Mild cognitive impairment (MCI) is the intermediate stage between the cognitive changes of normal aging and those of dementia.
1 Various sources can provide a detailed discussion of MCI.
2,3 Subjects with MCI constitute a high-risk group because they develop dementia at a rate of 10% to 15% per year, as compared with 1% to 2% per year in the general population.
4 In view of this, it is critical to identify potential protective factors against MCI. Previous studies have reported an association between cognitive activities and reduced risk of incident dementia.
5–7 However, little is known about the association between cognitive activities and the odds of having MCI. A convenience sample of a prospective cohort study involving community-dwelling elderly participants reported that baseline cognitive activities were associated with decreased risk of amnestic MCI.
8 There is a need to examine this question using a larger sample in a population-based setting.
We examined whether engaging in cognitive activities is associated with MCI in a cross-sectional study derived from an ongoing population-based study of normal cognitive aging and MCI in Olmsted County, MN. Throughout this manuscript, one can interchangeably think of the phrase “cognitive activity” to be equivalent to “mental activity” or “intellectual activity.”
RESULTS
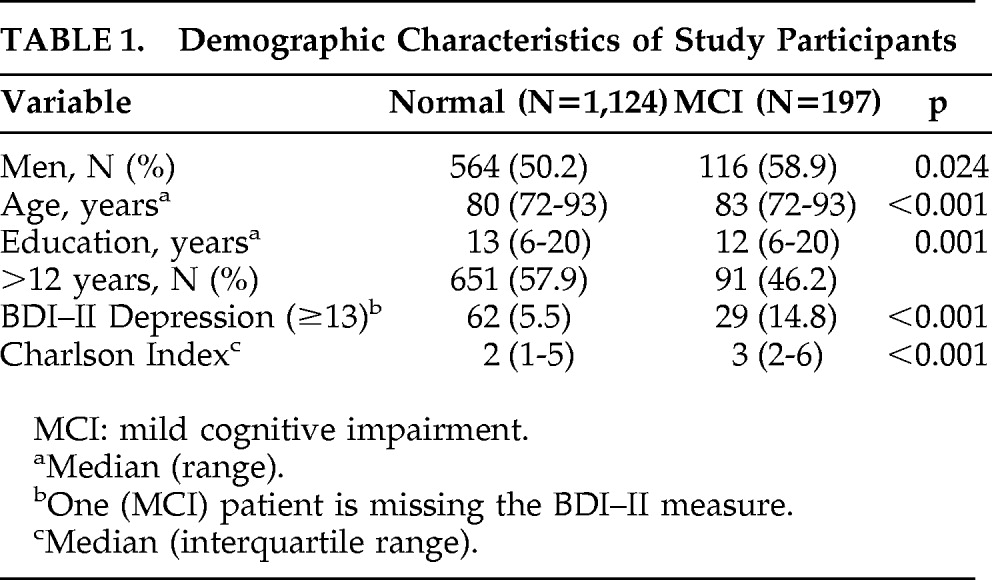
Table 1 summarizes the demographic data. There were 1,321 study participants without dementia (N=1,124 cognitively normal persons, N=197 subjects with MCI). Among the cognitively normal group (Normals), there were an equal number of men and women, whereas, among the MCI group, there were more men than women. On average, the MCI group was older than the Normal group. The two groups also significantly differed in education, medical comorbidity, and depression symptoms. Therefore, in the primary analysis, the comparison of engaging in cognitive activities between the two groups was made after adjusting for age (continuous variable), sex, and education (continuous variable). In a secondary analysis, we also adjusted for depression symptoms, medical comorbidity, and level of physical exercise.
