59 enrolled patients, 98% had additionally failed to benefit from a trial of one selective serotonin reuptake inhibitor (SSRI) and 40% failed to respond to two SSRIs. Of the 54 patients enrolled in the double-blind study, 51 completed the study. Therefore, a total of 56 patients completed the full schedule of 14 intravenous clomipramine infusions, including the five from the open-label trial. Patients randomized to placebo in the treatment study were subsequently treated with open-label intravenous clomipramine with the same schedule of clomipramine as in the double-blind phase. OCD severity assessments on the 56 patients were made before and after the 14 intravenous clomipramine infusions (“immediate post-intravenous clomipramine”). In addition, a sequential subgroup of the 56 patients was reevaluated 1 month after completing the clomipramine infusions (“one-month post-intravenous clomipramine”).
For the current follow-up study, 50 of the 56 participants were contacted; four participants were unable to be located and two were deceased. Of the 50 contacted individuals, six did not want to participate in the follow-up study and the remaining 44 were evaluated with a “brief interview” lasting 30 minutes. Of the 44 participants who agreed to participate in the brief telephone interview, 34 agreed to be assessed with an “extended interview” lasting 3 hours, through mail, telephone, or an in-person meeting.
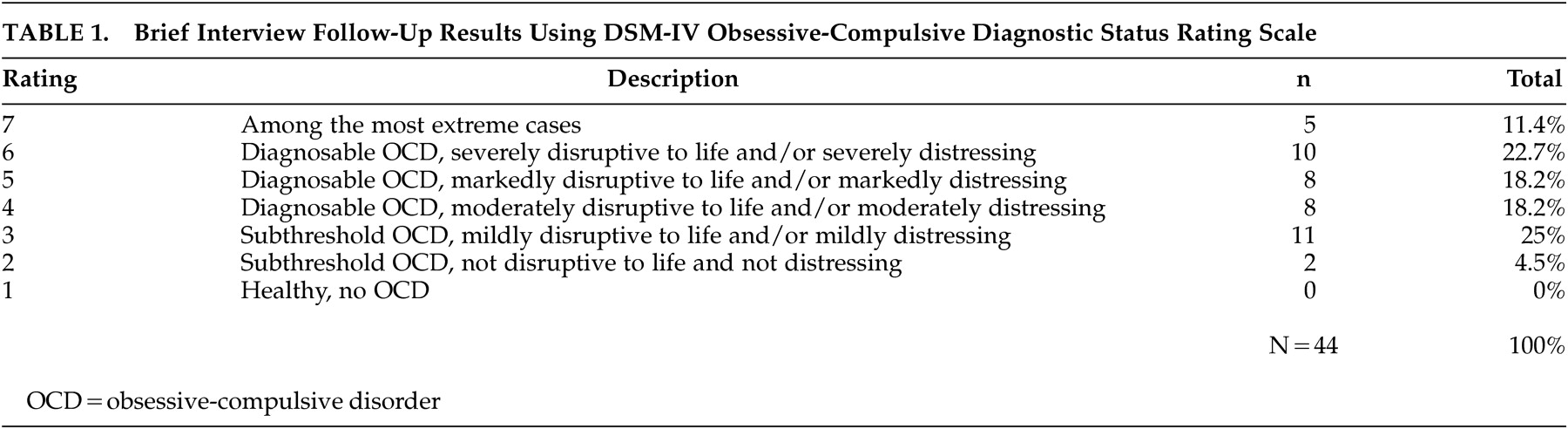
The brief follow-up interview (n=44) assessed severity using the DSM-IV Obsessive-Compulsive Diagnostic Status Rating Scale—a 7-point scale developed with specific clinical anchors to rate patients on OCD severity at healthy (1), subthreshold OCD (2–3), or diagnosable OCD (4–7) (
Table 1 ). A clinician- and patient-rated Clinical Global Impression (CGI) Severity and Improvement Scale
9 measured global severity and improvement in general functioning, compared to pre-intravenous clomipramine levels.
