Psychotherapy is emerging in randomized, controlled trials within the last year as the most effective treatment for borderline personality disorder (BPD).
Several forms of psychotherapy— including dialectical-behavioral therapy (DBT), cognitive-behavioral therapy (CBT), transference-focused therapy, and mentalization-based therapy—have been found effective for BPD and have been or are being replicated.
All of the psychotherapies proving successful for BPD strive to address underlying deficits in the ability of patients to relate to others and manage emotions, longstanding problems that are typically rooted in childhood experience.
In 2006 effectiveness of DBT was replicated in a study in the July 2006 Archives of General Psychiatry, and transference-focused therapy was proven effective in a study published in the February 2006 Journal of Clinical Psychology. A replication of early studies of mentalization-focused therapy is ongoing in an outpatient setting.
Schema therapy, the newest innovation integrating elements of several psychotherapies for BPD, was found highly effective in a first randomized, controlled trial, reported in the August 2006 Archives of General Psychiatry.
Experts say the new crop of trials has propelled the field into the era of evidence-based medicine.
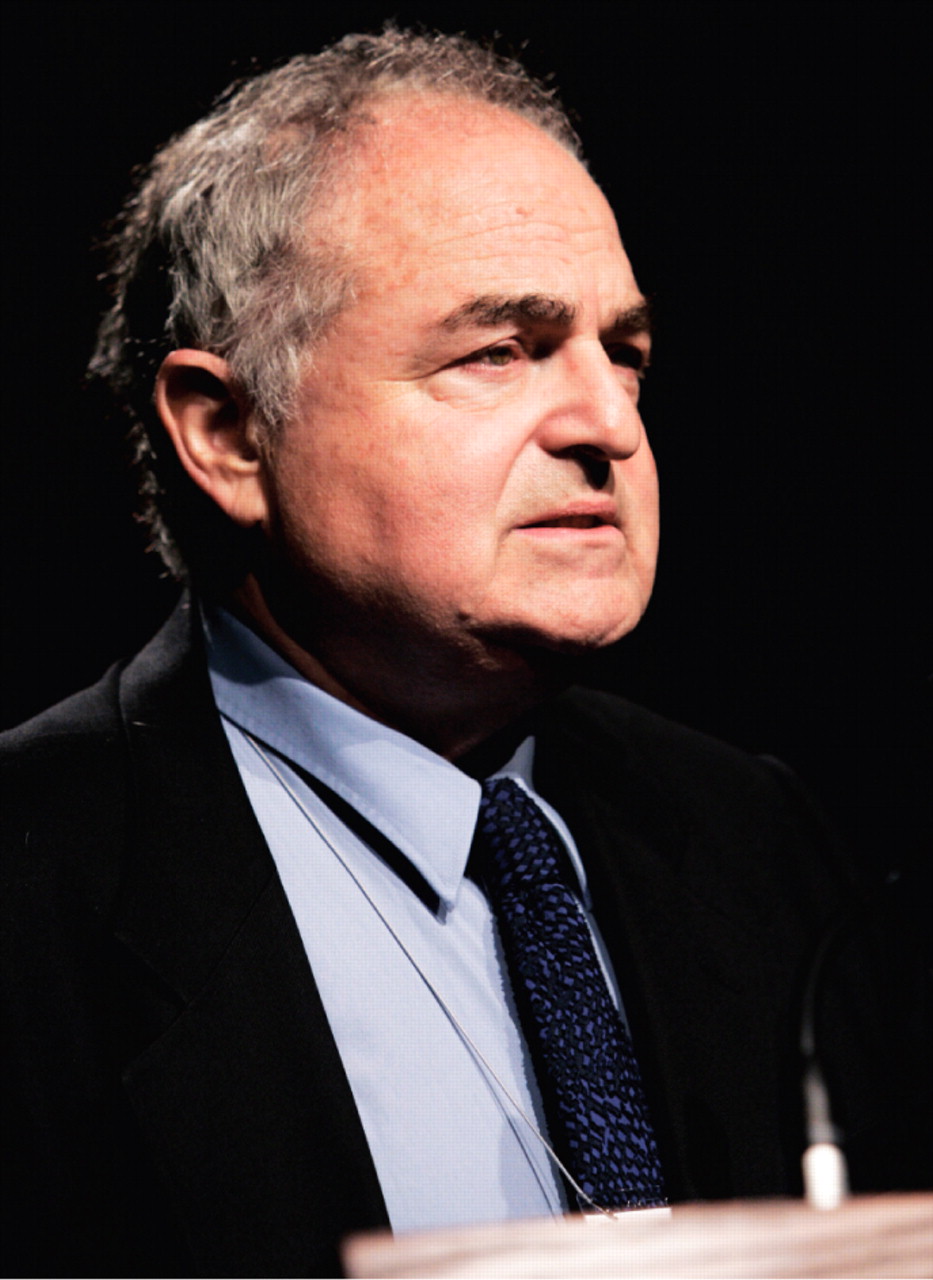
“The field is coming into its own because we are doing randomized, controlled trials to determine what actually works,” Joel Paris, M.D., told Psychiatric News. “In the past we were dependent on the charisma of therapeutic gurus.”
Paris is a professor and chair of the Department of Psychiatry at McGill University in Montreal and editor in chief of the Canadian Journal of Psychiatry. He is also a past president of the Association for Research in Personality Disorders.
He said there is no consensus about whether one therapy is any better than the others, though DBT has been around the longest and is widely taught.
“Most patients are probably receiving a mix of eclectic therapies,” Paris said.
DBT Targets Dangerous Behaviors
In the July Archives report on DBT, patients received either DBT or treatment by community experts. The latter were therapists who were experienced in the treatment of BPD but used methods other than DBT to treat randomly assigned patients.