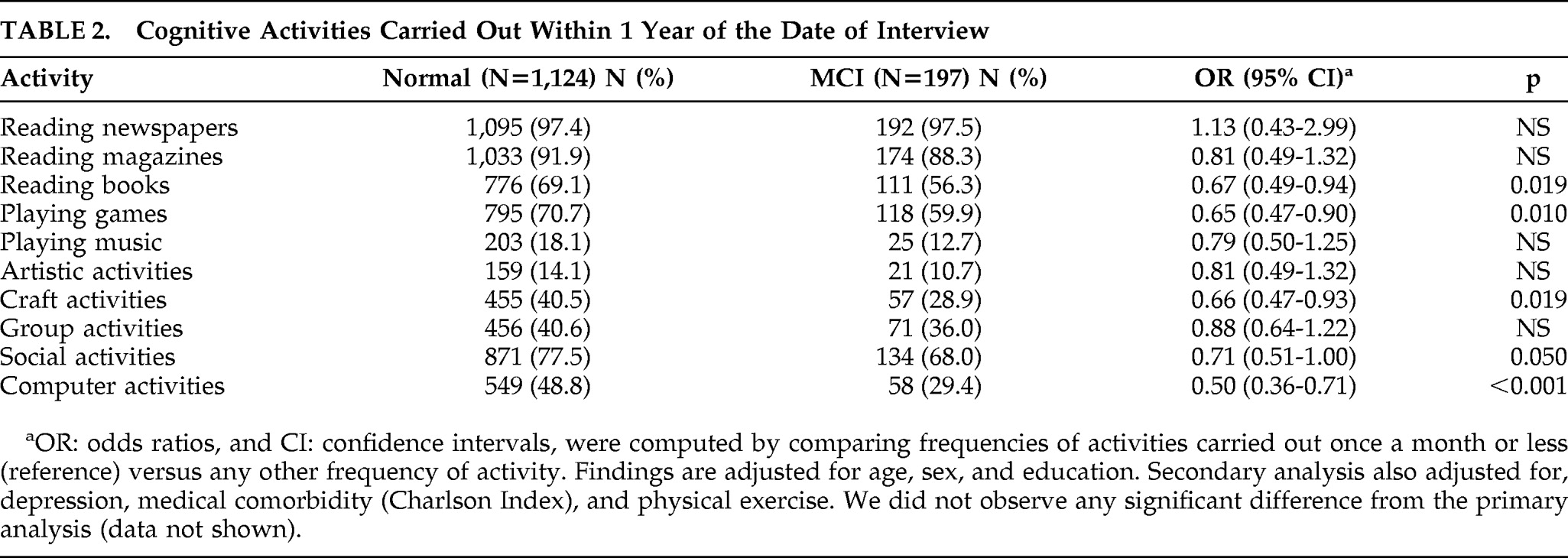
Table 2 displays the data comparing the two groups as measured by OR (95% CI). Reading books (0.67 [0.49–0.94]), playing games (0.65 [0.47–0.90]), craft activities (quilting, pottery, etc.: (0.66 [0.47–0.93]), and computer activities (0.50 [0.36–0.71]) were significantly associated with decreased odds of having MCI. The point estimate for social activity (e.g., going out with friends) was also associated with decreased odds of having MCI, but this association was only marginally significant (0.71 [0.51–1.00]).
The point estimates for reading magazines (0.81 [0.49–1.32]), playing music (0.79 [0.50–1.25]), artistic activities (0.81 [0.49–1.32]), and group activities (0.88 [0.64–1.22]) were associated with reduced odds of MCI; however, none reached statistical significance. The only exception to the overall trend was the cognitive activity of reading newspapers. The OR for reading newspapers (1.13 [0.43–2.99]) suggested increased odds of having MCI; however, close examination of the data indicates that almost identical proportions of the two groups engaged in regular newspaper reading (97.4% of the cognitively normal group versus 97.5% of the MCI group were reading newspapers on a regular basis).
We considered watching TV to be a hypothetically less beneficial activity; therefore watching TV was “reverse”-scored, that is, watching more TV (>6 hours/day) versus watching less (≤6 hours per day). We observed that watching less TV was associated with decreased odds of having MCI (OR [95% CI]=(0.48 [0.27–0.86]; p=0.013].
In the secondary analysis, additional adjustment for depression symptoms, medical comorbidity, and physical exercise did not affect the significance level observed in the primary analysis (data not shown).
DISCUSSION
In this population-based, cross-sectional study, we observed that cognitive activities such as computer use, playing games, reading books, craft activities (quilting, knitting, etc.) and watching less TV were associated with 30% to 50% reduced odds of having MCI. Social activities such as traveling were marginally significant. Even though the point-estimates for reading magazines, playing music, artistic activities, and group activities were associated with reduced odds of having MCI, none reached statistical significance. Almost identical proportions of the two groups were engaged in reading newspapers on a regular basis; therefore we could not observe a significant difference between the two groups.