The extended follow-up interview (n=34) assessed severity further using the Y-BOCS,
10 the National Institute of Mental Health Obsessive-Compulsive severity scale (NIMH-OC),
11 and the Symptom Check List interview (SCL-90),
12 as these measures had been administered years earlier during the intravenous clomipramine study. Comorbidity was assessed using the Structured Clinical Interview for DSM-III-R (SCID-I),
13 to evaluate current and lifetime prevalence of axis I disorders, as well as the SCID-II
14 to evaluate current axis II disorders. The Quality of Life Enjoyment and Satisfaction Questionnaire
15 was used to examine functioning in the following domains: home life, work, leisure activities, social activities, feelings, overall functioning, satisfaction with medications, and total life satisfaction. For the extended interview ratings on the Y-BOCS, a score that was at least 25% less than before the clomipramine treatment categorized a patient as “improved.” Finally, data regarding intervening and current biological and psychological treatments were collected at follow-up. Behavioral treatment was subclassified as “intensive” if it lasted for at least 4 months, was completed at least three times per week, and lasted at least 2 hours per session.
Assessment Availability
Pre-intravenous clomipramine treatment and immediate post-intravenous clomipramine ratings (Y-BOCS, NIMH-OC severity scale, and CGI Severity) were available for all follow-up participants. One-month post-intravenous clomipramine ratings using these same s everity assessments were available on 26 of 44 participants who completed the long-term follow-up brief interview and on 22 of the 34 participants who completed the extended interview. All patients in the extended follow-up interview had participated in the brief interview as well.
Statistical Methods
To address the first question regarding the percentage of patients who continued to have diagnosable OCD and the range of severity of symptoms, we used the DSM-IV Obsessive-Compulsive Diagnostic Status Rating Scale (
Table 1 ).
To assess whether any clinical measurements collected at follow-up were associated with long-term outcome, data from the extended interview were used. Patients were compared on various dimensions based on whether they fell into the “improved group” or the “unimproved group” as measured by the Y-BOCS. Specifically, the comparisons were made on measures of psychopathology (OCD severity based on the Y-BOCS, NIMH-OC scale, Symptom Check List interview, and CGI Severity) and functional status (Quality of Life Enjoyment and Satisfaction Questionnaire) using two sample’s t test. Using a Bonferroni adjustment for multiple comparisons, statistically significant results were those with p values <0.002. Also, we examined the association between current clinical status (improved or unimproved) and comorbid axis I and axis II diagnoses at follow-up using chi-square tests.
To assess the predictive power of various pre-intravenous clomipramine and post-intravenous clomipramine intercurrent measures on current changes in OCD severity, we used regression analyses. We used multiple linear regression with the DSM-IV Obsessive-Compulsive Diagnostic Status Rating Scale, change in Y-BOCS (pretreatment to follow-up), change in NIMH-OC (pretreatment to follow-up), and change in CGI Severity (pretreatment to follow-up) as outcomes measuring current improvement in OCD. Variables chosen as predictors of outcome included age of onset of illness, duration of illness pre-intravenous clomipramine treatment, pretreatment Y-BOCS/NIMH-OC/clinician-rated CGI Severity scores, and response status immediately and 1-month posttreatment. To study the effect of pretreatment OCD severity measures on the previously described dichotomous Y-BOCS measure (improved or unimproved), we used logistic regression analysis.
RESULTS
Characteristics of the Sample at Follow-Up
The range of the follow-up period was 4 to 11 years. Of the 56 patients sought for follow-up, we obtained information for 46 patients (82%). Two patients had committed suicide, of whom one had a history of severe childhood trauma (and a poor response to cingulotomy after a poor response to intravenous clomipramine) and another had comorbid bipolar disorder.
Of the 44 patients who completed the brief interview, the mean age was 41.2 years (SD=10), with a range of 27 to 62. There were 23 men and 21 women. Eight were working full-time (18.2%), nine were working part-time (20.5%), and 27 were either unemployed or on disability (61.4%). Fourteen were living with a significant other (31.2%), 16 were living alone or with a roommate (36.4%), 10 were living with their parents or relatives (22.7%), and four were living in a group home (9.1%).
With respect to current treatment status, 41 patients were being treated with medication with or without some form of psychotherapy (93.2%), zero with psychotherapy alone (0%), and three were not receiving any treatment (6.8%). Of the 41 patients being treated with medication with or without psychotherapy, 26 patients were treated with an SSRI as monotherapy (63.4%), 10 were receiving oral clomipramine as monotherapy (24.4%), and two were treated with a combination of an SSRI and oral clomipramine (4.9%). Moreover, 10 patients were being treated with medication and behavioral therapy (24.4%), seven were being treated with medication and supportive or dynamic psychotherapy (17.1%), and one was treated with dynamic psychotherapy alone (2.4%).
