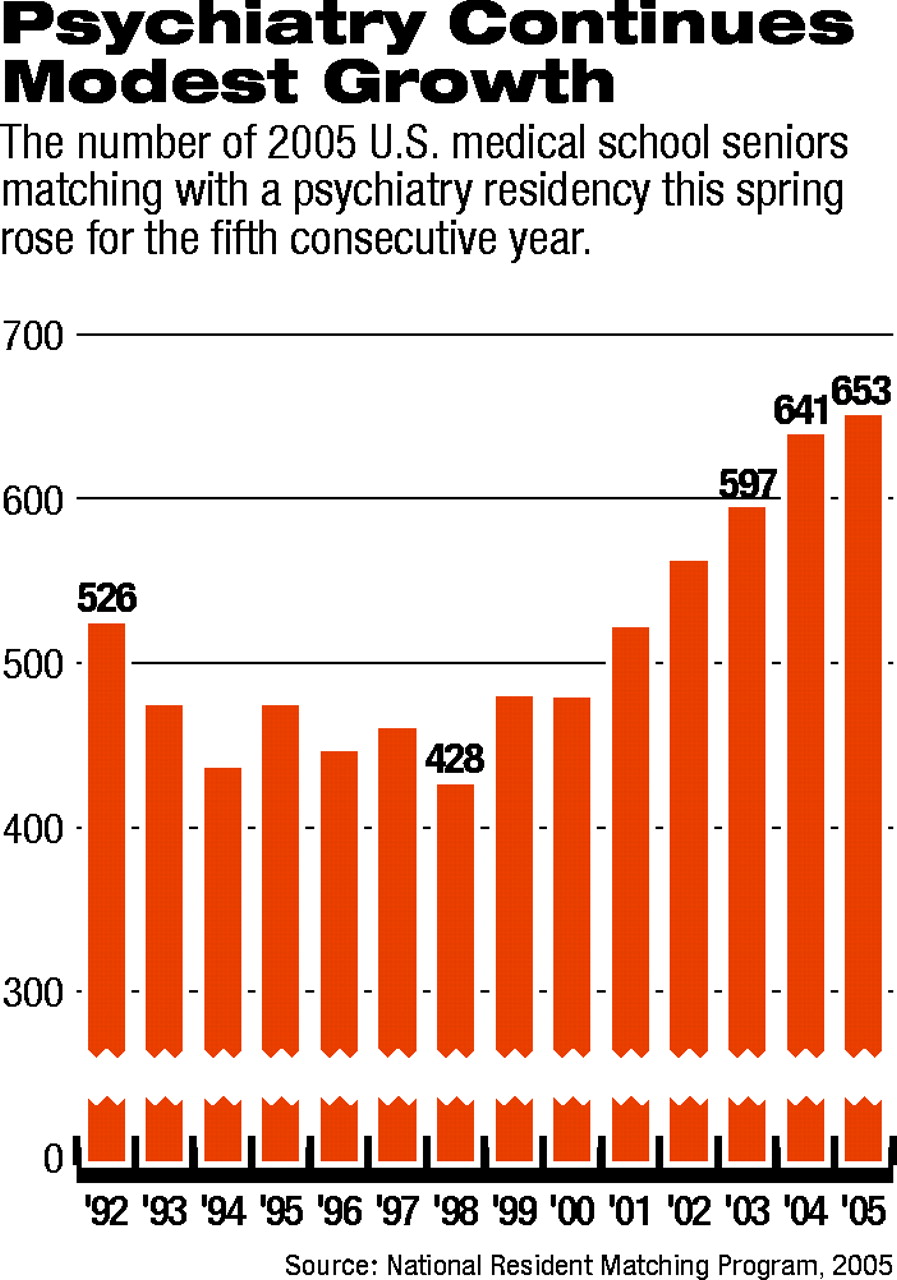
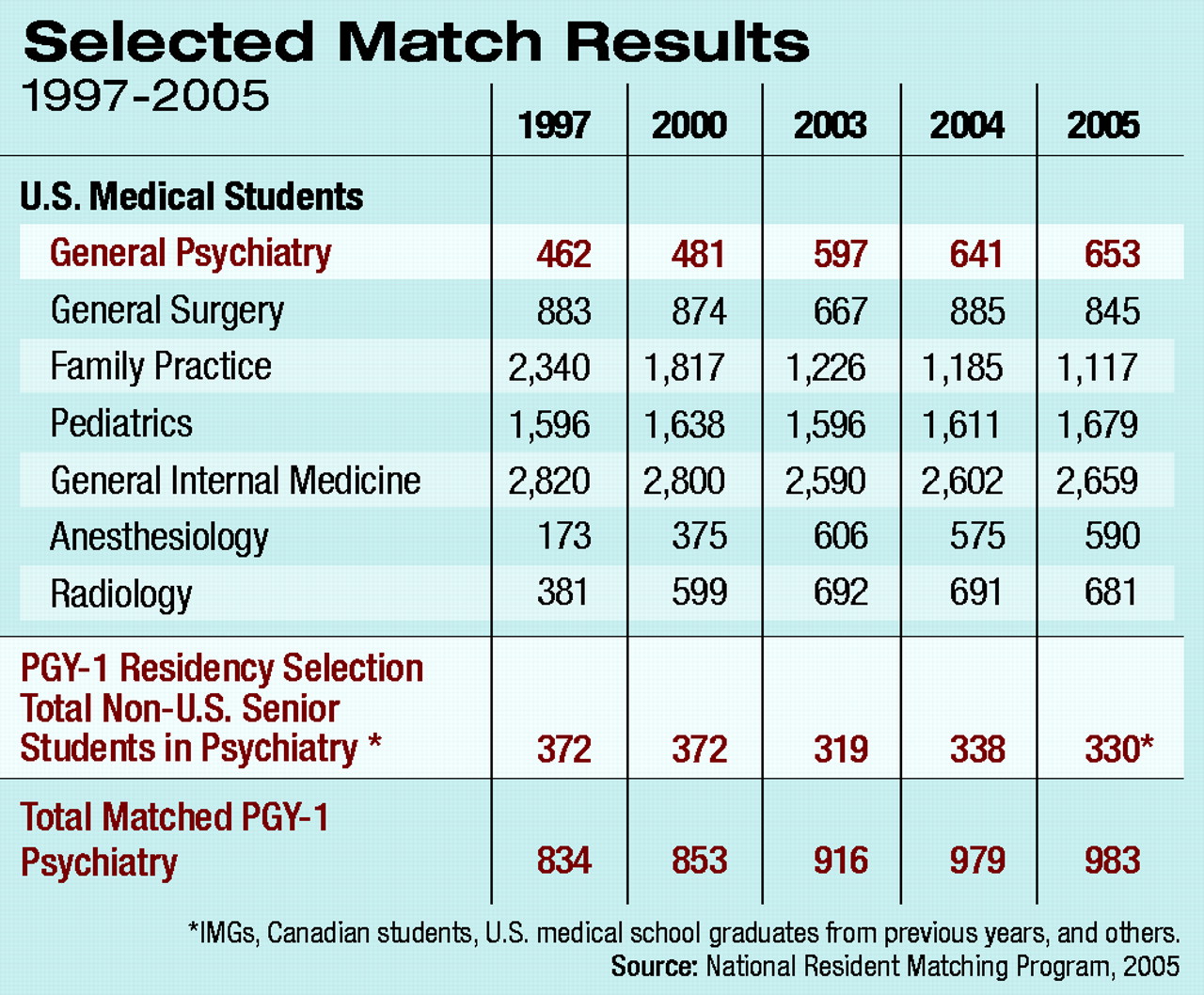
The number of U.S. medical school graduates choosing to enter a psychiatry residency has risen slightly for the fifth year in a row. A total of 653 U.S. medical graduates “matched” into psychiatry residency programs around the country in the annual National Resident Matching Program (NRMP). That figure is up from 641 last year and 597 in 2003 (see chart).
