Psychiatrist Linda Chaudron, M.D., M.S., runs a perinatal clinic at the University of Rochester Medical Center, where some of the new mothers she sees are taking psychotropic drugs.
Deciding whether a breastfeeding mother should remain on a particular medication, stop using it, or switch to another, presumably safer, drug is no simple matter. For a start, while some of Chaudron's clinic patients have planned for pregnancy and breastfeeding, others have become pregnant with little knowledge of how the drugs they are taking might affect their fetus or infant, Chaudron told Psychiatric News.
Chaudron, who has been studying the effects of psychiatric medications used while a mother is breastfeeding, is an associate professor of psychiatry and obstetrics and gynecology and associate chair for clinical services at the University of Rochester School of Medicine. She is a coauthor of the recent joint report from APA and the American College of Obstetricians and Gynecologists (ACOG) on treatment recommendations for depression in pregnant women (Psychiatric News, September 4).
The psychiatrists, pediatricians, and ob/gyns who care for mothers and their infants all need guidance on the risks of maternal medications during breastfeeding, but data can be hard to find, she said.
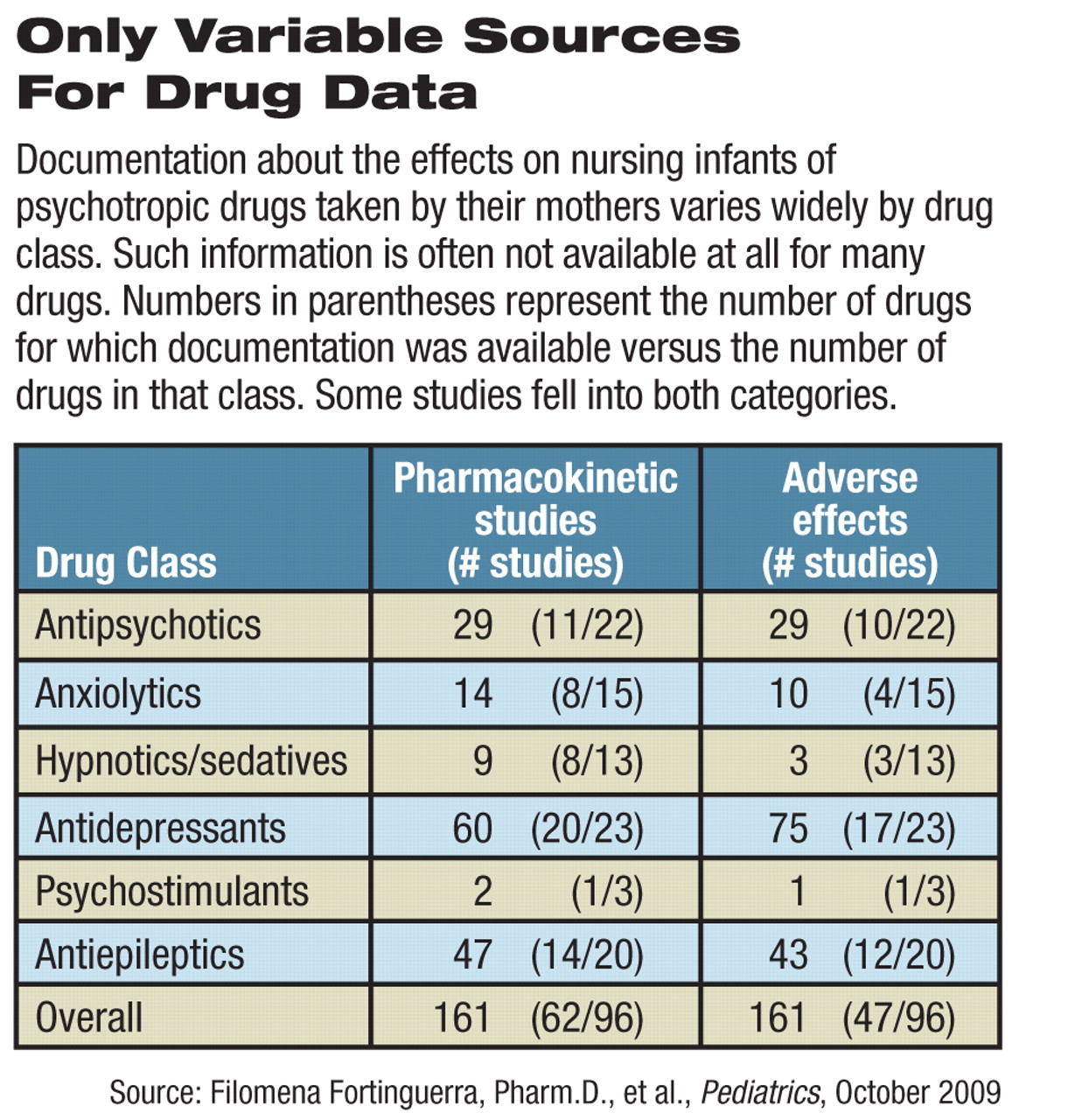
Use of psychotropic drugs during breastfeeding is supported by evidence-based research for less than one-third of such medications for which information was available, according to a review of four decades of medical literature in the October Pediatrics.