Of the 44 patients interviewed at follow-up, 13 had subthreshold OCD (29.5%) and 31 met full DSM-IV criteria for OCD (70.5%) (see
Table 1 ). Moreover, of the 44 patients, 20 (45.5%) reported an overall subjective clinical improvement based on a score of 1 or 2 (very much improved or much improved) on the patient-rated CGI Improvement Scale, comparing current status to pre-intravenous clomipramine status.
Long-Term Diagnostic Outcome
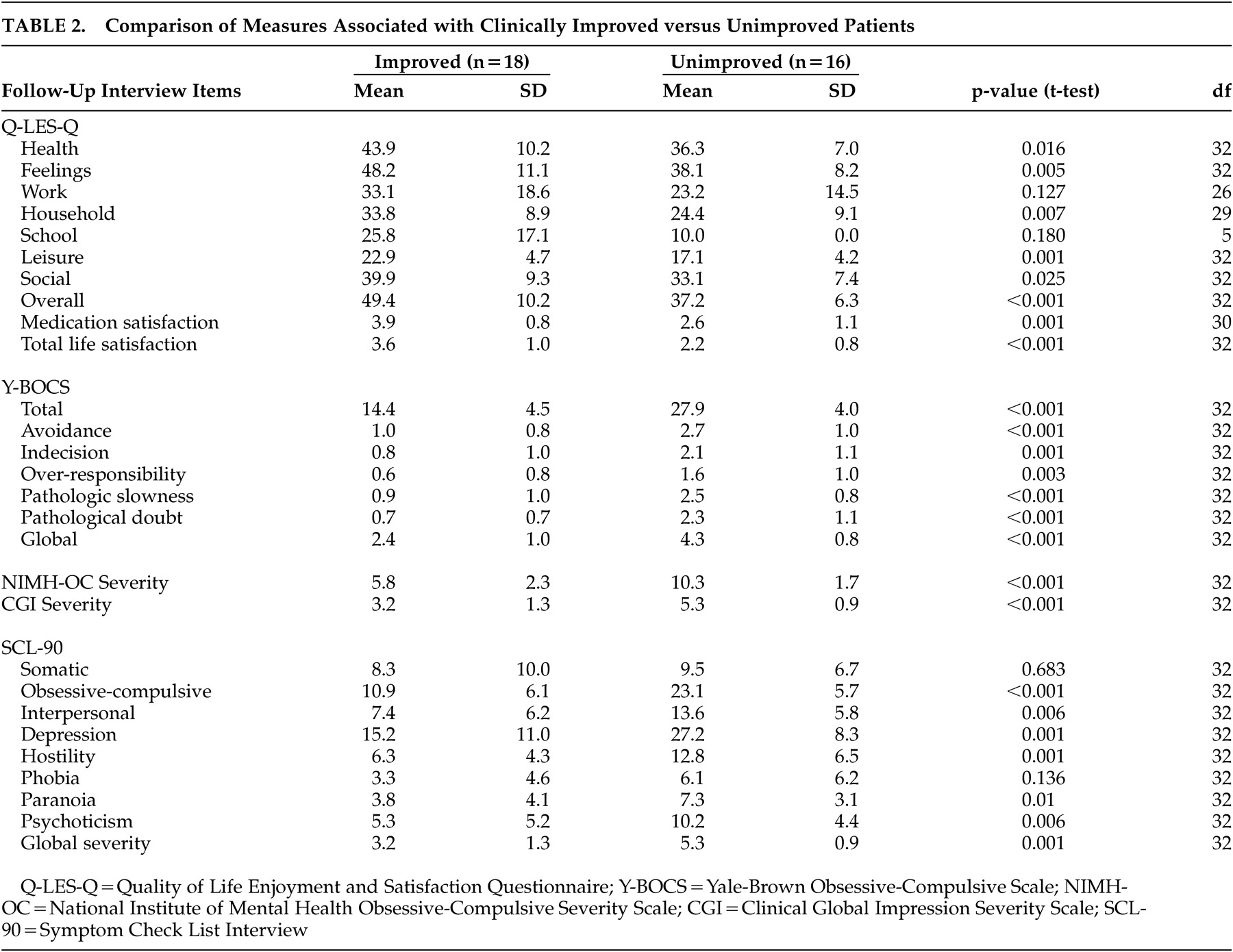
Of the 34 patients who completed the extended interview, 18 were classified as “improved” based on the change in Y-BOCS (53%); the remaining 16 patients were classified as “unimproved” (47%). Comparison between the improved and unimproved groups with respect to various follow-up assessments is given in
Table 2 . As expected, patients who were rated as improved based on the Y-BOCS also had significantly lower scores on NIMH-OC Severity, CGI Severity, and the other Y-BOCS items not included in the 10-item Y-BOCS score (avoidance, indecision, pathological slowness, pathologic doubting, and global severity). In addition to these clinician-rated scores, the clinically improved patients also had an improved functional status and decreased psychopathology on the Symptom Check List interview (SCL-90). These included Quality of Life Enjoyment and Satisfaction Questionnaire domains of leisure activities, overall functioning, medication satisfaction, and total life satisfaction; and the Symptom Check List interview cluster domains of obsessive-compulsive, depression, hostility, and global severity.
