Although monoamine dysfunction, particularly of the serotonin (5-HT) system, is the primary neurobiological hypothesis guiding research and treatment of major depressive disorders,
1 emerging evidence suggests that perturbations in sphingolipid metabolism may also be involved. The sphingolipid ceramide is a bioactive signaling lipid that regulates cellular events ranging from proliferation to apoptosis.
2 Ceramides can be rapidly generated via hydrolysis of sphingomyelins by sphingomyelinases. Recent findings have implicated acidic sphingomyelinase (ASM), and its reaction product ceramide, in monoamine function as well as the pathology of depressive disorders. Furthermore, ceramides may alter the function of the dopamine transporter, causing a reduction in dopamine and increase in 5-HT transport into rat striatal synaptosomes.
3 Also, increasing the ceramide content of cell membranes increases the affinity of the 5-HT-1A receptor.
4 In the only clinical study, peripheral blood mononuclear cell ASM activity was increased in subjects with major depression, as compared with healthy volunteers.
5Approximately 25%–30% of people with Alzheimer's disease (AD) are also diagnosed with major depression.
6 Multiple studies have shown that particular forms of ceramide are increased in the brains of people with AD,
7 and results predict memory impairment,
8 and experimental studies have identified pathogenic links between increased ceramide and aberrant amyloid-processing.
7,9 Together, these findings suggest that perturbed sphingolipid metabolism may increase the vulnerability of AD patients to depressive symptoms. The present preliminary study examined whether current or past depression was associated with increased plasma ceramides and whether the increase was greater in AD patients with depressive symptoms.
METHOD
Participants included 25 cognitively normal controls (NC) and 21 Alzheimer's disease (AD) patients recruited from the Johns Hopkins Alzheimer's Disease Research Center and Memory clinics. Participants were ≥55 years of age, had no neurological disease other than AD, and were required to have an informant. NCs had a Clinical Dementia Rating (CDR)
10 of 0; AD patients had a CDR of 1 and met NINCDS/ADRDA criteria for probable AD.
11 The study was approved by the Johns Hopkins University Institutional Review Board.
Participant evaluation included a clinical assessment, medical history, medication inventory, neuropsychological examination, and blood draw. Major depression was assessed via self- and informant-report of clinically-diagnosed recent depression (major depression within 2 years), past depression (last episode >2 years ago), or no major depression.
Non-fasting blood was drawn, and plasma was isolated and frozen at –80°C until processing. Sphingolipids were extracted as previously described,
12 and detected and quantified by LC/MS/MS, using multiple reaction monitoring (MRM).
Ceramide measurements were log-transformed and examined as continuous variables in units of counts per second (cps), a quantification of area under the curve, commonly used for sphingolipid assays. Group differences in plasma lipids were first examined with ANOVAs, and subsequent pairwise associations with t-tests. Effect size was examined with Cohen's δ. The a priori p value was set at p<0.05. All analyses were conducted with SPSS Version 16.0.
RESULTS
A total of 15 participants (5 NC and 10 AD) reported Recent Depression, 8 (4 NC and 4 AD) reported Past Depression, and 23 (16 NC and 7 AD) had no current or past history of depression (No Depression). Given that results between plasma ceramides and depression were the same, and there were no differences in mean ceramide levels between NC and AD, the two groups were combined.
The mean age of the sample was 74.6 (standard deviation [SD]: 6.9) years, and mean education level was 15.8 (SD: 3.2) years; 20 (43.5%) were women. On the basis of the General Health Medical Rating (GHMR) Scale, the majority of participants (80.0%) had “Excellent” health, and the others (20.0%) had “Good” health. Half (50.0%) of the sample were diagnosed with hypertension, 6.5% with angina, and 10.9% with diabetes mellitus. There were no differences between NC and AD patients with regard to age, education, or other health-related characteristics (p<0.05). The mean Mini-Mental State Exam (MMSE) score for the NC group was 28.8 (SD: 1.2), and for the AD group was 22.2 (SD: 3.1); 19 of the 21 AD patients (90.4%) were taking cholinesterase inhibitors or memantine at baseline; 14 participants (93.3%) with Recent Depression, 5 (62.5%) with Past Depression, and 0 with No Depression were taking antidepressants; all but 1 of these were taking selective serotonin reuptake inhibitors (SSRIs). There were no differences in age, gender, education, or health-related characteristics, including hypertension, hypercholesterolemia, or diabetes by Depression status (p<0.05).