Subjects receiving DBT were half as likely to make a suicide attempt, required fewer hospitalizations for suicide ideation, and had lower medical risk across all suicide attempts and self-injurious acts combined. They were also less likely to drop out of treatment and had fewer psychiatric hospitalizations and psychiatric emergency department visits, according to the report.
Developed by Marcia Linehan, Ph.D., of the Department of Psychology at the University of Washington, DBT directly targets suicidal and other dangerous, severe, or destabilizing behaviors. Standard DBT strives to increase behavioral capabilities, improve motivation for skillful behavior through management of issues and problems as they come up in day-to-day life and reduction of interfering emotions and cognitions, and structure the treatment environment so that it reinforces functional rather than dysfunctional behaviors.
Therapy consists of weekly individual psychotherapy, group skills training, telephone consultation, and weekly meetings between therapist and a consultation team to enhance therapist motivation and skills and to provide therapy for the therapists.
Mentalization-based therapy, pioneered by Andrew Bateman, M.A., and Peter Fonagy, Ph.D., seeks to facilitate the capacity for“ mentalization”—the ability to perceive the mind of others as distinct from one's own and hence to reconsider and reassess one's own perceptions of reality. Transference-focused psychotherapy, championed by Otto Kernberg, M.D., among others, is an adaptation of psychoanalysis that aims to correct distortions in the patient's perception of significant others and of the therapist.
Schema Therapy Builds on CBT
Schema therapy, the newest of the psychotherapies for BPD, appears to synthesize elements of several successful therapies. Paris has described it as“ CBT with a psychodynamic component.”
Schema therapy founder Jeffrey Young, Ph.D., who is on the faculty of the Department of Psychiatry at Columbia University College of Physicians and Surgeons, was one of the first students of Aaron Beck, M.D., the founder of cognitive therapy.
“I found that cognitive therapy was extremely effective with many Axis I disorders, as research has since substantiated, but was much less effective by itself with Axis II personality disorders,” he told Psychiatric News. “I began to look for ways to expand cognitive-behavior therapy to work with Axis II issues by integrating elements drawn from other approaches as well as CBT, including psychodynamic therapies such as object relations, emotion-focused/gestalt therapies, and attachment theory.”