When the DSM Obsessive-Compulsive Diagnostic Status Rating Scale at follow-up was regressed on pre-intravenous clomipramine treatment measures and intercurrent measures for 44 patients, the pretreatment NIMH-OC Severity, but not the pretreatment Y-BOCS, was significantly associated with outcome (p=0.004). When change in severity of OCD (Y-BOCS/CGI Severity/NIMH-OC) or categorical Y-BOCS improvement at follow-up was regressed on pretreatment measures and immediate post-intravenous clomipramine Y-BOCS (n=34), no statistically significant associations were found. However, using the smaller data set of 22 patients who had 1-month posttreatment Y-BOCS ratings and who also participated in the extended interview, the one significant predictor variable associated with categorical Y-BOCS improvement at follow-up was the 1 month posttreatment response status, defined as at least 25% improvement from pre-intravenous clomipramine (p=0.039; odds ratio=7.9, 95% confidence interval 1.062, 58.44). In other words, patients who were responders 1-month after intravenous clomipramine treatment had eight times higher odds of doing better at follow-up than patients who were nonresponders 1 month after clomipramine treatment
Prevalence of Comorbid Psychiatric Illness
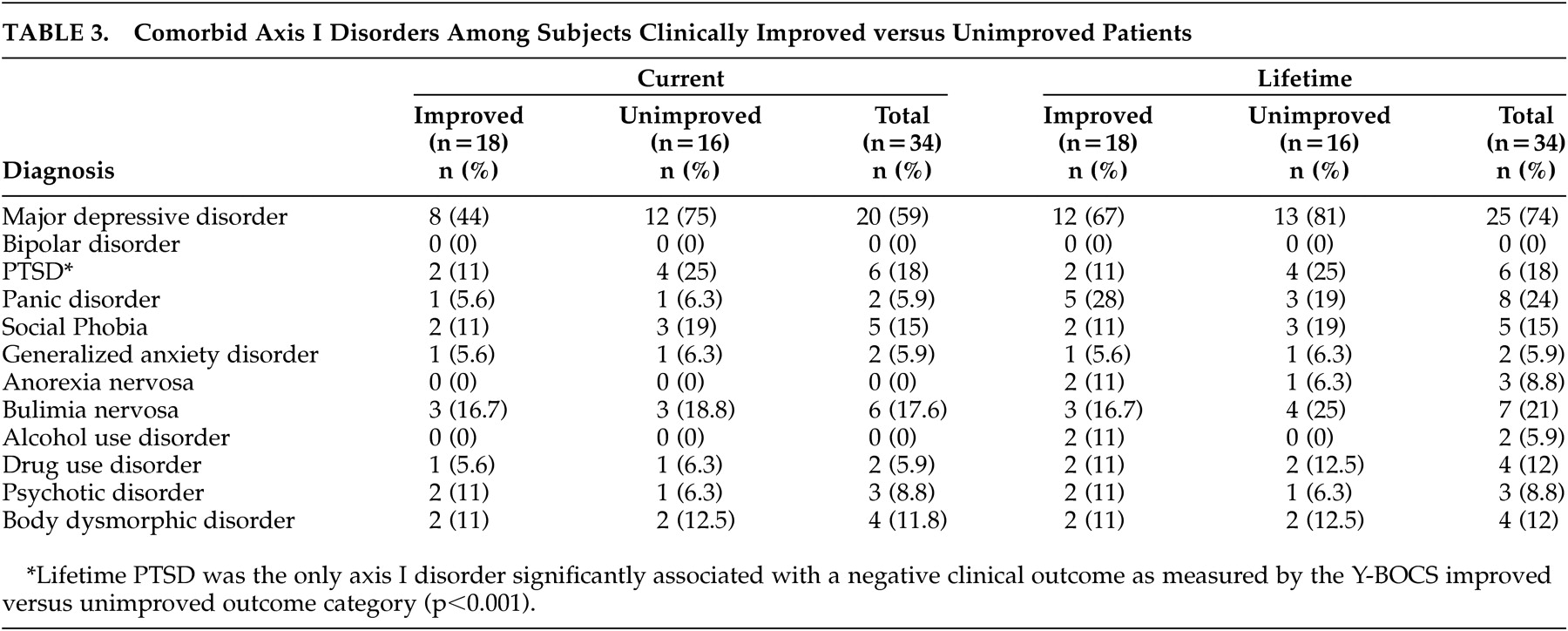
For patients who completed the extended interview (n=34), several axis I disorders were quite prevalent both currently and over the patient’s lifetime (
Table 3 ). Overall, 76% of the patients had a current comorbid axis I diagnosis (n=26) and 82% of them had a lifetime comorbid axis I diagnosis (n=28). Only one diagnosis, lifetime posttraumatic stress disorder (PTSD), was significantly associated with a negative outcome (Y-BOCS improved versus unimproved, p<0.001).