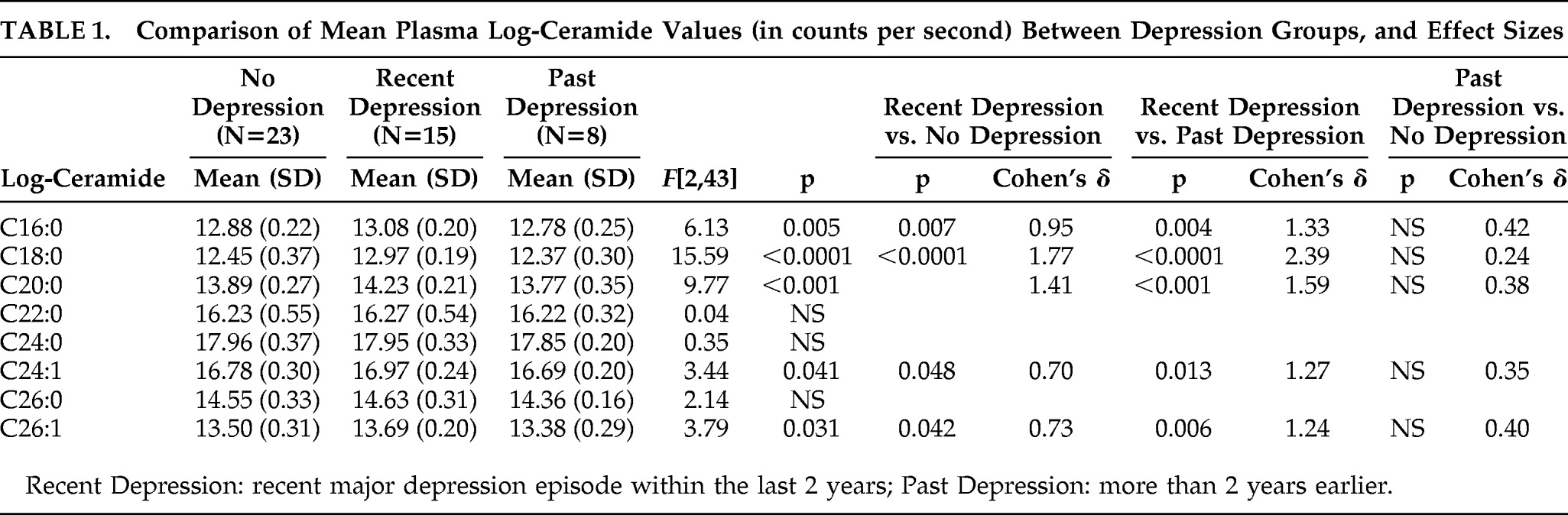
Plasma ceramides C16:0, C18:0, C20:0, C24:1, and C26:1, but
not C22:0 or C24:0 varied by Depression group (p<0.05;
Table 1). Examining pairwise associations, participants with Recent Depression had higher mean-log ceramide levels of C16:0, C18:0, C20:0, C24:1, and C26:1, than those with No Depression or Past Depression (p<0.05;
Table 1). Effect sizes for significant pairwise associations were large, ranging from 0.73 to 2.39. Mean ceramide levels did not differ between the No Depression and Past Depression groups. There was also no correlation between plasma ceramide levels and Geriatric Depression Scale (GDS) score across or within each Depression group. Plasma ceramides did not differ by current antidepressant use (p>0.10).
DISCUSSION
Participants with recent major depression (within the previous 2 years), had higher plasma levels of ceramide C16:0, C18:0, C20:0, C24:1, and C26:1 than subjects with a past (last episode more than 2 years ago) or no history of major depression. This increase was observed both in individuals with normal cognition and those with AD. Effect sizes were large.
These results are consistent with a previous clinical study that examined ceramide metabolism in depression and found higher ASM activity (which leads to higher ceramide levels) in peripheral blood mononuclear cells of patients with major depression versus controls.
5 In combination with our current findings, these data suggest that peripheral measures of sphingolipid metabolism may be useful indicators of current depression. Although the role of ceramides in the pathogenesis of depression remains to be elucidated, an increase in the ceramide content of cell membranes can perturb monoaminergic transport across the cell membrane and alter 5HT
1A affinity for 5-HT.
3,4 It has been suggested that ceramides may be responsible for the therapeutic latency of antidepressants.
13 Also, ceramides increase the activity of phospholipase
A2,
14 which has been reported to be elevated in major depression.
15Findings from cellular and animal studies suggest that antidepressant drugs may regulate ceramide levels. Treatment with imipramine and amitriptyline decreased ASM activity in cultured cells,
5 suggesting that these antidepressants may decrease ceramide levels. The effects of antidepressants on plasma ceramides were not directly measured in the present study because all but one participant in the Recent Depression group were taking antidepressants. Plasma ceramide levels in the Past Depression group did not differ between the five subjects taking an antidepressant and the three subjects who were not, but the sample sizes are too small to draw a conclusion.
The major limitation of this study is that the diagnosis of depression was by self- and informant-report of a physician's diagnosis, rather than with validated diagnostic instruments. Another limitation is the small sample size, although effect sizes were statistically significant and quite large regardless of the sample size. Last, the Recent Depression group included those diagnosed within 2 years, some of whom may have remitted. Despite this limitation, however, there were still significant differences in plasma ceramides between those with Recent Depression and those with Past Depression. One explanation for these findings is that subjects in the Recent Depression group are still in a “depressive state,” and once the depression has completely remitted, as in the Past Depression group, plasma ceramide levels return to normal. Future research will need to examine plasma ceramide levels or ASM activity over the course of major depression. Such an approach will allow us to understand the relationship between plasma ceramide levels or ASM activity to affective symptoms and cognitive dysfunction.
In summary, these findings support a potential role for dysregulated ceramide metabolism in the pathogenesis of depressive disorders. Additional research to identify the mechanisms by which ceramide metabolism contributes to pathogenesis may lead to the identification of new therapeutic targets to treat depressive disorders.
Acknowledgments
The abstract of this work was presented at the 2009 Annual Meeting of the International College of Geriatric Psychoneuropharmacology, Baltimore, MD.
This research was supported by National Institute on Aging grants R21AG028754, K08AG029157-01A1, and 2P50AG005146-22A1, and by National Institute of Neurological Disorders and Stroke Grant R21NS060271-01 and grants from GlaxoSmithKline and the George and Cynthia Mitchell Fund. All authors report no conflicts of interest. Although funding for this study was partially obtained through a grant from GlaxoSmithKline, the authors had access to the data at all times and retain the data. Funding for the plasma lipids were obtained from NIH grants. All authors report no conflicts of interests with regard to GlaxoSmithKline or any other organization.