Young described schema therapy as an active, structured therapy for assessing and changing deep-rooted psychological problems by looking at repetitive life patterns and core life themes, called “schemas.” Schema therapists use an inventory to assess the schemas that cause persistent problems in a patient's life.
“Once we have determined what schemas a patient has, we use a range of techniques for changing these schemas,” Young said. “These include cognitive restructuring, limited re-parenting, changing schemas as they arise in the therapy relationship, intensive imagery work to access and change the source of schemas, and creating dialogues between the `schema,' or dysfunctional, side of patients and the healthy side.”
He added that systematic behavioral techniques are also employed to change dysfunctional coping styles, especially maladaptive behaviors in intimate relationships.
More information about schema therapy is posted at<www.schematherapy.com>.
In a randomized trial of schema therapy versus transference-focused therapy published in the Archives in June 2006, statistically and clinically significant improvements were found for both treatments on all measures after one, two, and three-year treatment periods. Data on 44 schema therapy patients and 42 transference-focused therapy patients were available.
Main outcome measures included scores on the Borderline Personality Disorder Severity Index, quality of life, and general psychopat hologic dysf unction. Patient assessments were made before randomization and then every three months for three years.
Significantly more schema therapy patients fully recovered (46 percent versus 26 percent) or showed reliable clinical improvement (66 percent versus 33 percent) on the Borderline Personality Disorder Severity Index than patients receiving transference-focused therapy. They also improved more in general psychopathologic dysfunction and showed greater increases in quality of life.
Statistical analysis also revealed a higher dropout risk among transference-focused therapy (52 percent) patients than among patients receiving schema therapy (29 percent), according to the study report.
“This is the first controlled study demonstrating that a treatment is capable of reducing all of the BPD manifestations as defined by DSM-IV, reduces associated personality features and general psychopathology, and increases quality of life,” study co-author Arnoud Arntz, Ph.D., told Psychiatric News.
He is with the Department of Medical, Clinical, and Experimental Psychology at the University of Maastricht, in the Netherlands.
The authors also stated that, in a separate analysis, schema therapy was found to be highly cost-effective for society, despite the length and intensity of the treatment.
Young, who was not involved in the study, said it is the first to demonstrate “deep personality change” in a high percentage of patients long considered untreatable.
“Up until now, existing therapies for BPD have proven to lead to only partial recovery or have only been able to reduce self-harming behaviors,” he said. “This should be of great interest to psychiatrists because patients with BPD are usually considered the most difficult, frustrating, and risky patients within most therapists' practices.
“The second important implication for psychiatrists is that the use of a neutral stance toward the BPD patient, which is advocated in most psychody namic approaches to BPD, is clearly much less effective than the more engaged, warm, and nurturing stance of schema therapy,” Young said.“ This was demonstrated by the dramatic differences in dropout rates between the two treatments.”
Despite their proven effectiveness, all of the psychotherapies for BPD are time and labor intensive.
“All suffer from the need for highly trained therapists, specialized settings, human resources, and time,” Paris told Psychiatric News. “There are many barriers to psychotherapy for BPD. Most involve money, since only a small number of these patients can pay, and few have adequate insurance. Another barrier is the failure of psychiatrists and other professionals to recognize and diagnose BPD. Still another is the current tendency to treat BPD with medication alone.”
Paris said in an address at APA's annual meeting last year in Toronto that drugs were vastly overused in treatment of all the personality disorders (Psychiatric News, July 7, 2006).
“The problem is that there is no science to support polypharmacy, and it's probably bad for patients,” he said at the meeting. “When you give patients with classical depression an antidepressant, they may be cured in a few weeks. But you never see that in patients with borderline personality. It might take the edge off, but patients never go into remission.” ▪