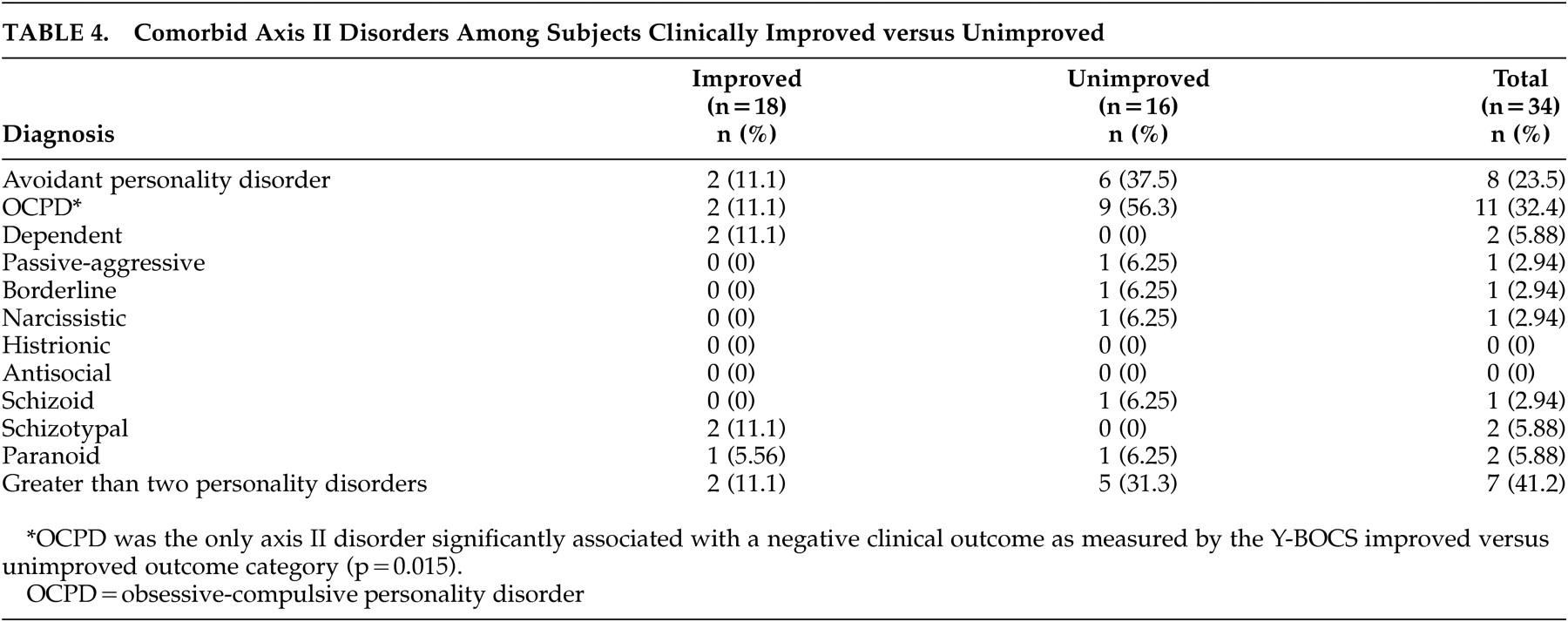
With respect to axis II (
Table 4 ), 20 patients met criteria for at least one personality disorder diagnosis (58.8%). The most common personality disorders were within the cluster C group: 11 with OCPD (32.4%) and eight with avoidant personality disorder (23.5%). Also, 41.2% of all patients with personality disorders (n=14) had at least two personality disorders. Only one diagnosis, OCPD, was significantly associated with a negative clinical outcome as measured by the Y-BOCS improved versus unimproved outcome category (p=0.015).