Despite efforts worldwide to promote breastfeeding of infants, little is known about the excretion of psychotropic drugs in breast milk or adverse effects on nursing babies, wrote Filomena Fortinguerra, Pharm.D., Antonio Clavenna, M.D., and Maurizio Bonati, M.D., of the Laboratory for Mother and Child Health in the Public Health Department of the Mario Negri Institute for Pharmacological Research in Milan, Italy.
Nursing women are often confused or anxious about using these medications, and often will stop using them or stop breastfeeding. Balancing drug risk to an infant against the potential harms of untreated mental illness is difficult.
Product-information data sheets offer little help in solving that dilemma. They frequently say that the drug should not be used during lactation or that breastfeeding should be discontinued, wrote the authors.
“The warnings are not necessarily related to observed or reported adverse effects,” they said. “They are often used as a defensive measure on the part of the manufacturer when the drug's safety information is not available.”
The Italian researchers searched Medline, Embase, and PsychINFO for studies published from 1967 through July 2008 on 96 selected psychotropic drugs. They found no documentation for 34 of those drugs. Of the remaining 62 medications (found in 183 original articles), there was evidence to back the use of only 19 (31 percent) among lactating women. SSRI antidepressants and antiepileptics appear to be the best-studied classes of drugs. Some of the drugs they include are used in Europe, but not in the United States.
The study considered factors such as maternal drug dosage, the ratio of the concentration of the drug in the mother's milk to that in her plasma, the fraction of the mother's dose that the baby ingested, and the incidence of adverse effects to the infants.
Each drug has to be considered individually, said the authors, because“ there are documented differences between drugs within the same class, and there is no class action in relation to breastfeeding.”
Drugs within each therapeutic category that result in minimal exposure to the infant should be considered as first choices for breastfeeding mothers.
For instance, among the 20 antidepressants reviewed, sertraline, paroxetine, and fluvoxamine are the first choices to prescribe, in the authors' opinion. Citalopram, escitalopram, and fluoxetine, in contrast, are contraindicated during lactation because of the relatively high amounts ingested by infants, the reported adverse effects in infants, and their long half-life. Too few extended studies of SSRIs are available to judge any long-term neurobehavioral effects.
Chlorpromazine and olanzapine could be considered first-choice drugs among antipsychotics, while clozapine, lithium, and sulpiride are contraindicated, wrote Fortinguerra, Clavenna, and Bonati.
“Because psychosis requires long-term treatment and because the data on safety of antipsychotics during lactation are limited, the benefits of breastfeeding may be weighed against the potential risks of medication,” they added.
There are few data available on the effects of hypnotics and anxiolytics on neonates, but long-acting benzodiazepines should be ruled out and infants monitored for sedation, nausea, or poor feeding.
The authors noted several points based on their analysis. Valproic acid and carbamazepine are the preferred medications for epilepsy during breastfeeding. Ethosuximide, phenobarbital, lamotrigine, primidone, topiramate, and zonisamide are contraindicated, because of reported adverse effects in infants and the relatively high dosage delivered to them in breast milk.
Only three mother-baby pairs have been included in studies of methylphenidate, the only psychostimulant studied, so it is not possible to evaluate its safety in nursing infants.
“This is a nice overview for psychiatrists, pediatricians, and ob/gyns to refer to about safety issues, but it shows how little information is out there,” said Chaudron.
Even with the help of the data in the Pediatrics article, care for breast-fed infants requires close cooperation among the patient and all of the medical providers working with her and her child, said Chaudron.
The APA and ACOG joint report in August recommended that women with depression discuss their diagnosis and treatment with their ob/gyn and their psychiatrist and that these physicians later consult closely with each other.
They should be aware that the mother is both breastfeeding and taking psychotropic drugs and explore the risks and benefits of all options.
“But if the mother is stable on a given medication, my advice is to go with what is known,” she said. “It's hard to recommend a change if something is working.”