In addition to the 653 U.S. medical graduates, 330 students—including mostly international medical graduates (IMGs), Canadian students, and U.S. seniors who had graduated in previous years—also filled slots this year, for a total of 983 students scheduled to enter PGY-1 general psychiatry residency positions this summer.
“Since 2000, psychiatry has seen a slow and steady increase in our match numbers every year,” said Deborah Hales, M.D., director of APA's Division of Education and Career Development. “I believe there are several trends behind this increase. First, the scientific advances in neurosciences and progress in understanding and treating mental illness make psychiatry an exciting career choice.
“Second, psychiatry offers physicians a controlled lifestyle, where the individual determines his or her own schedule, which is very attractive to medical students today.
“And last but not least, psychiatry is still the specialty where doctors have a significant relationship with their patients and are able to spend time with them, and this too is something valuable when choosing a career.”
Sidney Weissman, M.D., APA's Area 4 trustee and a past president of the American Association of Directors of Psychiatric Residency Training, told Psychiatric News that the modest increase in the number of students entering psychiatry also reflects a continued shift away from primary care that began at the end of the 1990s. Earlier in that decade there had been a rapid increase in the number of students entering family practice and related primary care fields, when health policy experts were predicting that primary care physicians would be the gatekeepers of a new, highly managed American health care system.
Public backlash against managed care and a widespread perception that managed care had fallen far short of its promise, along with physician dissatisfaction with the role of gatekeeper, caused the trend to reverse. In the last five years students have been returning to specialty practice, including some fields—such as anesthesiology and radiology—that had at one time been considered moribund.
“The match this year appears to have consolidated the career shifts of students that began at the end of the last decade,” said Weissman, professor and director of psychiatry residency training at the Feinberg School of Medicine at Northwestern University. “From 1997 until today, 1,200 fewer U.S. seniors are selecting family practice. In the same period, our recruitment of U.S. seniors into psychiatry has increased by nearly 50 percent.
“We can understand the career choice of U.S. seniors in the past seven years as a movement away from family practice with more than 1,000 students now filling positions in a diverse fields, including diagnostic radiology, anesthesiology, emergency medicine, and psychiatry.”
Weissman has maintained a longtime interest in psychiatric workforce issues and provided Psychiatric News with data on the match this year specific to psychiatry, which includes information from the NRMP.
The NRMP is a private, not-for-profit organization established in 1952 to provide “an orderly and fair mechanism” to match the preferences of applicants to U.S. residency positions with the preferences of residency program directors for those applicants. The NRMP is sponsored by the American Board of Medical Specialties, the AMA, the Association of American Medical Colleges, the American Hospital Association, and the Council of Medical Specialty Societies.
Because the match results reflect the fields of medicine preferred by tomorrow's doctors, they are watched like tea leaves by medical educators and policymakers. And while psychiatry has benefited from the return of students to specialty medicine, said Weissman, that shift is likely to level off pitting psychiatry in a “fierce competition” with other specialties for students.
As in past years, Weissman stressed that the profession's own self-definition—what the nature of psychiatric practice will be in the future—is crucial to attracting students.
“In mapping psychiatry's recruitment strategy for the second half of this decade, we will be competing not with family practice for residents, but against varied medical specialties,” he said. “We must ensure that students know what psychiatry is, what the requisite skill sets are to become a psychiatrist, and what practice opportunities exist in diverse settings after completing training.”
Weissman noted also that psychiatry—like the rest of medicine—is heavily dependent on international medical graduates and will remain so for the future.
“American medicine is dependent upon IMGs to fill one-fifth of all residency training positions,” he said. “This reliance will continue for many years to come. For the foreseeable future, approximately a third of psychiatry's residents will be IMGs.”
Information about the NRMP and 2005 match results is posted online at<www.nrmp.org/>.▪