DISCUSSION
This follow-up study examined a sample of treatment refractory patients with OCD 4 to 11 years after they were treated with intravenous clomipramine. Information on 82% of the targeted sample was obtained, making it likely that the results are representative for the original cohort of patients.
Using the data set from the brief interview on all 44 patients, this study revealed that 46% of these patients reported being subjectively clinically better (n=20) compared to at study entry, and 30% no longer met criteria for OCD (n=13). None, however, reported full remission. Approximately forty percent had some form of employment (n=17), and approximately two-thirds were living independently (n=30). Over 90% continued on medication (n=41), either an SSRI, clomipramine, or a combination of the two. These results suggest that a substantial percentage of the patients with “refractory” OCD improve symptomatically with time. It is unclear whether this was a gradual, sustained improvement or one that fluctuated over time. It is also unclear if the improvement was in fact due to the intravenous clomipramine treatment or due to some other therapeutic intervention over time. The vast majority of patients, however, appeared to need maintenance pharmacotherapy.
Using the greater amount of information available on 34 patients (61% of the targeted sample), this study revealed that 53% of these patients were clinically improved, by objective Y-BOCS measures, at the time of follow-up (n=18). This is consistent with the results of the brief interview with the larger sample of 44 patients, and it is consistent with the published long-term follow-up studies of refractory OCD patients, where approximately one-third to one-half of patients were at least partially improved at follow-up.
8 –
10 Statistical analyses revealed various features associated with clinical improvement. As expected, scores on OCD severity as measured by instruments other than the Y-BOCS (NIMH-OC Scale and the CGI Severity Scale) were substantially lower in the improved compared to the unimproved group. Overall concurrent psychopathology was also noted to be significantly less in the improved group when measured on the continuous scale of the SCL-90 in the domains of obsessive-compulsive, depression, hostility, and global severity. In addition, the improved patients reported greater satisfaction with their quality of life, particularly with regard to leisure activities, medication satisfaction, overall functioning, and total life satisfaction. Therefore, improvement in OCD was accompanied by improvement in several other areas.
The NIMH-OC Severity assessed prior to intravenous clomipramine treatment was related to long-term outcome, with higher pretreatment scores being predictive of a worse outcome as measured by the DSM Obsessive-Compulsive Diagnostic Status Rating Scale. It is unclear why the pretreatment Y-BOCS and CGI Severity were also not associated with the long-term outcome. However, one could speculate that NIMH-OC scale in its blending of functional status with OCD severity measures the broader impact of OCD that might not be detected by the Y-BOCS or CGI measures. Because more symptomatic and functionally impaired patients may be at greater risk for poor long-term outcome, treatment strategies among these patients may be more effective if the functional aspects of life were addressed as well as the OCD psychopathology. The only historical measure that was associated with long-term improvement, as measured by the Y-BOCS, was the dichotomous Y-BOCS improvement 1-month post-intravenous clomipramine treatment. This suggests that the sustained (i.e., 1-month posttreatment) response to intravenous clomipramine may have more long-term prognostic value than the immediate end-of-treatment response. Also, we were unable to identify any intercurrent treatments that were more or less likely to result in improved outcome.
The strengths and limitations of this study should be noted. The strengths include a well-defined population of patients with “refractory” OCD who received standardized reliable assessments 4–11 years earlier, a subgroup of whom also received these identical assessments at follow-up. A limitation includes uncertainty regarding the validity of the Clinical Global Impression assessments during the “brief” interview, because faulty recall and recall bias would certainly have an impact after 4–11 years. Second, because the extended data set was obtained on only 60% of the target sample, it is possible that a “sicker” subgroup of patients was not included in the more extensive analysis; however, we do not believe this is a major concern, as the results from the brief interview were similar to those from the extended interview.
In conclusion, a subsample of patients, considered “treatment refractory,” did show considerable clinical and functional improvement at follow-up. This study therefore suggests that the prognosis for a sizable portion of patients with refractory OCD is promising.
Acknowledgments
FDA Grant #R-000374-01 to Dr. Michael Liebowitz and Dr. Brian Fallon; NIMH Grant #R01 MH55842 to Dr. Brian Fallon and Dr. Michael Liebowitz.