Several studies have reported the association of cognitive/intellectual or “mental” activities with decreased risk of incident dementia.
5–7 However, little is known about the association of cognitive activities with MCI. The Bronx Aging Study prospectively followed a convenience sample of 437 community-dwelling cognitively normal elderly persons ages 75 and older to the outcome of incident amnestic MCI.
8 During the median follow-up duration of 5.7 years, there were 58 subjects who developed incident amnestic MCI. The investigators noted that a unit-increase in cognitive activity was associated with a 5% decreased risk of incident amnestic MCI. Even though the Bronx study was a convenience sample, the prospective study design would enable one to make some degree of etiologic inferences. The investigators retrofitted the MCI criteria; hence, this might have potentially led to misclassification errors. Although our study is population-based, the cross-sectional design does not allow one to make etiologic inferences. Therefore, the observations made in our current study need to be tested on a larger sample in a prospective cohort design.
The findings of our study should be interpreted within the context of the following limitations: The first limitation pertains to study design. Since this was a cross-sectional study, we cannot determine the direction of causality between the hypothesized exposure of interest (i.e., cognitive activity) and the hypothesized outcome of interest (i.e., MCI). Second, like any survey-based study, recall bias is a potential limitation. This is even more relevant to participants with MCI; however, at our center, the data on cognitive activities are collected before determination of whether a person has MCI. Therefore, neither the participant nor the research personnel knew the case–control status of the participant at the time of administration of the cognitive-activities questionnaire. This likely minimized bias, but could not eliminate it. Also, in the past, we had reported that the test–retest correlations were similar among subjects with normal cognition and MCI.
26Our study did not address mechanism of action. However, the possible beneficial impact of cognitive activities as discussed in the literature is worth mentioning. Engaging in cognitive activities may be a marker for an overall healthy lifestyle; for example, a person who likes to read books on a regular basis may also engage in an overall healthy lifestyle that includes exercise, diet, and stress-management. Another possible explanation is related to the brain/cognitive-reserve hypothesis.
27,28 Engaging in cognitive activity is more likely to reinforce and perhaps stimulate the formation of various neuronal networks in the brain
28 that can buffer against dementia and Alzheimer's disease (AD).
29 This argument is supported by both basic science and clinical research. For instance, animals with enriched environments are protected against cognitive impairment.
28,30 Also, in clinical settings, it is observed that clinical manifestations may not correlate with the neuropathological burden on postmortem examination,
6,31–33 which implies that the cognitive reserve may serve as a buffer against the AD neuropathological burden. Since MCI is considered to be a prodromal state to AD, one can invoke the cognitive-reserve theory to explain the inverse association between cognitive activities and the odds of having MCI. Yet another potential mechanism pertains to the classic stress model proposed by Sapolsky and colleagues.
34 According to this model, the hippocampus, which is the epicenter of the memory network,
35 has a number of glucocorticoid receptors. These receptors are down-regulated in excessively stressful situations. Thus, cognitive activities may serve as stress-modifying agents, leading to decreased “neurotoxic” insult to the hippocampus and related structures pertinent to cognition and emotion.
In summary, our findings contribute to the growing body of literature indicating that cognitive activities are associated with decreased odds of having MCI. A future prospective, population-based cohort study needs to confirm whether cognitive activity is associated with a decreased risk of incident MCI. We are following a large cohort of cognitively normal persons for the outcome of incident MCI; thus, we will be able to test the observation made from the current cross-sectional study. The population-based setting will improve generalizability, and the prospective cohort will strengthen etiologic inferences.
Acknowledgments
The authors express their appreciation to Ms. Stephanie K. Cheung, summer research student from Columbia University, for her help in the final editing of the manuscript.
This study was supported by grants from the NIH (K01 MH68351; AG06786, Mayo CTSA (RR024150 [Career Transition Award]), the RWJ Foundation (Harold Amos Scholar), and from the Robert H. and Clarice Smith and Abigail Van Buren Alzheimer's Disease Research Program.
The authors report no financial conflicts of interest.